Figures & data
Figure 1. Seven days after tumor implantation, convection-enhanced delivery of PEGylated liposomal doxorubicin was performed into tumor of 9L isografted intracranial tumor model. Hematoxylin and Eosin (H&E) staining of representative two rat brain sections show the tumor formation (A, C). Fluorescent detection of the doxorubicin in same sections revealed robust distribution of PLD in the tumor mass and surrounding tumor margin (B, D). Note the intra-tumoral distribution (arrow) and extra-tumoral distribution (arrowhead).
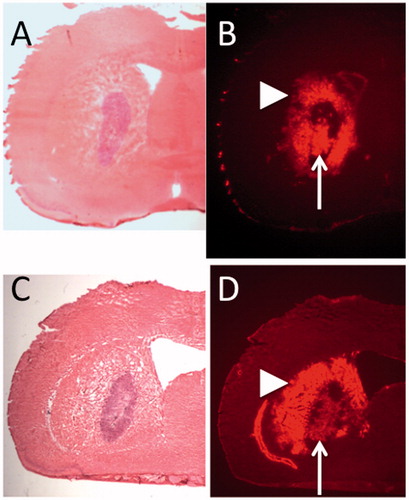
Figure 2. In the F98 glioma intracranial isografted model, trypan blue dye was infused peri-tumorally by CED. Results from 2 representative rats are shown (upper and lower). Distribution of Trypan-blue dye (left) and H&E staining of the same section (right). The dye effectively distributed into the tumor surrounding brain at the tumor-brain interface.
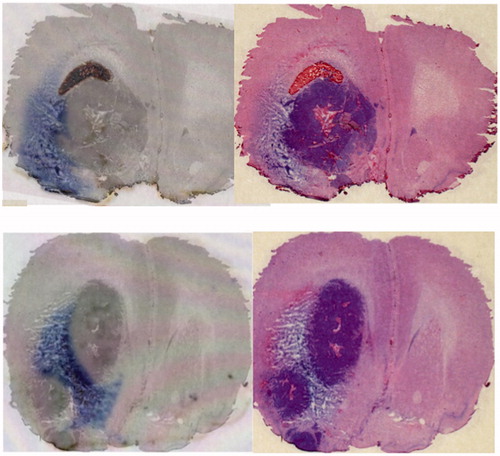
Figure 3. Volume of distribution (Vd) observed in rats that received Evans blue infusions with different mode of infusions were compared. Vd after intra-tumoral infusion, peri-tumoral infusion after tumor removal, peri-tumoral infusion without tumor removal, and peri-tumoral infusion without tumor removal with prior use of dexamethasone, were 97.6 ± 3.9 mm3 (mean ± standard deviation), 74.5 ± 14.4 mm3, 112.7 ± 4.7 mm3, and 130 ± 6.6 mm3, respectively. Representative bright-field images for each group are shown at the bottom. *1; p = 0.0008, *2; p < 0.0001, *3; p < 0.0001.
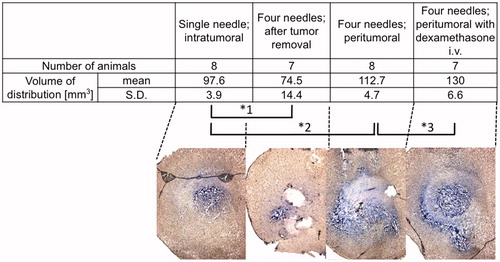
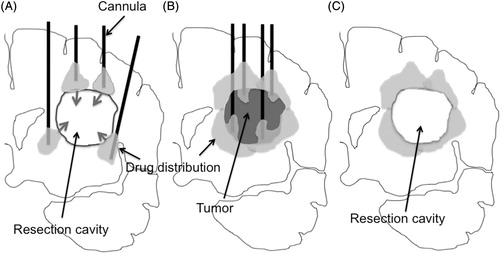
Figure 4. Schema of the current problem for post surgical peri-tumoral CED (A). After tumor resection, the brain surrounding the tumor is adjacent to a lower pressure space, i.e. resection cavity. Once the infusate leaks into the resection cavity during CED, the distribution into surrounding brain ceases. Schema of proposed pre-surgical CED (B). As demonstrated in , peri-tumoral CED prior to tumor removal can distribute infusate robustly into brain surrounding the tumor at the tumor-brain interface. Infusion from multiple cannulae inserted into the peri-tumoral area enables robust drug distribution at the tumor-brain interface. Removal of the tumor afterward may be ideal (C). Brain tissue surrounding resection cavity contains distributed drug after surgical resection.