Figures & data
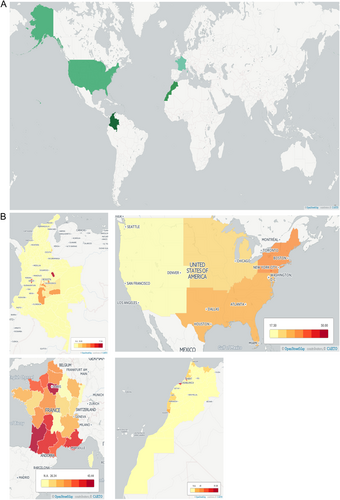
a Countries compared herein are highlighted. Across our countries of interest, there is significant variation in seroprevalence, with the United States having the lowest overall seroprevalence and Colombia having the highest. Contributing factors to this variation must include exposure to oocysts from cats and contaminated meat. Factors that influence these exposures include climate, host behaviors, and public health infrastructure. b There is regional variation within countries. In Colombia, there is significant variation that correlates with annual rainfall, which is associated with oocyst survival and with oocysts contaminating the environmentCitation55. Regions without seroprevalence data available are marked N.A. (no data available), while increasing rates of seroprevalence are indicated by darkening of the shading of the region. Seroprevalence data for the generation of these maps were obtained from several sourcesCitation40,Citation41,Citation47,Citation49,Citation55. Maps were generated with Carto
Manifestations of ocular disease are common in congenital toxoplasmosis. However, the disease can be quite severe, and patients from Morocco, shown here, demonstrate significant severe cases. a Severe hydrocephalus can occur due to inflammation preventing resorption of cerebrospinal fluid (CSF) or obstructing flow of cerebrospinal fluid (CSF). This child was admitted to the Hôpital des Spécialités in Rabat, Morocco, and unfortunately did not survive due to the severity of his illness. b Ocular involvement is also common in congenital toxoplasmosis. Substantial scarring of the retina is also possible, and disruption of the retina can lead to loss of sight. c Progression of an ocular lesion in a congenitally infected 19-year-old patient. Ocular lesions progress without adequate treatment and can involve the formation of subretinal fluid and choroidal neovascular membranes (observed using optical coherence tomography)
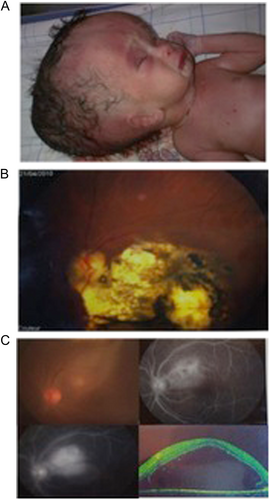
Congenital toxoplasmosis in Morocco
The geographic distribution of cases of congenital toxoplasmosis in a cohort of patients identified by Pr. Barkat are presented here and occurred across three distinct climate and cultural zones. The ocean region encompasses Rabat and Dakhla (indicated in red). The mountain region includes Khénifra, Midelt, and Tinghir (indicated in yellow), whereas the region of the Sahara includes Errachidia (indicated in green). Although the sample size is small, with only 21 cases of severe congenital toxoplasmosis, it is suggestive of the possibility that there is a geographic variation in the rates of this parasitic infection, potentially attributable to differences in climate or risk behaviors

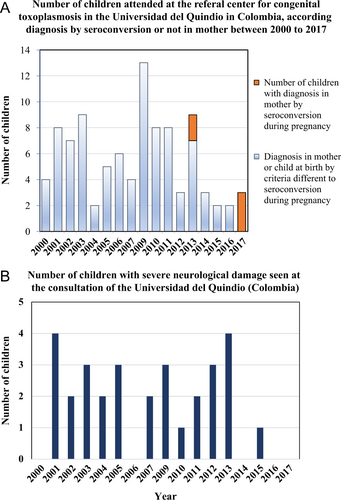
a Before 2013, when evidence-based guidelines for congenital toxoplasmosis were implemented, no cases based on seroconversion criteria presented for clinical consultation for congenital toxoplasmosis at the University of Quindio; after that date, three new cases were discovered by the monthly follow-up of mothers for the development of anti-Toxoplasma IgM antibodies. The congenital infection in children was confirmed by postnatal monthly serological follow-up. Children had prenatal treatment and had congenital infection that was asymptomatic. In 2017, only cases based on seroconversion diagnostic criteria were received, with none diagnosed at birth with severe disease, as is often the case in countries without systematic screening. b Before 2013, 2–6 cases of congenital toxoplasmosis with severe neurological damage (hydrocephalus or hydranencephaly) were identified annually at the Universidad del Quindio. After 2013, the only case that presented with severe neurological sequelae was an indigenous baby whose mother, for cultural reasons, did not participate in the prenatal screening program. There is a significant difference between the percentage of children seen with severe neurological damage in 2013 or earlier compared with after 2013 using Fisher’s exact test (29/65 = 44.6% vs. 1/10 = 10%, p = 0.04)
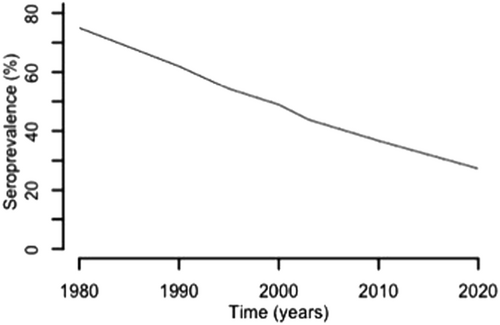
According to the French data collected over the last several decades, the seroprevalence for antibodies specific to T. gondii has decreased markedlyCitation72. In this graph, the seroprevalence data for 30-year-old women decreased over time, which is likely due to changes in risk behaviors influenced by educational programs as well as gestational screening. This downward trend in frequency is projected to decrease even further in the coming years. Decreasing disease severity in congenitally infected infants over this period has also been noted
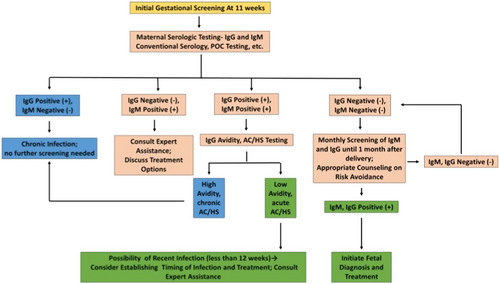
A gestational screening algorithm, identifying those patients who ultimately require no treatment (blue), those who require additional testing (pink), and those for whom treatment should be strongly considered (green). This algorithm can be applied in any setting with basic laboratory capabilities, though avidity and AC/HS is more complex. In these settings, given the benign treatment profile of spiramycin, it might be appropriate to err on the side of treatment of these patients without further testing. The AC/HS test is a differential agglutination test using the ratio of two antigens present predominantly in early (AC) and late (HS) T. gondii infection to suggest the timing of infection. It is critical to note that this algorithm should only be utilized for pregnant women presenting for care during the specified time period. For those presenting at different times in gestation for care, testing and treatment protocols are more nuanced. Refer to work from the Palo Alto Reference Laboratory or papers on the management of congenital toxoplasmosis for further details regarding the screening protocolCitation8,Citation13