Figures & data
Figure 1. Signaling cascade events during FcγRIIA-mediated platelet activation.
(1) Immunocomplexes of PF4, heparin and anti-PF4 antibodies bind to FcγRIIA activating Src family kinases. (2) This results in the phosphorylation of Syk and (3) activation of PLCγ and PI3 kinase. (4) PLCγ catalyzes the conversion of PIP2 to IP3 and DAG. IP3 induces calcium mobilization in the cells which ultimately phosphorylates light chain of non-muscle myosin IIA through calmodulin-dependent mechanism. Simultaneously, DAG activates PKC, which in turn directly catalyzes the phosphorylation events on light chain of non-muscle myosin IIA. (5) These events prompt cytoskeletal reorganization and (6) shape changes in the cell, inducing conformational changes in integrin, resulting in the association with fibrinogen. (7) Concomitantly, activated PI3K converts PIP2 to PIP3 enabling the recruitment of (8) BTK which might induce granule secretion. (9) The exocytosis of granules, harboring PF4, calcium, and other procoagulatory agents is accomplished by the concerted efforts of calcium-dependent SNARE proteins in the plasma membrane. (10) On the activated cell membrane prothrombinase complex forms along with factor Xa and factor Va, which directly participates in the coagulation pathway generating thrombin. Fibrin is formed from fibrinogen upon the action of thrombin, eventually leading thrombus formation. (11) Furthermore, anti-PF4 antibodies are able to bind to the newly released PF4 forming immune complexes that are able to activate FcγRIIA, starting the signaling cascade following FcγRIIA again.
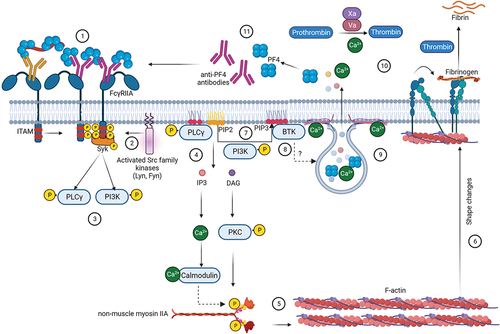
Figure 2. Different therapeutic interventions in HIT.
(a) Anticoagulants: either directly inhibit factor Xa or thrombin or indirectly by activating antithrombin. (b) (1) In addition to its anticoagulatory effect, danaparoid exerts a stoichiometric effect by direct interaction with PF4, thus limiting the binding of pathogenic anti-PF4/heparin antibodies to PF4. (2) Partially cleaved anti-PF4 monoclonal antibodies (e.g. deglycosylated monoclonal antibodies KKO or 5B9) directly interact with PF4, constraining the binding of pathogenic anti-PF4 antibodies to PF4. FcγRIIA-mediated activation of platelets is absent as these therapeutic antibodies do not have a functional Fc-part. (c) Therapeutic plasma exchange removes pathogenic anti-PF4/heparin antibodies from patient plasma. (d) (1) IVIG and also monoclonal antibodies directly bind to FcRn, inhibiting downstream signaling which accelerates degradation of pathogenic antibodies. However, the main effect of IVIG and DARPins is mediated by competitively inhibiting binding of the Fc-part of pathogenic immune-complexes to FcγRIIA. (2) BTKs, which are part of the FcγRIIA downstream signaling cascade can also be inhibited by pharmaceutical agents (BTK-inhibitors, e.g. ibrutinib), which in turn inhibits platelet activation.
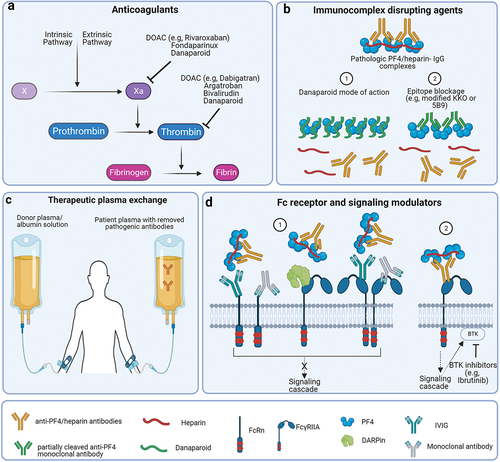
Table 1. Treatment options for anticoagulation in HIT and VITT.
Supplemental material
