Figures & data
Figure 1 Wnt signaling pathways and the biology of sclerostin.
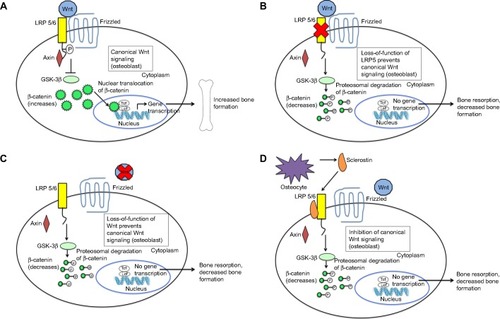
Figure 2 Clinical effects of sclerosteosis and van Buchem disease.
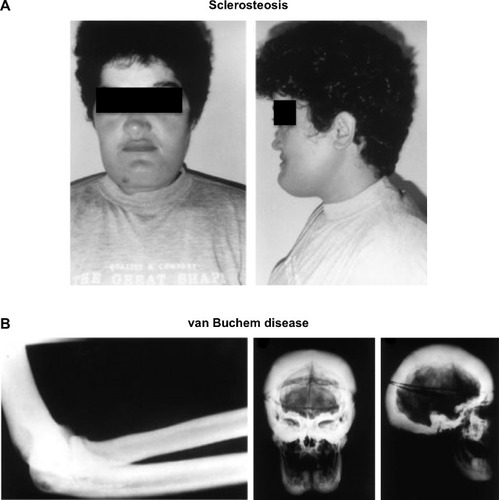
Figure 3 The effect of sclerostin inhibition on Wnt signaling.
Abbreviation: MAb, monoclonal antibody.
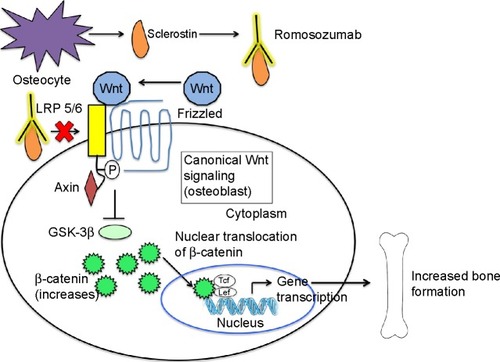
Table 1 Summary of Phase I and II studies of romosozumab
Table 2 Summary of Phase III studies of romosozumab in osteoporosisTable Footnote*
