Figures & data
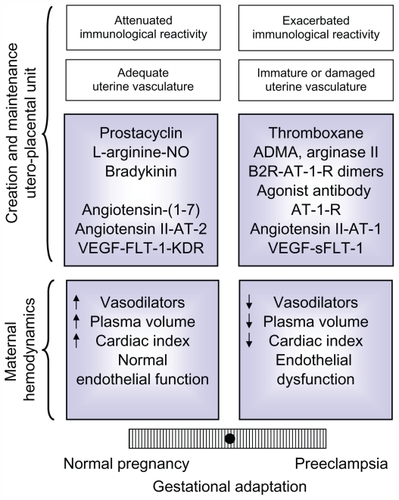
Figure 1 Interactions between the different vasodilator systems.
Abbreviations: ACE, angiotensin converting enzyme; AT-1-R, angiotensin II type 1 receptor; AT-2-R, angiotensin II type 2 receptor; B2R, bradykinin 2 receptor; eNOS, endothelial nitric oxide synthase; Flk, fetal liver kinase 1; Mas-R, Mas receptor; NO, nitric oxide; PGH2, prostaglandin H2; VEGF, vascular endothelial growth factor; VEGF-R2, VEGF receptor 2.
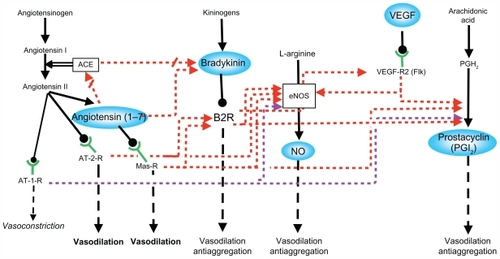
Figure 2 Diagram of the uteroplacental interface, showing its main cell types and the vasodilator repertoire of each type.Citation9 The discontinuous yellow line depicts the path of trophoblasts that detach from the anchoring column to migrate through the uterine stroma, destroy the vascular smooth muscle, and colonize the lumen of the spiral arteries.
Abbreviation: NK, natural killer.
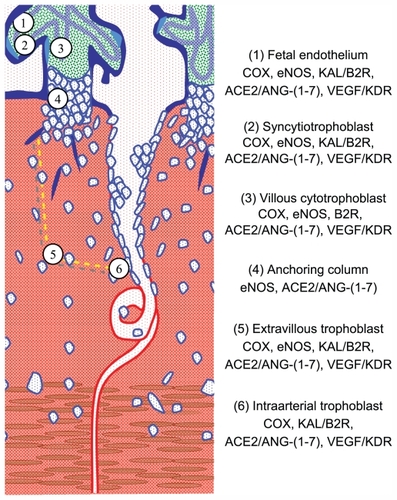
Figure 3 Diagram showing the relation between the placenta and the maternal endothelium, in ischemic conditions, increased placental mass, and underlying cardiovascular risks. The microphotographs of the placental villi show syncytial knots prior to being deported into the maternal circulation (orange circles). In addition, the placenta sheds factors to the maternal circulation (green stars: sFLT-1, agonist autoantibodies to the AT-1-R, ADMA, and reactive oxygen species). Both syncytiotrophoblast microparticles and the soluble factors provoke endothelial dysfunction in pregestational healthy (smooth borders) or dysfunctional endothelial cells (spiky borders). Pregestational endothelial dysfunction also hinders uterine artery transformation (red broken arrow).
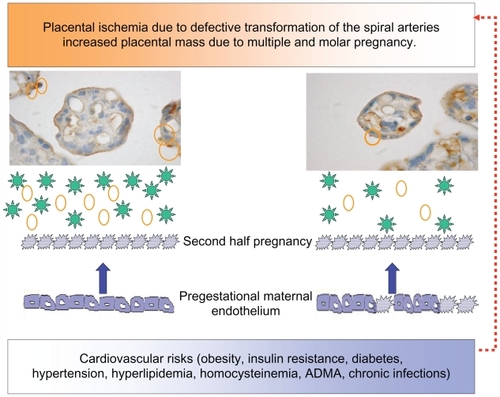
Figure 4 Balance of factors that determine an adequate or defective adaptation to pregnancy in the maternal hemodynamics and in the development and maintenance of the uteroplacental unit,Citation9 based on the equilibrium initially proposed for PGI2 and TXA.Citation45 The modulation of the maternal immune reaction and the state of the maternal vasculature have also been included, because though not analyzed in this review, they influence the adaptation to pregnancy.
Abbreviations: ADMA, asymmetric dimethylarginine; AT-1-R, angiotensin II type 1 receptor; AT-1, angiotensin II type 1; AT-2, angiotensin II type 2; B2R, bradykinin 2 receptor; KDR, kinase domain receptor; FLT-1, fms-like tyrosine kinase 1; NO, nitric oxide; sFLT-1, soluble fms-like tyrosine kinase 1; VEGF, vascular endothelial growth factor.