Abstract
Background
Human immune-deficiency virus/acquired immune-deficiency syndrome predisposes to opportunistic parasitic infestations of the gastrointestinal tract. This study aimed to determine the prevalence of intestinal parasites in newly diagnosed treatment naïve HIV/AIDS patients.
Methods
This hospital-based cross-sectional study was carried out from December 2010 to June 2011. Questionnaires were administered to 238 HIV/AIDS subjects, and 238 age and sex-matched controls. CD4+ T cell count was carried out on HIV-positive subjects. Stool samples were examined using direct microscopic and modified Ziehl-Neelsen methods. Positivity of intestinal parasites was taken as the presence of worms, oocyst, cyst, ova or larvae in the stool samples.
Results
Ninety males and 148 females were studied for the HIV-positive and HIV-negative controls respectively. Intestinal parasitic infestation in HIV-positive subjects was 68.5%, and was significantly higher than in the HIV-negative controls 49.2% (P < 0.05). In HIV-positive subjects, Cryptosporidium spp. was the commonest (55.0%) parasite isolated. Others were Cyclospora cayetanensis (41.2%), Isospora belli (3.0%), Entamoeba histolytica (8.4%), Giardia lamblia (3.7%), Ascaris lumbricoides (2.5%), Strongyloides stercoralis (1.7%), Trichuris trichiura (0.8%) and Schistosoma mansoni (0.4%). HIV-positive patients with CD4+ T cell count of less than 200 cells/ul were more at risk of opportunistic parasites compared to the HIV-negative controls.
Conclusion
The prevalence of intestinal parasites in newly diagnosed HIV/AIDS individuals was high, and its association with CD4+ T cell count was demonstrated. Routine screening for parasitic infestations at diagnosis is indicated to reduce the burden of the disease.
1 Introduction
Human immune-deficiency virus/acquired immune-deficiency syndrome (HIV/AIDS) is a global public health problem.Citation1 The disease predisposes individuals to various opportunistic infections of which parasitic infestations of the gastrointestinal (GI) tract are prominent.Citation2 Several studies have shown that some intestinal parasites such as Cryptosporidium spp., Cyclospora cayetanensis, Isospora belli, Entamoeba histolytica/dispar, Strongyloides stercoralis, and Giardia lamblia are responsible for 60–80% of infestations.Citation3 Thus infestation of the GI tract by these organisms plays a crucial role in HIV/AIDS pathogenesis, and diarrhoea diseases assume a prominent role reaching up to 50% in developing countries.Citation2 The decrease in immunity by attack on the immune system especially the cluster of differentiation (CD4+ T cells) component, macrophages, and defect in the production of immunoglobulin A (IgA) increases susceptibility to these parasites.Citation4 Gut-associated lymphatic tissue (GALT) in the GI tract is an important site for early HIV replication and CD4+ T cell replication.Citation5
Helper T cells which are very important in adaptive immunity, activate B cells to secrete antibodies, activate macrophages to destroy ingested microbes, and also activate cytotoxic T cells to kill infected target cells. These functions are impaired in patients with HIV/AIDS.Citation6 Furthermore, HIV/AIDS decrease the circulating pool of effector, and memory CD8+ T cells which combat viral infections. The end result is immunosuppression.Citation7 There have been reports of the prevalence of intestinal parasites in HIV/AIDS patients in other parts of Nigeria and the world.Citation8–Citation14 Ibrahim et al.Citation8, and Babatunde et al.Citation9, in North central, Nigeria, found an increase in the prevalence of intestinal parasites in HIV-positive patients compared to HIV-negative controls. Similarly, Akinbo et al.Citation10, Hailemariam et al.Citation11, Alemu et al.Citation12, Jegede et al.Citation13, and Oyedeji et al.Citation14 all found an increase in the prevalence and multiple intestinal parasitosis in HIV-positive Nigerian and Ethiopian patients compared with HIV-negative controls. These studies were mostly on patients already on highly active anti-retroviral therapy (HAART). There is a paucity of data on similar studies on treatment naïve HIV/AIDS patients. It is thus important to find out the common intestinal parasites in newly diagnosed treatment naïve adult HIV/AIDS patients in Ilorin, Nigeria, since these parasites play a prominent role in diarrhoeal diseases, and HIV/AIDS pathogenesis.
This study therefore aimed to determine the prevalence of intestinal parasites in newly-diagnosed treatment naive HIV/AIDS patients.
2 Subjects, materials and methods
The study was a hospital-based cross-sectional study carried out over a six-month period (December 2010–June 2011), at the Infectious disease clinic of University of Ilorin Teaching Hospital (UITH), Ilorin, Nigeria. A standard structured questionnaire was administered to consecutive 238 newly diagnosed treatment naive adult HIV/AIDS patients, and 238 age and sex-matched HIV-negative controls whose blood and stool samples were tested at first enrolment. Individuals who had taken antibiotics, anthelmintic drugs and steroids prior to enrolment were excluded from the study.
2.1 Specimen collection
Blood sample: Ten millilitres of venous blood samples were collected aseptically into labelled EDTA specimen bottles. Rapid Enzyme-linked immunosorbent assay (ELISA) was carried out to detect antibodies to HIV 1 and 2 using rapid ELISA test kit (AcuuBio Tech Co., Ltd., China). CD4+ T cell count was carried out with Partec 4000 cyflow counter Germany (2006) at the HIV laboratory of UITH.Citation15 The range of CD4+ T cell count was classified using the 1993 Center for Disease Control and Prevention USA, immunological criteria.Citation16
Stool sample: Stool samples were collected into sterile containers, labelled, and analysed within 24 h of collection. Stool samples were examined using direct microscopy for wet preparation, and iodine preparation.Citation17,Citation18 Modified Ziehl-Neelsen methods, and Faecal concentration technique (using formol ether concentration method) were also used to increase the yield of intestinal parasites. Positivity of intestinal parasites was taken as the presence of worms, ova, trophozoites, oocysts and cysts in the stool samples.Citation17–Citation19
Data analysis: Epi-info™ version 3.5.1(CDC, USA 2008) software package was used for analysis. Statistical significance was taken as p-value less than 0.05.
Ethical approval was obtained from the Ethics and Research committee of UITH.
3 Results
There were 90 males (37.8%) and 148 females (62.2%) in both groups, with a male to female ratio of 0.6:1. The age range for both groups (HIV-positive subjects and HIV-negative controls) was from 16 to 65 years. The mean age of respondents was 36.1 ± 9.6 years and 35.9 ± 9.4 years for the HIV-positive subjects and HIV-negative controls respectively. The commonest age group was 26–35 years for both HIV-positive subjects and HIV-negative controls. The mean age of the respondents was similar (P > 0.05). Majority of the respondents were married, and secondary school level of education was the highest level of education attained by them. Most of the respondents were of Yoruba ethnic origin, and trading was the major occupation of the HIV-positive subjects, while most of the HIV-negative controls were self-employed ().
Table 1 Socio-demographic characteristics of respondents.
The prevalence of intestinal parasites in HIV-positive subjects and HIV-negative controls was 68.5% and 49.2% respectively. HIV-positive subjects had increased risk of intestinal parasites compared to HIV-negative controls (P < 0.05); OR = 2.25 CI (1.52–3.32).
The most frequently detected parasites in the HIV-positive subjects and HIV-negative controls were Cryptosporidium spp. and C. cayetanensis. These were significantly higher in the HIV-positive subjects than in HIV-negative controls (55% vs 16.8%) (X2 = 73.97: P < 0.05) and (41.2% vs 8.4%) (X2 = 66.81; P < 0.05) respectively. There were no statistically significant differences in the prevalence of I. belli (3.0% vs 0.8%; X2 = 1.81: P > 0.05), E. histolytica (8.4% vs 8.8%) (X2 = 1.0: P > 0.05), G. lamblia (3.7% vs 0%), Hookworm spp. (0% vs 0.8%), S. stercoralis (1.7% vs 0.8%; P > 0.05), Ascaris lumbricoides (2.5% vs 0%), Trichuris trichiura (0.8% vs 0%), Schistosoma mansoni (0.4% vs 0%) in both groups ().
Table 2 Distribution of intestinal parasitic species in respondents.
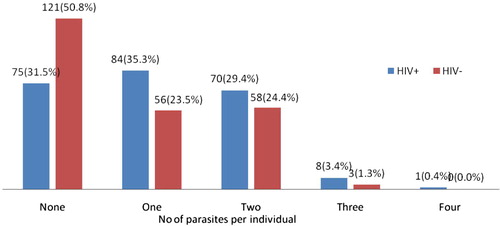
Some respondents were infected with up to four different parasites. HIV-positive subjects had more multiple parasitic infestation rates (more than one) than the HIV-negative controls 33.2% (79/238) and 25.6% (61/238) respectively (X2 = 34.13; P < 0.05) ().
The range of CD4+ T cell count in HIV-positive patients was 13–883 cells/ul. The mean CD4+ T cell count was 257 ± 201.7. HIV-positive patients with CD4+ T cell count <200 cells/ul had increased risk of intestinal parasitic infestation (p = 0.017; OR 1.95: CI = I.09–3.55) compared to those with CD4+ T cell count of 200–499 (p = 0.760; OR = 1.09, CI = 0.59–2.04) and those with CD4+ T cell count >500 (p = 1.00; OR = 0.24, CI = 0.10–0.54) ().
Table 3 Distribution of intestinal parasites in HIV-positive subjects at different values of CD4+ T cell count (cells/ul).
4 Discussion
Intestinal parasites, especially the opportunistic ones are a common cause of morbidity and mortality in HIV/AIDS patients.Citation8 The prevalence of intestinal parasites in HIV-positive subjects in this study was found to be high (68.5%). Studies carried out in other parts of Nigeria showed diversity in findings. The figure of 68.5% is lower than the 87.8% reported in an earlier study carried out in our centre by Babatunde et al.Citation9 Ibrahim et al. in North-central Nigeria, documented a figure of (50.0%).Citation8 Akinbo et al. in South-south Nigeria reported 15.3%.Citation10 This variation in prevalence is not different from that documented in Africa and other parts of the world. Hailemariam et al.Citation11 and Alemu et al.Citation12 in Ethiopia reported a prevalence of 52.6% and 80.3% respectively. Kipyegen et al. in Kenya documented a parasitic prevalence in HIV-positive patients which is to be 50.0%).Citation20
Da silva et al. in Brazil found a prevalence rate of 27.0%.Citation21 Mohandas et al. in India found out that 30.0% of HIV-positive patients harbour intestinal parasites.Citation22
HIV-positive subjects in this study were all newly diagnosed and treatment naïve in contrast to the other studies mentioned above. Furthermore, the study subjects in aforementioned studies, were a combination of those on treatment and treatment naïve. They may have used anthelmintic drugs such as Albendazole, Piperazine, Levamisole, and HAART. This may have boosted their immunity and subsequently altered the intestinal flora in the gut.Citation14 Sampling techniques and observer differences in the examination of stool samples may be another factor responsible for these differences in prevalence even though most of the studies involved the use of direct wet mount, formalin-ether sedimentation concentration, and modified Ziehl Neelsen methods. However, Hailemariam et al.Citation11 did not use Ziehl Neelsen method.
Cryptosporidium spp. was found to be the most predominant intestinal parasite in HIV-positive subjects (55.0%). Studies carried out in Ile-Ife, South-west Nigeria, by Oyedeji et al.Citation14 and Adesiji et al.Citation23 found the most predominant intestinal parasite in HIV-positive subjects to be Cryptosporidium spp. (19.2% and 52.7%), and Thomas et al. in Lagos, South-west Nigeria, documented similar findings.Citation24 However, this is in contrast to the findings by Nwokediuko et al. in Enugu, South-east NigeriaCitation25 and Oyerinde et al. in LagosCitation26, who reported a rarity of Cryptosporidium spp. This is unusual, as Cryptosporidium spp. infection has been documented even in apparently normal individuals by Ikeh et al.Citation27, NwabuisiCitation28, and Banwat et al.Citation29 all in North-central Nigeria. The prevailing environmental conditions may not be favourable for the transmission of these parasites in that part of the country, which may have accounted for the reported low incidence of Cryptosporidium spp. in those regions. These studies were noted to have been carried out on patients with diarrhoea; hence, they may have taken anthelmintic drugs such as Albendazole, Piperazine, and Levamisole prior to enrolment into the studies. The findings of Oyedeji et al.Citation14 were influenced by the prior use of ant-helminthics and Co-trimoxazole. Jegede et al.Citation13 in North central, Nigeria, did not find any statistical difference in the spectrum of intestinal parasites between HIV-positive and HIV-negative controls.
However, studies in Nigeria by Wokem et al.Citation30 and Ethiopia by Hailemariam et al.Citation11 found A. lumbricoides to be the most predominant parasites in HIV-positive subjects. S. stercoralis was found to be most predominant in HIV-positive subjects in Thailand.Citation31 Further studies need to be carried out in those geographical areas to validate these findings as opportunistic parasites are expected to thrive more in HIV-positive patients.
From this study, C. cayetanensis was detected in a significant number of HIV-positive subjects compared to HIV-negative controls (41.2% vs 8.4%). This differs from reports in some parts of Nigeria and the world at large, in which the prevalence was found to be low or undetected.Citation23,Citation24,Citation32,Citation33 The geographical variation and the remarkable similarity in morphologic features with Cryptosporidium spp. could account for these differences. The presence of Cryptosporidium spp. and C. cayetanensis in the HIV-negative controls may be due to the fact that asymptomatic carrier state can occur in immune-competent individuals and they only become symptomatic with diarrhoeal disease, when they become immune-deficient.Citation28,Citation30,Citation34,Citation35 Reports by NwabuisiCitation28 in Ilorin, and Banwat et al.Citation29 in Jos, North-central Nigeria, have shown that infection with Cryptosporidium spp. and C. cayetanensis can occur in immuno-competent individuals. Poor personal, and environmental hygiene which could facilitate transmission of the cyst and ova of parasites may be responsible in this part of the world.
The rate of multiple parasitic infestations was 33.2% and 25.6% in HIV-positive and HIV-negative controls respectively. A report from Jos by Ibrahim et al.Citation8, found multiple parasitic infection rates in HIV-positive subjects to be lower (13%), while Hailemariam et al.Citation11, and Alemu et al. documented a high multiple parasitic infestation rate of 91.3%.Citation12 This may be attributed to depressed immunity in the HIV-positive subjects, which predisposed them to mixed infections including the opportunistic and non-opportunistic parasites.
HIV-positive patients with CD4+ T cell count < 200 cells/ul had increased risk of intestinal parasitic infestation (P < 0.05) compared to those with CD4+ T cell count of >200. Majority of HIV-positive subjects with CD4+ T cell count of <200 cells/ul had more than double the risk of developing diarrhoea (P < 0.05) compared to those with CD4+ T cell count of >200. This is in keeping of reports from earlier studies carried out by Babatunde et al.Citation9, WiwanitkitCitation31 and Assefa et al.Citation32 All these findings have shown that immunity plays a major role in the survival and proliferation of intestinal parasites in HIV-positive patients.
A major limitation in this study, is the fact that other staining techniques such as modified trichome staining technique were not used which could have detected Microsporidia spores.
In conclusion, the prevalence of intestinal parasites in treatment naive adult HIV/AIDS individuals was found to be high. HIV-positive individuals with CD4+ T cell count less than 200 cells/ul were more at risk of infestations with intestinal parasites, and multiple intestinal parasites than those with more than 200 cell/ul. Apparently normal individuals also harbour opportunistic parasites.
Conflict of interest
None.
Source of funding
None
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 6 May 2016
References
- L.O.KallingsThe first postmodern pandemic: 25 years of HIV/AIDSJ Intern Med26332008218243
- S.CimermanB.CimermanD.S.LeviEnteric parasites and AIDSSao Paulo Med J117619997077
- R.C.BolingerT.C.QuinnTropical diseases in the HIV-infected travellerSBroderMeriganJrDBolognesiTextbook of aids medicine1994Williams & WilliamsNew York311322 2nd ed.
- S.OsmanovC.PathouyN.WalkerB.Schward-landerJ.EsparzWHO-UNAIDS network for HIV isolation and characterization. Estimated global distribution and regional spread of HIV-1 genetic subtypes in the year 2000J Acq Immune Def Syndr292002184190
- S.DandekarPathogenesis of HIV in the gastrointestinal tractCurr HIV/AIDS Rep4120071015
- B.AlbertsA.JohnsonJ.LewisM.RaffK.RobertsP.WalkerHelper T cells and lymphocyte activationMolecular biology of the cell4th ed.2002Garland ScienceNew York561562
- N.GulzarK.F.CopelandCD8+ T-cells: function and response to HIV infectionCurr HIV Res2120042337
- A.IbrahimE.IkehA.MaluE.OkekeJ.DamenIntestinal parasitosis in Human Immunodeficiency Virus (HIV) infected adults with chronic diarrhoea at Jos University Teaching Hospital, NigeriaThe Int J Par Dis212007
- S.K.BabatundeA.K.SalamiJ.P.FabiyiO.O.AgbedeO.O.DesaluPrevalence of intestinal parasitic infestations in HIV- seropositive and HIV- seronegative patients in Ilorin, NigeriaAnn Afr Med932010123128
- F.O.AkinboC.E.OkakaR.OmoregiePrevalence of intestinal parasitic infections among HIV patients in Benin city, NigeriaLibyan J Med5201010
- G.HailemariamA.KassuG.AbebeE.AbateD.DamteE.MekonnenIntestinal parasitic infections in HIV/AIDS and HIV- seronegative individuals in a Teaching Hospital in EthiopiaJpn J Infect Dis57220044143
- A.AlemuY.SiferawG.GetnetA.YalewZ.AddisOpportunistic and other intestinal parasites among HIV/AIDS patients attending Gambi higher clinic in Bahir Dar city, North West EthiopiaAsian Pac J Med482011661665
- E.F.JegedeE.T.I.OyeyiA.H.BichiH.A.MbahK.TorpeyPrevalence of intestinal parasites among HIV/AIDS patients attending Infectious Disease Hospital, Kano, NigeriaPan Afr Med J172014295
- O.A.OyedejiE.AdejuyigbeS.O.OninlaA.A.AkindeleS.A.AdedokunE.AgelebeIntestinal parasitoses in HIV infected children in a Nigerian Tertiary HospitalJ Clin Diag Res9112015SC01SC05
- Partec Cyflow. Count of CD+4 cell with cyflow counter and partec CD+4 count essay count kit. Application note on procedures partec code number 05-8401 partec GmbH Germany; 2007.
- Center for Disease Control and PreventionRevised classification system for HIV infection and expanded surveillance classification system case definition for AIDS among adolescence and adultsJAMA26919931993729730
- M.CheesbroughParasitological testsDistrict laboratory practice in tropical countries2nd ed.2005Cambridge University PressCambridge191200
- World Health Organisation. Guidelines on standard operating procedures for laboratory diagnosis of HIV-opportunistic infections, Geneva; 2001.
- D.E.SaidDetection of parasites in commonly consumed raw vegetablesAlexandria J Med482012345352
- C.K.KipyegenR.S.ShivairoR.O.OdhiamoPrevalence of intestinal parasites among HIV patients in Baringo, KenyaPan Afr Med J12201237
- C.V.Da silvaM.S.FarreiraA.S.BorgesJ.M.Costa-CruzIntestinal parasitic infections in HIV/AIDS patients: experience at a teaching hospital in central BrazilScan J Inf Dis3732005211215
- K.MohandasR.SehgalA.SudN.MallaPrevalence of intestinal parasitic pathogens in HIV-positive individuals in Northern IndiaJpn J Infect Dis55320028384
- Y.O.AdesijiR.O.LawalS.S.TaiwoS.A.FayemiwoO.A.AdeyebaCryptosporidiosis in HIV infected patients with diarrhoea in Osun State south-western NigeriaEur J Gen Med432007119122
- Thomas B, Fagbenro-Beyioku AF, Ukegbuy CB. Prevalence of enteric opportunistic pathogens among HIV/AIDS patients in Lagos, Nigeria and comparative assessment of three staining techniques. Int Conf AIDS 2000 July 9–14; 13: abstract no. MoPeB2266.
- S.C.NwokediukoB.J.BojuwoyeB.OnyenekweApparent rarity of cryptosporidium in HIV related diarrhoea in Enugu, NigeriaNig Postgrad Med J9220027073
- J.P.OyerindeT.OdugbemiR.I.BensonA.A.AlongeInvestigation of cryptosporidium in relation to other intestinal parasites at the Lagos university teaching hospital, LagosWest Afr J Med841989264269
- E.I.IkehM.O.ObadofinB.BrindeiroC.BaugherbF.FrostD.VanderjargtIntestinal parasitism in Magama Gumau rural village and Jos township in North Central NigeriaNig Postgrad Med J1442007290295
- C.NwabuisiChildhood cryptosporidiosis and intestinal parasitosis in association with diarrhoea in Kwara State, NigeriaWest Afr J Med202001165184
- E.B.BanwatD.Z.EgahB.A.OnileI.A.AngyoE.S.AuduPrevalence of cryptosporidium infection among under-nourished children in Jos, Central NigeriaNiger Postgrad Med J1020038487
- G.N.WokemC.ChukwuB.C.NwachukwuPrevalence of intestinal parasites seen in HIV sero-positive subjects in Port-Harcourt, Nigeria, NigerJ Parasitol2922008115120
- V.WiwanitkitIntestinal parasitic infections in Thai HIV-infected patients with different immunity statusBMC Gastroenterol12001 3e-pub
- S.AssefaB.ErkoG.MedhenZ.AssefaT.ShimeliIntestinal parasitic infection in relation to HIV, AIDS status, diarrhoea and CD4 cell-countBMC Inf Dis92009155
- O.BrandonosioM.A.MaggiS.PanasoA.LisiIntestinal protozoa in HIV infected patients in Apulia, south ItalyEpidermiol Infect1231999457462
- G.AlakpaA.Fagbenro-BeyiokuS.ClarkeCyclospora cayetanensis in stool submitted to hospitals in LagosInt J Infect Dis642001314317
- M.M.HelmyL.A.RasheedH.C.Abdel-FattahCo-infection with cryptosporidium and cyclospora in immunocompetent and immunocompromised patientsJ Egypt Soc Parasitol3622003613627