Figures & data
Figure 1. Decision points during infertility treatment. GnRH: gonadotropin-releasing hormone; hCG: human chorionic gonadotropin; LH: luteinizing hormone.
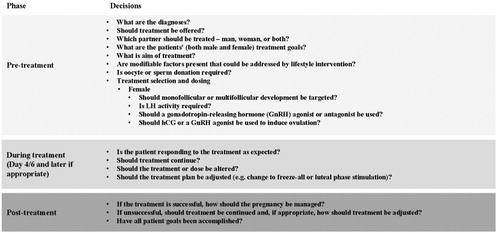
Figure 2. An overview of the treatment of female infertility including the main decision points and treatment suggestions. As infertile women often present with multiple diagnoses and this diagram attempts to segment patient diagnosis to one contributing factor, the suggested treatment may not be most appropriate based on a full diagnosis (e.g. for anovulatory infertility, monofollicular development may not be appropriate if the patient also has tubal factor). ART: assisted reproductive technologies; IUI: intrauterine insemination; OI: ovulation induction; PCOS: polycystic ovary syndrome.
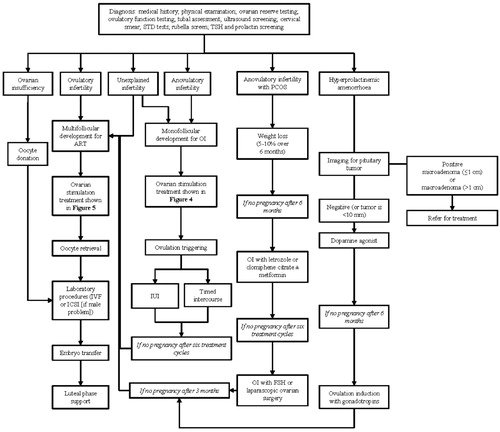
Figure 3. Ovulation induction vs. controlled ovarian (hyper)stimulation. ART: assisted reproductive technologies.
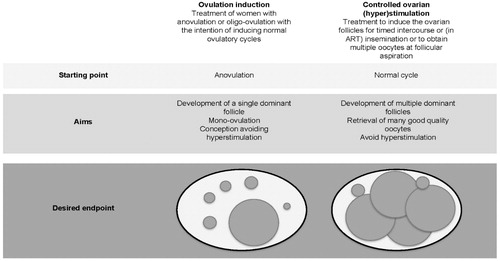
Figure 4. Proposed treatment algorithm for ovulatory infertility. As infertile women often present with multiple diagnoses and this diagram attempts to segment patient diagnosis to one contributing factor, the suggested treatment may not be most appropriate based on a full diagnosis. COS: controlled ovarian stimulation; FSH: follicle-stimulating hormone; GnRH: gonadotropin-releasing hormone; hCG: human chorionic gonadotropin; ICSI: intracytoplasmic sperm injection; IUI: intrauterine insemination; IVF: in vitro fertilization; WHO: World Health Organization.
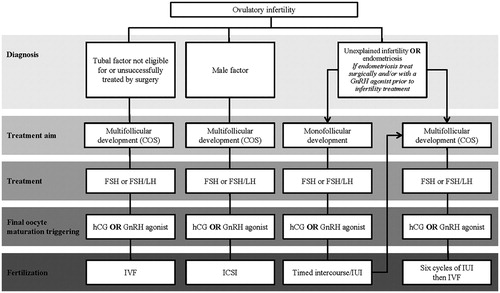
Figure 5. Standard treatment flow for ART treatment. *GnRH antagonist can be used in a flexible or fixed protocol. †If the estradiol level is low in relation to follicles LH supplementation may be considered. If both the estradiol level and follicle count are low, a gonadotropin dose increase should be considered. If the estradiol level is very low, a gonadotropin dose increase should be considered. ‡Additional testing is recommended on day 11 to assess hyperstimulation or premature luteinization. GnRH: gonadotropin-releasing hormone.
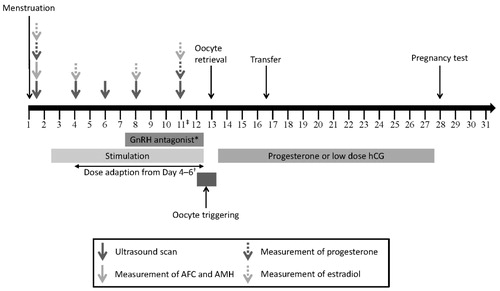
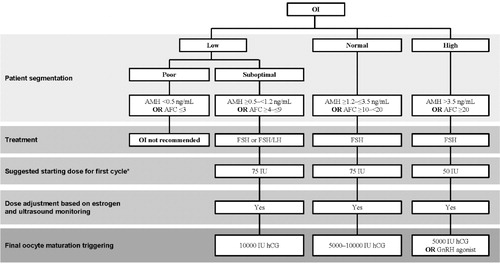
Figure 6. Proposed treatment algorithm for controlled ovarian stimulation according to (predicted) ovarian response. Doses indicated are suggestions, and the dose should be individualized according to all patient characteristics. AFC: antral follicle count; AMH: anti-Müllerian hormone; COS: controlled ovarian stimulation; FSH: follicle-stimulating hormone; GnRH: gonadotropin-releasing hormone; hCG: human chorionic gonadotropin; LH: luteinizing hormone.
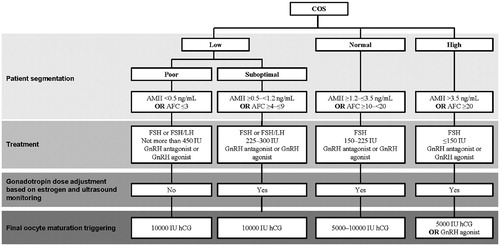
Figure 7. Proposed treatment algorithm for anovulatory infertility. ART: assisted reproductive technologies; CC: clomiphene citrate; COS: controlled ovarian stimulation; GnRH: gonadotropin-releasing hormone; hCG: human chorionic gonadotropin; IUI: intrauterine insemination; LOS: laparoscopic ovarian surgery; OI: ovarian induction; WHO: World Health Organization.
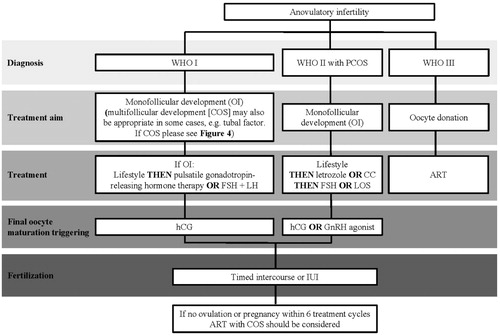
Figure 8. Standard treatment flow for ovulation induction plus IUI/timed intercourse. *If the estradiol level is low in relation to follicles, LH supplementation may be considered. If both the estradiol level and follicle count are low, a gonadotropin dose increase should be considered. If the estradiol level is very low, a gonadotropin dose increase should be considered. †Additional testing is recommended on day 11 to assess hyperstimulation or premature luteinization.
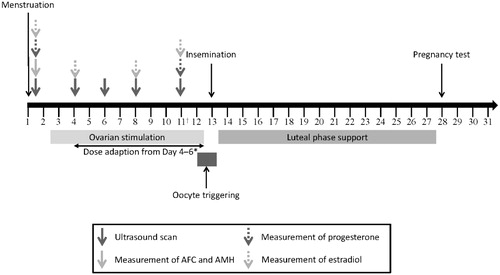
Figure 9. Proposed treatment algorithm for ovulation induction according to (predicted) ovarian response. *The starting dose for subsequent cycles should be selected, taking into account the ovarian response during the previous cycle. AFC: antral follicle count; AMH: anti-Müllerian hormone; hCG: human chorionic gonadotropin; OI: ovulation induction.