Figures & data
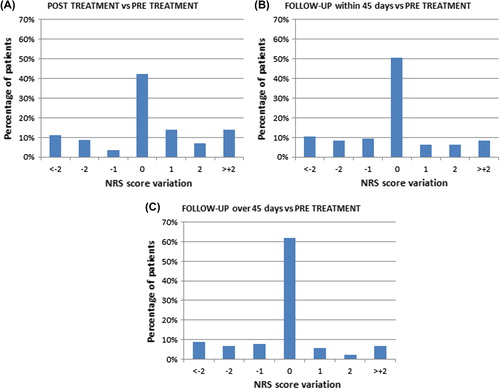
Figure 1. Clinical characteristics of patients. Patients referred for electrochemotherapy present with quite different clinical problems. Top panels: 93-year-old male patient with squamous cell carcinoma of the scalp before treatment (left) and after three treatments (right), treated at University of Rome. Middle panels: 88-year-old female patient with multiple metastases of malignant melanoma on left lower leg, recurrence after several other treatments including surgery and radiotherapy (left side). Four months after one session with electrochemotherapy (right side) all cutaneous and subcutaneous metastases regressed. Typical hyperpigmentation and fibrosis of the skin. Lower panels; 58-year-old female patient with extensive relapse and metastases of breast cancer of the chest wall, accompanied by extensive bleeding and malodour (left side). Eight weeks after first electrochemotherapy session, regression of exophytic tumors, cessation of bleeding and malodur. Development of new metastases at the border of the treated area. Latter two cases treated in Ludwig-Maximilian Institute, Munich.
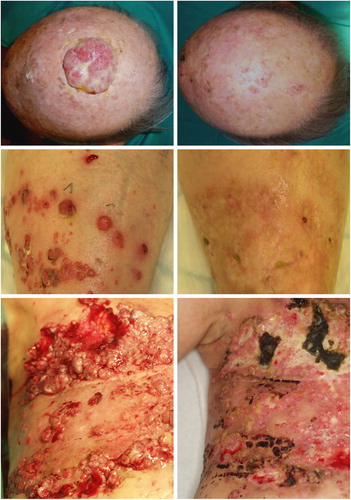
Figure 2. Percentage distribution of patients in relation to their pain score. The reported pain relating to treated cutaneous metastases using numeric rating scale (NRS) is illustrated in (A) before treatment, (B) within 24 hours from treatment – either after completion of treatment in local anaesthesia or before discharge from hospital in the case of general anaesthesia, (C) within 45 days from treatment, (D) after more than 45 days from treatment.
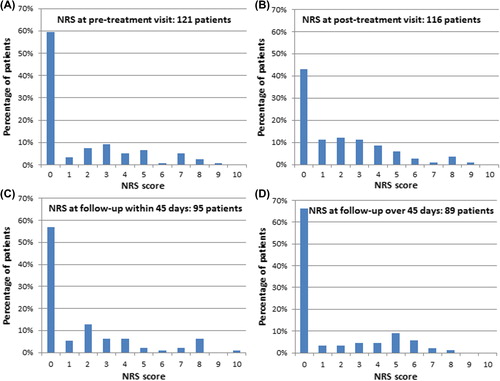
Table I. Patient demography and treatment choices.
Table II. Distribution of patients with regards to pain medication before electrochemotherapy, at follow-up within 45 days after treatment, and at follow-up after more than 45 days from treatment.
Table III. Pain intensity at follow-up within 45 days: association with parameters recorded at pre-treatment visit, and treatment data.
Table IV. Pain intensity at follow-up: relationship with the response per patient on the largest nodule.
Figure 3. Change in numeric rating scale score for pain before and after treatment. The change in numeric rating scale (NRS) score for pain with respect to NRS score before treatment is illustrated for (A) within 24 hours from treatment – either after completion of treatment in local anaesthesia or before discharge from hospital in the case of general anaesthesia, (B) within 45 days from treatment, (C) after more than 45 days from treatment. 0 = no change, + 1 = one score up from baseline value (e.g. from NRS = 3 to NRS = 4), and likewise -1 = one score down.