Figures & data
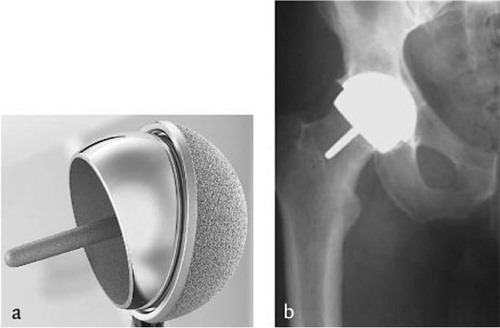
Figure 1a. Example of a cemented total hip arthroplasty with polyethylene cup and polished stem. 1b. Radiographic appearance.
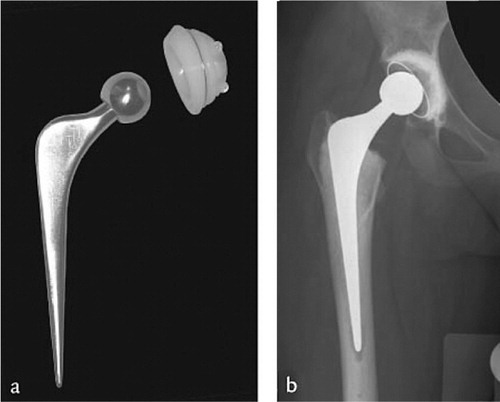
Figure 2a. Cementless total hip arthroplasty with screw cup and titanium stem. 2b. Radiographic appearance.

Table 1. Classification of acetabular deficiencies (AAOS)
Figure 4. Technique of acetabular solid grafting: (A) Graft is fixated with two cancellous lag screws with its sclerotic convex side toward the defect as an inlay graft. (B) Reaming of the graft to prepare for a cemented socket. (C) Final situation before cementation and insertion of the acetabular component.
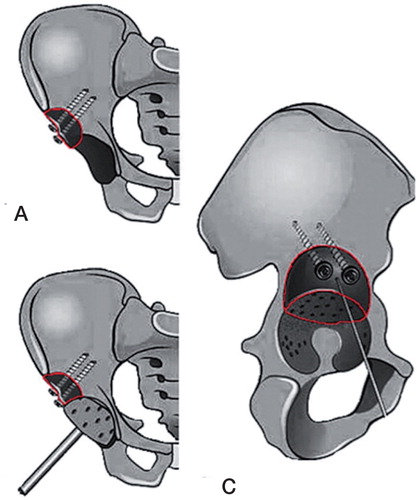
Figure 5. Technique of acetabular impaction bone grafting: (a) after localisation of the defect a mesh is situated and fixated using screws; (b) the contained defect is now filled with bone graft; (c) the grafts are impacted with a hammer and (d) a cemented cup is inserted.
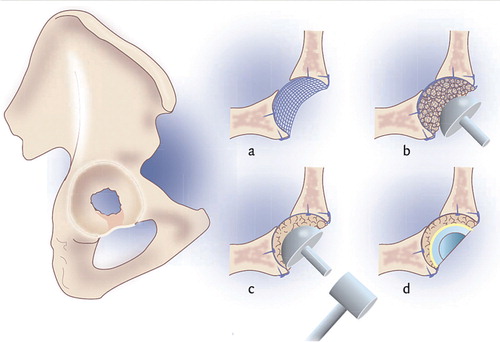
Figure 6. Fixation method of total registered number of 24,595 primary THAs in patients of all ages in the Netherlands in 2012.
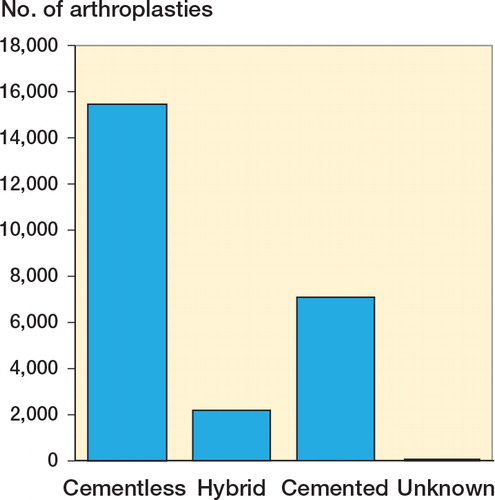
Figure 7. Method of fixation per age group in the Netherlands in 2012. Redrawn from source data LROI - graphics LROI-Dashboard in ProMISe accessed December 2013.
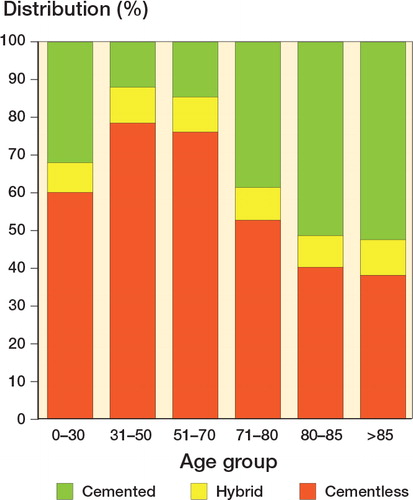
Table 2. Primary diagnosis of patients receiving a THA in 2012. Source data LROI accessed December 2013. Values are percentages
Figure 8. A. A preoperative radiograph of a 29-year-old woman with bilateral secondary osteoarthritis due to Bechterew’s disease. B. The hips after bilateral cemented THA with acetabular impaction bone grafting of a cavitary defect. C. At 17 and 18 years after the reconstruction there was incorporation of the bone graft and no signs of loosening except for an acetabular radiolucent line at the right hip in zone III.
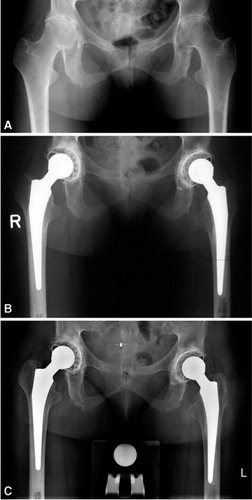
Figure 9. Radiographs of acetabular reconstruction using impaction bone grafting with a mesh covering the graft; at the right the incorporation of the graft can be seen at 16 years of follow-up
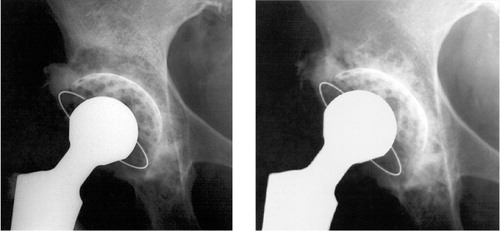
Figure 10. (A) Preoperative radiograph of a 55-year-old woman with bilateral DDH, classified as a Crowe III, Hartofilakidis C, and Edinburgh system A2 F3. (B) Postoperative radiograph showing bilateral reconstruction using roof grafts and a cemented Exeter THA after femoral shortening osteotomy. (C) Radiograph 15 years after the reconstruction showing incorporation of the roof grafts without evidence of loosening or resorption of the graft but signs of wear.
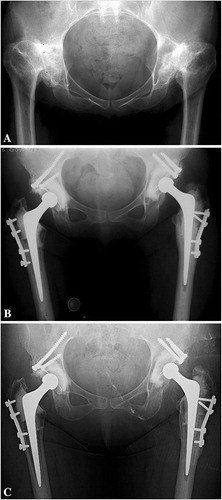
Figure 11. Radiograph of a Zweymüller stem (type Hochgezogen) with the CSF cup in a 69-year old man more than 21 years after the index operation with no evidence of loosening but showing polyethylene wear.

Figure 13. Markov model with cycles of 1 year to estimate QALYs and costs accumulating over a time period of 15 years.
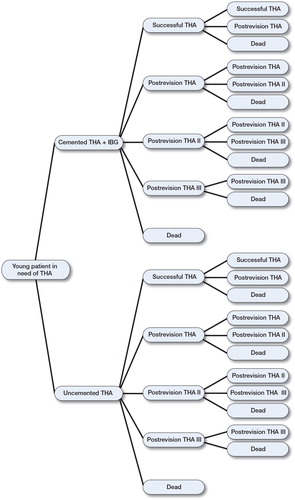
Figure 14. Incremental cost-effectiveness plane showing 2 scenario’s. In the baseline scenario (black dots), almost 90% of the simulated ICERs lay in the southeast quadrant meaning that cemented with grafting is more cost-effective than the uncemented option. The second scenario with equal survival rates for both options (red dots) still shows an effect gain (higher QALY) for cemented with grafting but at higher costs.
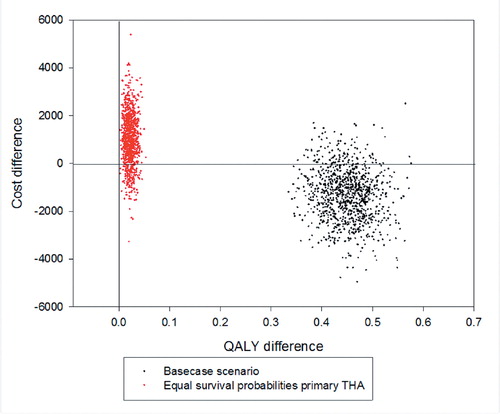
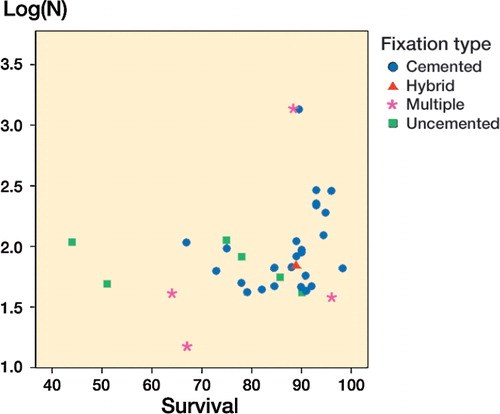
Table 3. Overview of literature a of acetabular bulk grafts in patients with DDH with a mean follow-up of 10 years or longer