Figures & data
Table 1. Advantages and disadvantages of standard oral and topical antifungal treatments versus device-based treatments.
Figure 2. Summary of device mechanisms for the treatment of onychomycosis. Starting from left: Lasers) heat the fungal infection under the nail through transmission as well as generation of reactive oxygen species causing fungal cell damage; photodynamic therapy (PDT)) involves excitation of a photosensitizer by a light source leading to the generation of reactive oxygen species; microdrilling) small holes through the nail to aid the topical antifungal agent to reach the nail bed; microwaves) increase the temperature of the fungus, denaturing its proteins, they also cause DNA damage, and trigger an immune response; ultrasound) uses acoustic streaming to push the active drug through the layers of the nail; iontophoresis) also drives drugs in a topical antifungals through the nail by first applying a charge to the drugs and then introducing an electric field across the affected nail to pull them; non-thermal plasma) in contact with the air generates both reactive oxygen and reactive nitrogen species to damage the fungus.
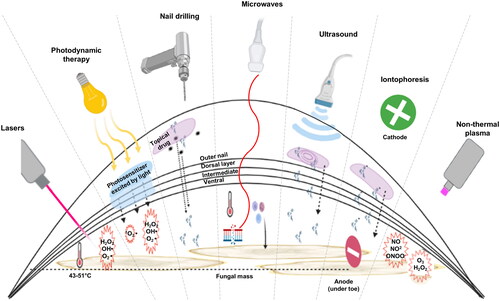
Figure 3. Mechanism of lasers and photodynamic therapy (PDT). (A) laser pulses have a photothermal effect on the fungal cells while sparing the surrounding dermis and tissue. (B) A topical photosensitizer is applied to a softened nail. A light source of specified wavelength excites the photosensitizer to a singlet state, to an excited singlet state, to an excited triplet state. In a type I photoreaction, the photosensitizer then interacts with biomolecules to produce unstable free radicals. Likewise, in a type II photoreaction the photosensitizer reacts with oxygen to produce singlet oxygen, which like free radicals, is cytotoxic to the fungus.
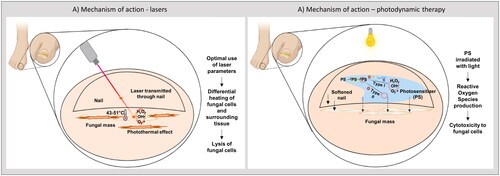
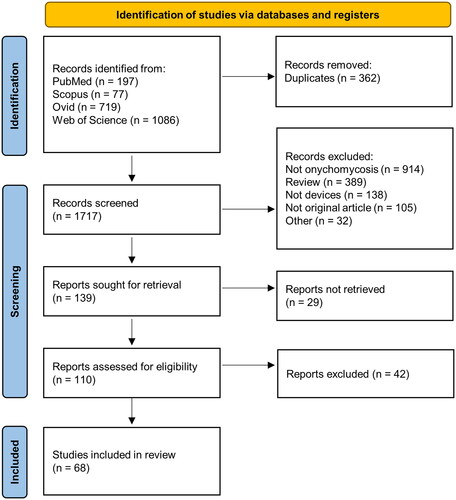
Figure 4. Summary of reports on clinical trials on devices from systematic search. From the 68 clinical studies obtained from the search, 53 reports on lasers, 9 reports on PDT, 2 reports on nail drilling, 2 reports on iontophoresis, and 2 reports on non-thermal plasma were identified. Quality of evidence in terms of studies reporting on the efficacy of monotherapy (lasers), RCTs, and complete mycological cure (negative culture and negative microscopy/histology) are depicted for (A) lasers and (B) other devices.
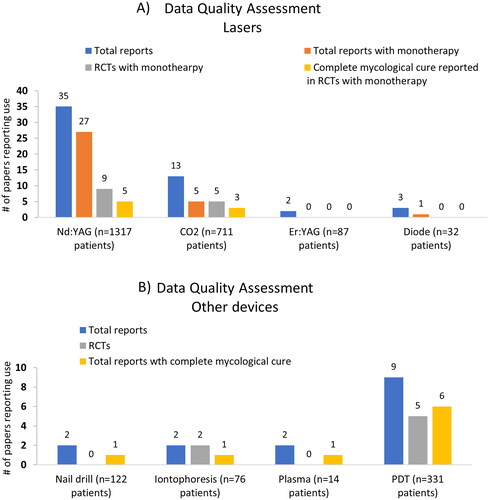
Table 2. Summary of randomized controlled trials (RCTs) on lasers for the treatment of toenail onychomycosis.
Table 3. Summary of randomized controlled trials (RCTs) on photodynamic therapy (PDT) for the treatment of toenail onychomycosis.
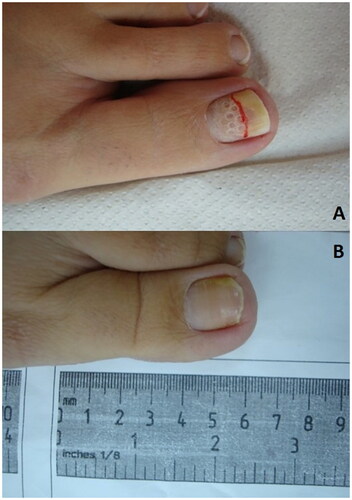
Figure 5. Photographs showing microwave treatment of toenail. Toenails of two patients treated with 4 and 5 sessions. (A) The toenail of a patient after the first microwave treatment, after 6 weeks, having received a total of 4 microwave treatments, and after 2 years follow-up. (B) The toenail of another patient after the first microwave treatment, after 1.5 years, having received 5 microwave treatments, and after 3 years at follow-up (Citation44).

Figure 6. Photographs showing nail drilling of a toenail. (A) the toenail Shortly after nail drilling and application of topical antifungal. (B) Healthy nail after 6 months, with clear nail observed.
Data availability statement
Data sharing not applicable – no new data generated.