Figures & data
Table 1 Immune-Related Response Criteria in Relation to Conventional Criteria
Figure 1 Coronal maximal-intensity-projection PET whole body scans obtained at baseline and Weeks 12, 24, 38, and 50 during therapy with ipilimumab 3 mg/kg in Patient A. Melanoma metastases are indicated by red arrows. At baseline, scans showed metastatic muscular, lymph node, lung, intestinal, and bone lesions. A Week 12 assessment showed a rapid response with regression of most of the metastatic sites. Only a muscular metastasis in the upper left leg and the bone metastases in the right knee and tibia remained 18FDG-avid. At Week 24, there was a disappearance of the muscular upper left leg metastasis and the skeletal knee metastasis became 18FDG-negative. At Week 38, there was a reappearance of metastatic mediastinal lymph nodes (blue arrow) and the patient was given retreatment therapy with ipilimumab. Repeat scans after retreatment showed a stabilisation of the mediastinal lymph node and bone (right tibia) metastases.
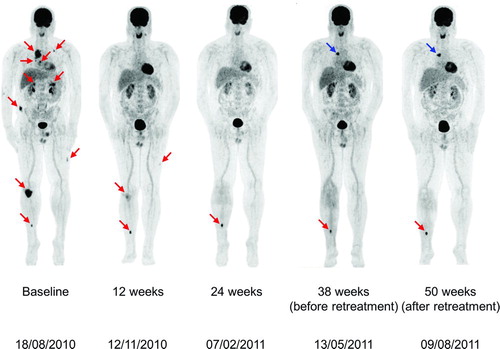
Figure 2 (Top) Axial sections of total body 18FDG-PET/CT scans in Patient B at baseline and evaluation in Weeks 12, 24, and 33 following initiation of ipilimumab 3 mg/kg. (A) Baseline: presence of metastases in the quadriceps and hamstring muscles, mesenteric, duodenal, lung, and several mediastinal locations. Melanoma metastases are indicated by red circles. (B) Images at 12 weeks showing disappearance of metastases in the quadriceps and hamstring muscles, metabolic normalization of mesenteric metastases and disappearance of lung metastases; metabolic activity persisted in the duodenal lesion and two new mediastinal lymph node metastases and a new peri-hepatic lymph node metastasis appeared (blue circles). (C) Images at 24 weeks after initiation of ipilimumab showing disappearance of mediastinal and peri-hepatic lymph node metastases and persistent activity of the duodenal lesion. (D) At 33 weeks after initiation of ipilimumab, there was a continuing response of all previously active lesions with the exception of persistence of 18FDG-uptake in the duodenal lesion. (Bottom) Corresponding coronal maximal-intensity-projection PET whole body scans of Patient B at baseline and subsequent assessments.
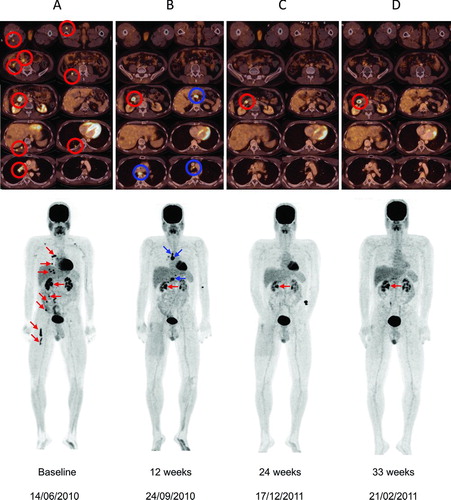
Figure 3 (Top) Axial sections of total body 18FDG-PET/CT scans in Patient C. Views A1 and B1 show 18FDG-avid right retroclavicular and retroperitoneal lymph node metastases. (Bottom) Corresponding coronal maximal-intensity-projection PET images at baseline and subsequent assessments. Baseline scan shows 18FDG-avid right retroclavicular and retroperitoneal lymph node metastases. At 12 weeks after starting treatment with ipilimumab 3 mg/kg, scan showed normalization of both the retroclavicular lesion and two out of four retroperitoneal lymph node metastases (red arrows) with simultaneous growth of the other two retroperitoneal lymph node metastases (blue arrows). At Week 24, there was a regression of all lymph node metastases, resulting in a CR at Week 36.
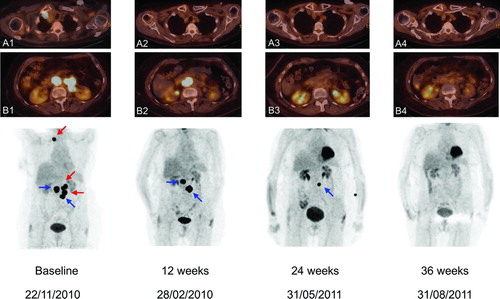
Figure 4 Coronal maximal-intensity-projection PET whole body scans obtained at baseline and Weeks 12, 24, 43, and 56 during therapy with ipilimumab 3 mg/kg in patient D. At baseline, before he started ipilimumab 3 mg/kg, there were 18FDG-avid metastases in the liver, para-iliac lymph node and distally in the inner left upper leg (red arrows). At the first evaluation in Week 12, there was regression of the liver metastasis but increases in the dimensions of (and 18FDG uptake in) the para-iliac lymph node and distal upper leg metastases and the appearance of a new iliaco-femoral lymph node metastatic lesion (blue arrows). Evaluation in Week 24 showed further regression of the liver metastasis and regression of the para-iliac metastasis and the distal metastasis in the left leg with complete loss of 18FDG uptake in these two lesions; there was an increase in size and 18FDG uptake in the iliaco-femoral metastasis and appearance of a new proximal lesion in the left leg. Immediately before retreatment, there was near-complete regression of the liver and para-iliac metastases but further progression of the other three lesions. After retreatment, all lesions further regressed in size with complete loss of 18FDG uptake.
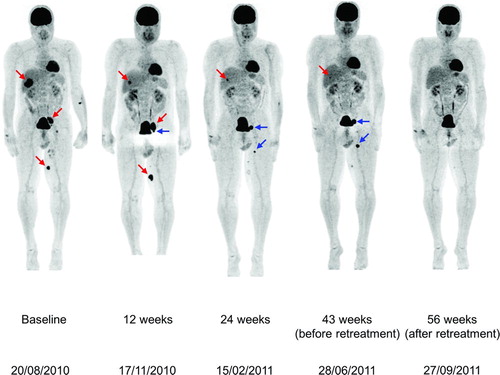
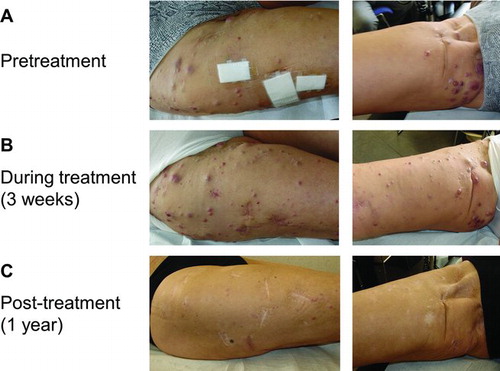
Figure 5 (A) In-transit melanoma metastases on the right leg prior to therapy with ipilimumab 3 mg/kg. (B) During the first weeks of treatment, there was an increase in size and number of the right leg in-transit lesions. C. Two months after starting ipilimumab therapy, the in-transit metastases slowly regressed and all disappeared (as illustrated 1 year after ipilimumab treatment).