Figures & data
Figure 1. Increase in rate of maternal depression, prenatal antidepressant prescription, and prenatal SSRI prescription from 2013 to 2022. (A) Maternal depression rate from 2013 to 2022. Green line indicates prevalence rate of women who had depression diagnosis before the start of the pregnancy. Orange line indicates prevalence rate of prenatal depression. Blue line indicates prevalence of postpartum depression. As the definition of postpartum depression indicates depression up to one-year postpartum period, we did not evaluate the rate of postpartum depression of patients who delivered in 2022. (B) Comparison of prenatal depression rate in control period (6 March 2017 to 31 December 2019) and pandemic period (6 March 2020 to 31 December 2022). There was 50.3% increase in prenatal depression rate during pandemic period. (C) Prenatal antidepressant prescription rate from 2013 to 2022. Antidepressant with prescription rate below 0.01% is not displayed. (D) Comparison of prenatal antidepressant prescription rate in control period (6 March 2017 to 31 December 2019) and pandemic period (6 March 2020 to 31 December 2022). There was 36.0% increase in prenatal antidepressant prescription rate during pandemic period. (E) Prenatal SSRI prescription rate from 2013 to 2022. SSRI with prescription rate below 0.01% is not displayed. (F) Comparison of prenatal SSRI prescription rate in control period (6 March 2017 to 31 December 2019) and pandemic period (6 March 2020 to 31 December 2022). There was 36.0% increase in prenatal SSRI prescription rate during pandemic period. +p < .1; *p < .05; **p < .01; ***p < .001; ****p < .0001; *****p < .00001.
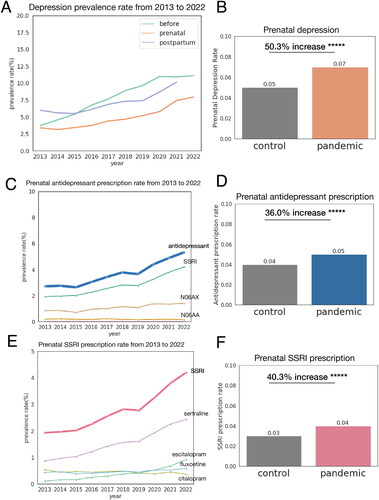
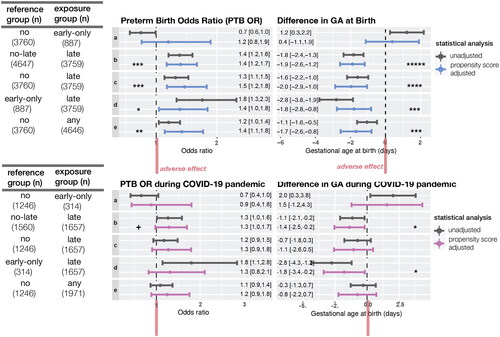
Figure 2. Increased risk of preterm birth and decreased gestational days at birth for women exposed to SSRI in second or third trimester. CI: confidence interval; GA: gestational age. The odds ratio of preterm birth and difference in the mean of GA at birth were calculated using log-binomial regression and linear regression adjusting for propensity score (top). Exposure groups were defined as follows. No: women with no SSRI exposure during pregnancy. Early only: women with SSRI exposure only in the first trimester. Late: women with SSRI exposure in the second or third trimester. Any: women with any SSRI exposure during pregnancy (early only + late). No-late: women with no SSRI exposure in the 2nd nor 3rd trimester (no + early only). This increased risk of the late SSRI exposure group was similar among subsample of patients who delivered during COVID-19 pandemic period (bottom). Each comparison (a–e) is defined in the table on the left. +p < .1; *p < .05; **p < .01; ***p < .001; ****p < .0001; *****p < .00001.
Supplemental Material
Download MS Word (341.3 KB)Data availability statement
Results have been aggregated and reported within this paper to the extent possible while maintaining privacy from personal health information as required by law. Data are archived within Providence St. Joseph Health systems in a HIPAA-secure audited compute environment. All clinical logic for data extraction has been shared within the paper and supplemental materials. Code is publicly available at https://github.com/Hadlock-Lab/YH_SSRI_PTB.
