Figures & data
Figure 1. GOS. Perpendicular scanning shows that the pleural line is thickened and blurred, the echogenicity in the near-field is enhanced, and the echogenicity in the far-field is significantly weakened, looking like groundglass opacity (A). Parallel scanning shows that the ground glass-like performance is more obvious in the near field (B). GOS is a characteristic ultrasound finding of grade I RDS.
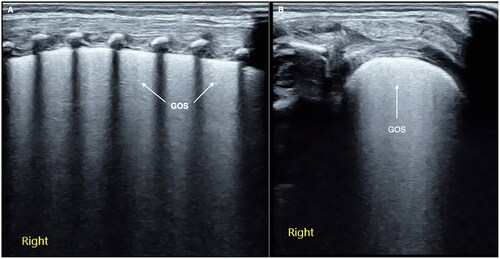
Figure 2. SFS. On the B-mode ultrasound, we can see a kind of specific lung consolidation, which is characterized by an obvious spot and patchy or thin line air-bronchograms in the lesion area, forming a snowflake-like manifestation, known as SFS. SFS is a characteristic ultrasound finding of grade II and above RDS.
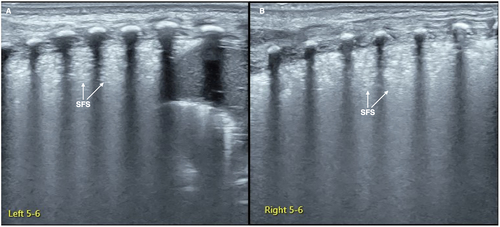
Figure 3. Normal lung LUS performance. On B-mode imaging, both the pleural line and A-line present as smooth, regular and hyperechoic lines, arranged in parallel and equidistant from each other, that is, a bamboo sign. On M-mode ultrasound, the presents as a sand beach sign.
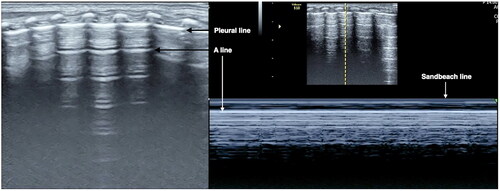
Figure 4. Grade I RDS. Grade I RDS patient. LUS showed GOS-like lung consolidation in the last two intercostal spaces of the left lung and DLP between its upper and lower lung fields (A). GOS was more typical when the probe was scanned along the intercostal space in parallel (B).
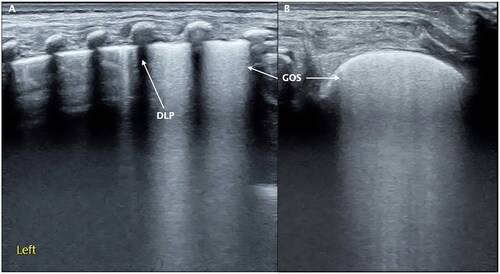
Figure 5. Grade II RDS. RDS patients. LUS showed the SFS-like lung consolidation only involved partial intercostal space (the right 6th region of this patient) of the right lung (A: perpendicular scanning; B: parallel scanning).
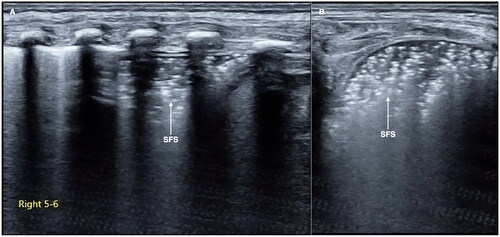
Figure 6. Grade III RDS-SFS-like consolidation invoked all of the lung fields. An infant with a gestational age of 29 weeks and birth weight of 1210 g experienced serious respiratory distress shortly after birth. LUS showed that the SFS-like lung consolidation involved all of the lung fields of the bilateral lungs, caused by grade III (i.e. severe) RDS.
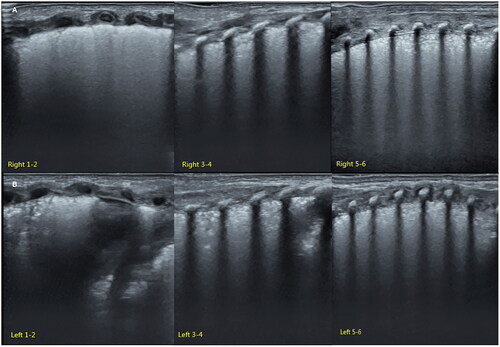
Figure 7. Grade III RDS: RDS result in pneumothorax. An infant with a gestational age of 28 weeks and birth weight of 1020 g experienced serious respiratory distress shortly after birth. LUS showed an SFS-like lung consolidation in his left lung (A). Bamboo signs on B-mode ultrasound (B) and stratosphere signs on M-mode ultrasound (C) in his right lung. Lung sliding disappeared in real-time ultrasound.
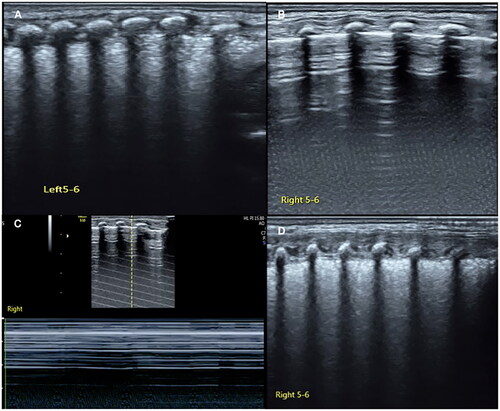
Figure 8. RDS complicated with pulmonary hemorrhage. A term RDS patient, bloody fluid emerging from the endotracheal tube during ventilator treatment. LUS examination revealed SFS-like lung consolidation with significant pleural effusion. The bloody fluid was withdrawn by thoracentesis. It was confirmed pulmonary hemorrhage due to RDS.
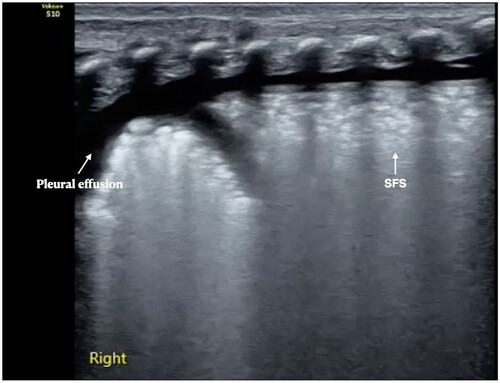
Figure 9. The identification of GOS and B-lines. It can be seen that the echogenicity of B-line (A) and confluent B-line (B) in far-field of the lung did not decrease significantly, while the echogenicity of GOS (C) significantly fading in the in far-field.
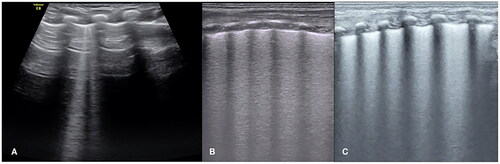
Figure 10. LUS manifestations in pneumonia. Patient with pneumonia. LUS showed large area lung consolidation with air – air-bronchograms, as well as irregular and serrated boundaries. We can see the consolidation is much different from that in RDS patients. The ultrasound findings of MAS were similar to those of pneumonia. Their identification needs to be combined with medical history, such as the time of onset, the presence of meconium contamination of amniotic fluid, etc.
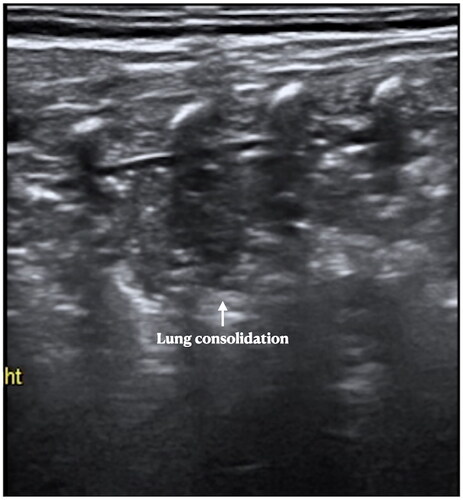
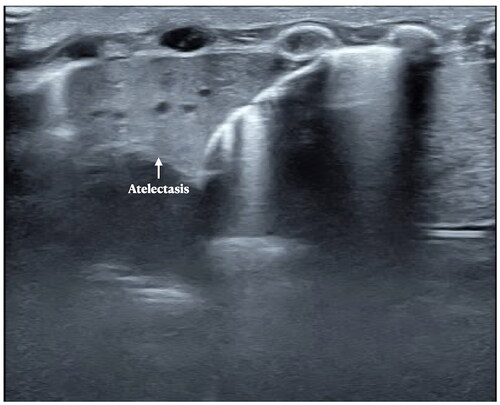
Figure 11. LUS manifestations in pneumonia. Patient with atelectasis. LUS showed significant lung consolidation with regular boundaries. We can see also the consolidation is much different from that in RDS patients and pneumonia. Atelectasis is not an independent disease, but a complication of other lung diseases such as pneumonia, MAS, RDS, etc.
Data availability statement
The data set used and analyzed are available from the corresponding author upon reasonable request.
