Figures & data
Figure 1. An Essex-Lopresti lesion: comminuted fracture of the radial head, resulting in proximalization of the radius and dislocation of the unstable distal radio-ulnar joint.

Figure 3. Part 1 of the sequence of development of an Essex-Lopresti lesion. A. Unloaded specimen. B. Loading leads to slight impaction and bending of radius and ulna, and thereby to a transverse movement of the radial and ulnar shaft away from each other (see increasing distance between radial and ulnar shaft), leading to tension of the interosseous membrane (IOM). C. Due to the rising tension in the IOM, the IOM ruptures and ulna and radius separate further. D. A slight proximalization of the radius—and thereby of the radial head—is detectable (see movement of radial head in relation to the black line).
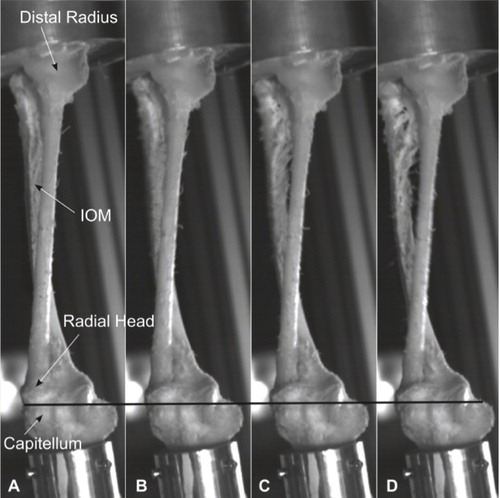
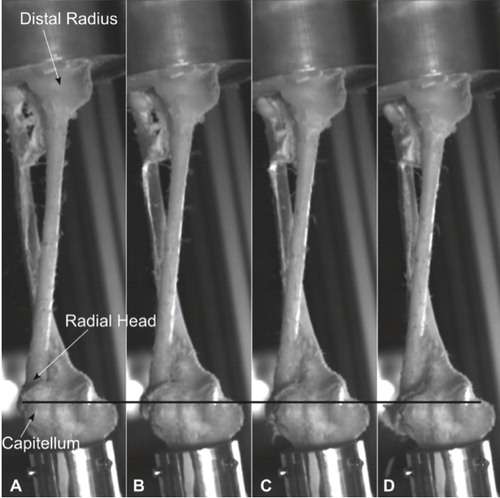
Figure 4. Part 2 of the sequence of development of an Essex-Lopresti lesion. A. The intraosseous membrane is completely ruptured. Radius moves downwards (proximal direction), leading to fracture of the radial head and increasing displacement (again in relation to the black line). B–D. The lesion progresses to a dislocation of the distal radio-ulnar joint, then to a full Essex-Lopresti lesion.
Initiated and diverted impulses, calculated with the measured forces (Ns) of the superior and inferior sensor
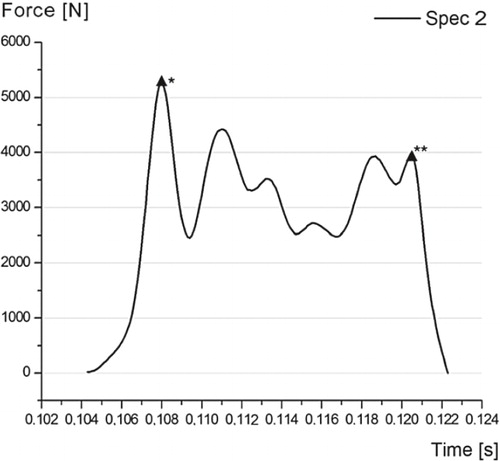
Figure 5. Curve representing force over time in specimen 2. * marks the moment of failure of the interosseous membrane, as in Figure 3C. ** marks the moment of fracture and proximalization of the radius, as in Figure 4B. The irregular lines in-between can be explained by dislocation movements of the radial head before the fracture, resulting in complete longitudinal instability.