Figures & data
Table 1. Comorbidity rates in MF, PV and ET compared with matched controls in a retrospective observational analysis of patients with MPNs.
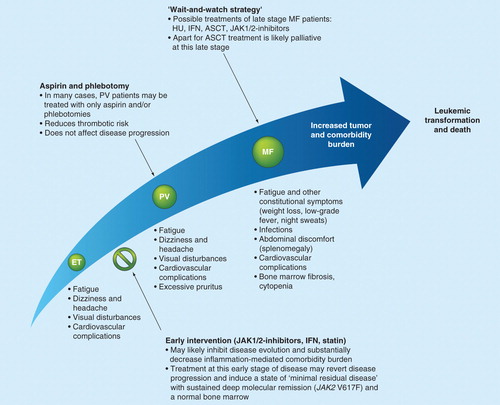
Figure 1. The assortment of comorbidities observed in patients with MPNs. Patients with MPNs display a variety of comorbidities that severely impact patient quality of life and survival. The increased morbidity and mortality in the MPNs are significantly affected by cardiovascular, pulmonary and abdominal complications as well as more global features including peripheral vascular insufficiency and an increased risk of developing fractures. A number of the listed comorbidities are related to the chronic inflammatory state that is associated with the MPNs and progression of disease.
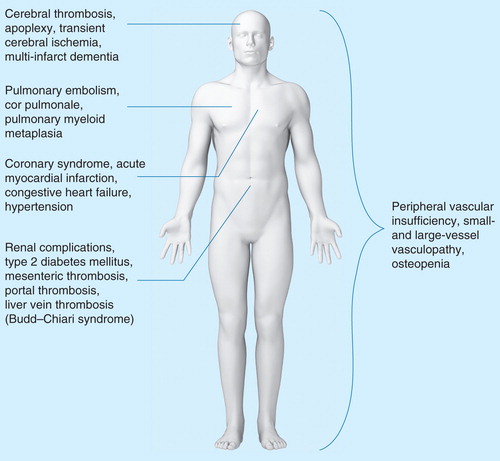
Figure 2. Tumor burden and comorbidity burden in patients with MPNs. Comorbidity burden increases from early disease stage (ET/PV) to the accelerated phase with myelofibrotic and leukemic transformation. In the JAK2 V617F-positive patient, the red area also depicts the steady accumulation of the JAK2 V617F mutation load, which promotes thrombosis and also induces increasing genomic instability, subclone formation and resistance to treatment. Long-term chronic inflammation induces increasing genomic instability and resistance to treatment and a heavy load of comorbidities, with ensuing impairment of quality of life. The ‘wait-and-watch strategy’ allows the cancer to progress and diminishes the possibility of a favorable outcome. The early intervention concept argues for treating the cancer at an earlier stage, preferably at the time of diagnosis, rather than at a later stage, when complications such as major thrombosis have occurred. The early-intervention concept implies early upfront combinatorial treatment with interferon-α2, a JAK inhibitor and statins.
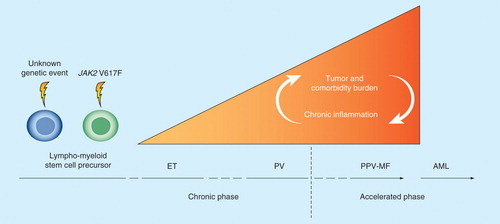
Figure 3. The MPN care pathway and the effect of early intervention. It is suggested that ET, PV and MF exist on a biological continuum and thus, early intervention with combination therapies including JAK1/2 inhibitors, IFN and/or statins is likely to result in the inhibition of disease evolution. It is important to note that in several centers, according to the EuLeuNet recommendations, younger ET patients without a history of thrombosis are not treated with cytoreductive agents unless the platelet count exceeds 1500 × 109/l or a thrombotic or hemorrhagic event has occurred. Similarly, PV patients may also be treated with aspirin and phlebotomies only rather than with cytoreductive agents.