Figures & data
Figure 1. Distribution of fractures by age and sex (from Paper 4). Copyright Journal of Bone and Joint Surgery [Am], reprinted with permission.
![Figure 1. Distribution of fractures by age and sex (from Paper 4). Copyright Journal of Bone and Joint Surgery [Am], reprinted with permission.](/cms/asset/77fa4aae-9f6d-4749-bb85-4eea8bae0744/iort_a_789731_f0001_b.jpg)
Figure 2. Measuring the sagittal displacement of distal radial fractures in children. α represents the angular displacement caused by the fracture.
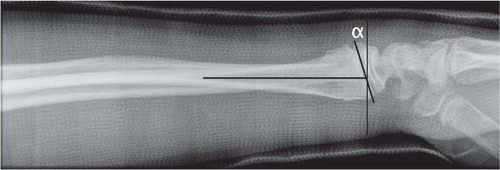
Figure 3. Examples of fractures from each category. A: Buckle fracture B: Greenstick fracture C: Complete fracture D: Physeal fracture (From Paper 3). Published by BioMedCentral Musculoskeletal Disorders.
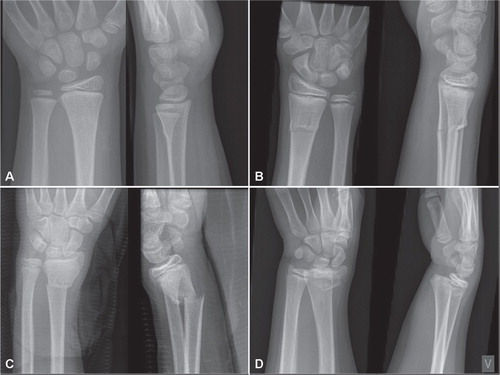
Figure 4. The Salter-Harris classification of growth plate injuries. Type I is a plain fracture through the physis. Type II includes a metaphyseal fragment. Type III is an intraarticular physeal fracture without affection of the metaphysis. Type IV has both intraarticular affection and a metaphyseal component. Type V is a compression injury of the physis. There is some controversy regarding the existence of type V.

Figure 5. Lateral angulation during the immobilization period in plaster of unreduced greenstick fractures. Note the tendency of the lateral angulation to increase throughout the period. (Data from Paper I).
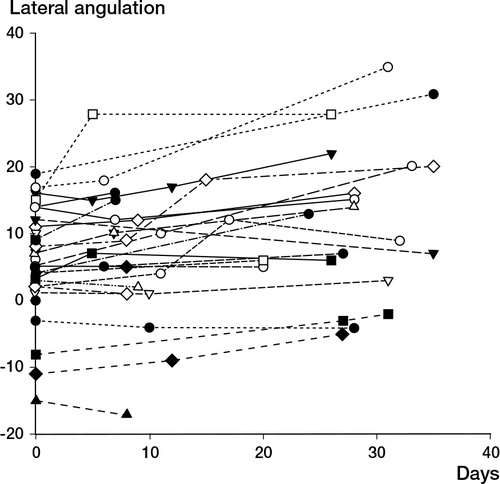
Table 1. Limits of angulation of distal radial metaphyseal fractures that will remodel anatomically. Based on references Citation(3;25;37;39;58;61;152)
Figure 7. Growth arrest of the distal radial physis following a SH Type 2 fracture in a 12 year-old girl that was initially reduced on the day of injury, and re-manipulated 3 days later due to loss of reduction.
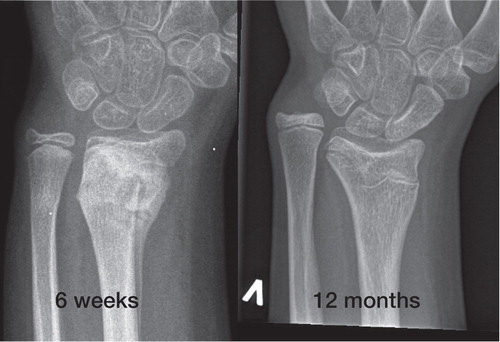
Table 2. Mechanism of injury for 114 Gartland 2 and 3 supracondylar humerus fractures treated with closed reduction and percutaneous pining at Akershus University Hospital between 1999 and 2005
Figure 8. The Gartland classification for supracondylar humerus fractures in children. Type 1: Undisplaced. Type 2: Displaced, with intact posterior cortex. Type 3: Displaced with no bony contact between fragments.
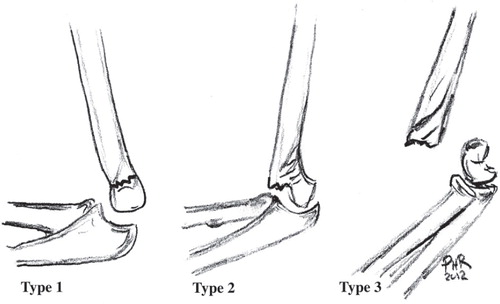
Figure 9. Gartland 3 supracondylar humerus fracture in a 3 year old girl, managed by closed reduction and percutaneous pinning.
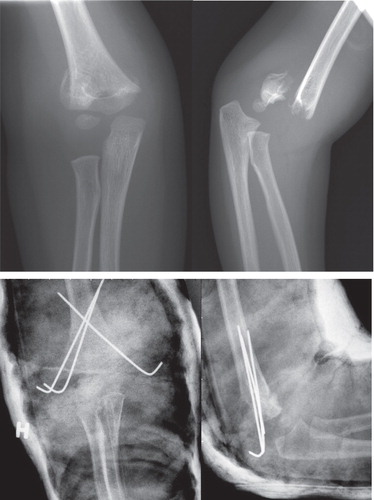
Figure 10. Cubitus varus after a supracondylar humerus fracture of the right elbow. The patient had no functional complaints, normal neurovascular status and had a Quick-DASH score of 0 four years after injury.
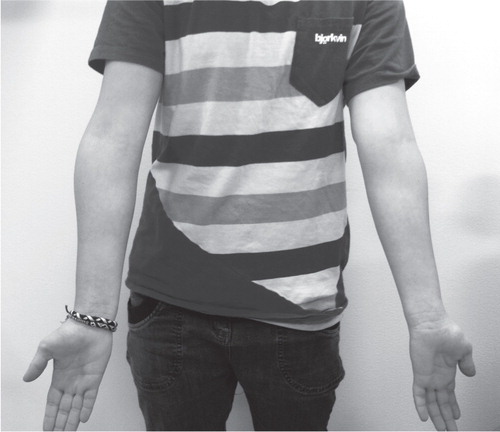
Table 3. Flynn’s criteria for grading functional and cosmetic outcome of supracondylar humerus fractures in children Citation(34). Values are degrees
Table 4. Most common fractures by most common sport activity. Values are number (%). (From Paper 4) Copyright The Journal of Bone and Joint Surgery [Am]. Reprinted with permission
Table 5. Fracture rate estimates for common children activities. Estimates number of fractures per 104 hours of activity. Confidence interval assuming Poisson distribution of fractures (From Paper 4) Copyright The Journal of Bone and Joint Surgery [Am], reprinted with permission
