Figures & data
Figure 1. Ultrasound features of typical AVF lesions.
(A) Type intima-dominant. Intimal hyperplasia at the proximal vein: distance shows the thickness of the intima (1.5 mm), and the minimum luminal diameter is 1.3 mm. The PSV at the stenosis site is 567 cm/s. (B) Type Non-intima-dominant: distance shows the thickness of intima (0.3 mm), and minimum luminal diameter is 1.7 mm. The PSV at the stenosis site is 592 cm/s. (C) Type Valve obstruction (In color mode). The valve is stiff, and the lead vascular lumen shows severe stenosis. The minimum luminal diameter is 1.0 mm. The white curved arrow points to the stiff valve. The PSV at the stenosis site is 534 cm/s. (D) Type vascular calcification. Vein calcification at venous outflow near the anastomosis, and the minimum luminal diameter is 0.8 mm. The PSV at the stenosis site is 511 cm/s. Sheet-like calcified plaques break into the lumen of the vessel and are hyperechoic. The white straight arrows point to calcified plaques. The border between intima and lumen is marked on the figures as dotted lines, * residual lumen, + intima. AVF: arterial-venous fistula; PSV: peak systolic velocity.
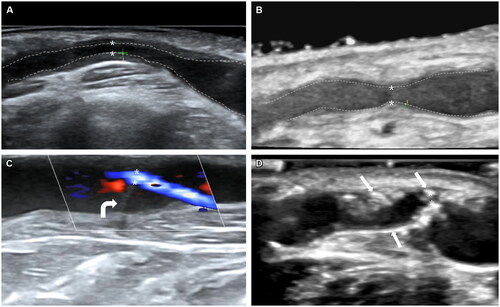
Table 1. Baseline demographics, clinical, and laboratory examination characteristics of all 185 patients in the cohort.
Table 2. Ultrasound characteristics of different AVF lesion types (n = 185).
Figure 2. Kaplan–Meier survival analysis of AVF primary patency after PTA.
(A) Kaplan–Meier survival analysis of the type of AVF stenosis location on AVF primary patency after PTA; (B) Kaplan–Meier survival analysis of the type of ultrasound appearance on AVF primary patency after PTA; type I: stenosis near the anastomosis; type II: stenosis in the region of the draining vein, particularly in the area of the puncture; type III: stenosis in the venous confluence site or the central vein, particularly in the region of the cephalo-axillary vein or the cephalic arch); mixed type: AVF with two or more types of stenosis. AVF: Arterial-venous fistula; PTA: percutaneous transluminal angioplasty.
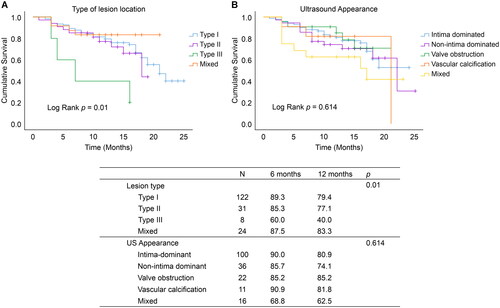
Table 3. Multivariate Cox regression model of factors predicting post-intervention primary patency of AVF in patients receiving HD (n = 185).
Data availability statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
PTA times indicates the number of times patients are treated with PTA for AVF dysfunction within the life of the AVF.
Data are expressed as mean ± standard deviation for normally distributed measures and as median (interquartile range) for non-normally distributed measures, except where noted. a: Mann–Whitney U non-parameter test; b: Fisher exact probability method is used for comparison.
Data forms are expressed as mean ± standard deviation for normally distributed measures and median for non-normally distributed measures, except where noted; a: Fisher exact probability method is used for comparison.
