Figures & data
Figure 1 Monocyte function in normal vs AATD lungs. (1) In response to infection/inflammation, circulating monocytes enter the lungs where they release AAT which acts to neutralise NE. (2) Monocytes also release cytokines including TNFα, CXCL-8, LTB4 and IL-6 to recruit immune cells including neutrophils and monocytes. (3) AAT blocks LPS induced pro-inflammatory cytokine release, thus limiting inflammation. (4) Monocytes differentiate into monocyte-derived macrophages, adding to the alveolar macrophage pool. (5) In AATD, AAT polymers form in monocytes, leading to elevated release of pro-inflammatory cytokines including IL-6 and CXCL-8 which increases neutrophil recruitment (6), thus increasing NE levels and activity in the lungs. (7) Levels of AAT below the putative protective threshold (<11μmol/L) causes LPS induced pro-inflammatory cytokine release to increase, driving inflammation.
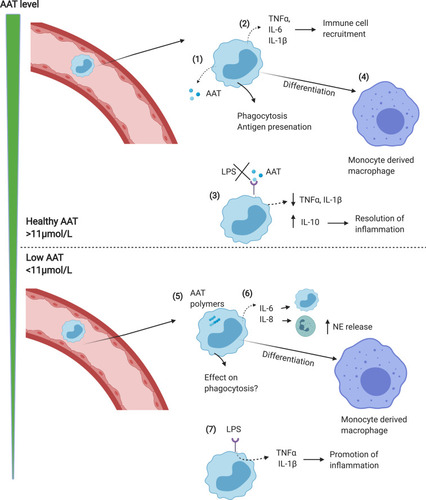
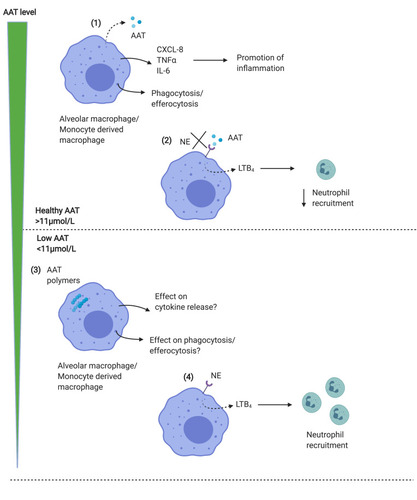
Figure 2 Macrophage function in normal vs AATD lungs. (1) Alveolar macrophages or MDM release AAT in response to inflammatory stimuli, together with proinflammatory cytokines including CXCL-8 and IL-6 which promote inflammation. Macrophages also phagocytose bacteria, and efferocytose apoptotic cells. (2) AAT acts to block the binding of neutrophil elastase to macrophage receptors, limiting the release of LTB4 resulting in reduced neutrophil recruitment to the airways, which limits inflammation. AAT is thus anti-inflammatory in the lungs. (3) In AATD, both MDM and alveolar macrophages contain AAT polymers, which may limit phagocytic function. (4) Levels of AAT below the putative protective threshold (<11μmol/L) results in the ability of NE to bind to receptors on macrophage surface, increasing LTB4 release and recruiting neutrophils, which further contribute to NE levels in the lungs, driving inflammation.