Figures & data
Table 1 Baseline demographic and clinical characteristics from claims
Table 2 Baseline clinical characteristics from medical records
Figure 2 COPD exacerbations during the 12-month pre- and postindex periods.
Abbreviation: FEV1, forced expiratory volume in 1 second.
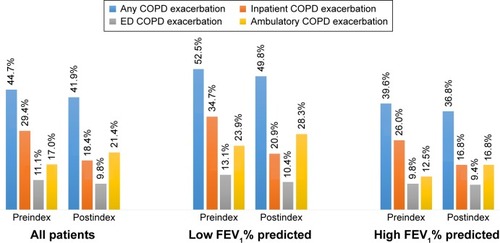
Table 3 Baseline all-cause and COPD-related health care resource utilization and costs
Table 4 12-month postindex all-cause and COPD-related health care resource utilization and costs
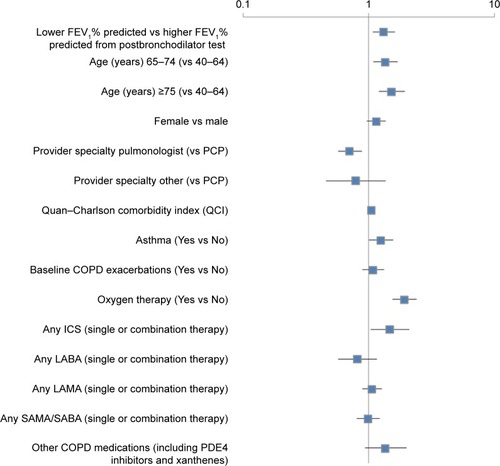
Figure 3 Factors associated with COPD exacerbations within the 12-month postindex period.
Abbreviations: FEV1, forced expiratory volume in 1 second; PCP, primary care physician; ICS, inhaled corticosteroids; LABA, long-acting β-agonist; LAMA, long-acting muscarinic agent; SAMA, short-acting muscarinic antagonist; SABA, short-acting (inhaled) β2-adrenergic agonist; PDE4 inhibitors, phosphodiesterase-4 inhibitors.
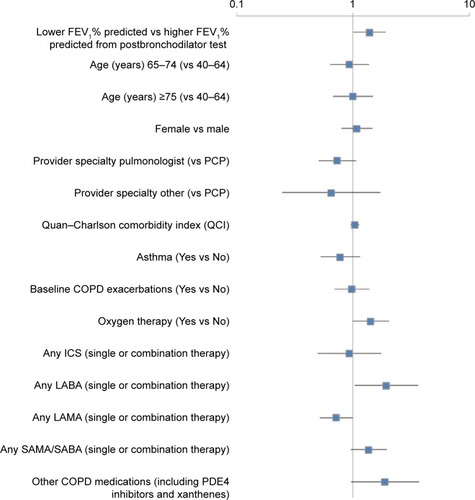
Figure 4 Factors associated with COPD-related health care costs within the 12-month postindex period.
Abbreviations: FEV1, forced expiratory volume in 1 second; PCP, primary care physician; ICS, inhaled corticosteroids; LABA, long-acting β-agonist; LAMA, long-acting muscarinic agent; SAMA, short-acting muscarinic antagonist; SABA, short-acting (inhaled) β2-adrenergic agonists; PDE4 inhibitors, phosphodiesterase-4 inhibitors.