Abstract
The high rate of local recurrence is considered the major concern and challenge regarding the surgical treatment of cancer rectum. The target of use of pre-operative neoadjuvant therapy is reducing tumour size and improving its resectability in order to reduce local recurrence risk and improve survival rates.
Plans for management and treatment of locally advanced rectal cancer showed clear changes after use of neoadjuvant therapy. This in turn necessitates accurate evaluation of the tumour parameters before and after use of combined chemotherapy and radiation therapy (CRT).
Aim of study is to assess the initial stage of cancer rectum then its response to neoadjuvant therapy using MRI, prior to operative interference. This is followed by post-operative histo-pathological data correlation.
Methods
This study was conducted on 50 patients. All patients were examined by high-resolution T2-weighted images. Turbo-spin-echo sequences taken in sagittal plane, axial plane perpendicular to tumor axis and coronal plane parallel to tumor axis or anal canal. All are according to tumor height. Diffusion weighted images (DWI) performed in all cases.
Results
Following neoadjuvant therapy, down-staging was detected in this study in more than 90% of patients regarding the T2 signal and apparent diffusion coefficient (ADC) value of the tumour, also status of depth of involvement of meso-rectal fascia (MRF), circumferential resection margin (CRM), extra-mural vascular invasion (EMVI) and nodal involvement.
Conclusion
Pre-operative MRI in cancer rectum is irreplaceable to assess initial staging and post-neoadjuvant therapy response thus improving surgical results.
1 Introduction
The high rate of local recurrence is considered the major concern and challenge regarding the surgical treatment of cancer rectum. The target of use of pre-operative neoadjuvant therapy is reducing tumour size and improving its resectability in order to reduce local recurrence risk and improve survival rates.Citation1
Plans for management and treatment of locally advanced rectal cancer showed clear changes after use of neoadjuvant therapy. This in turn necessitates accurate evaluation of the tumour parameters before and after use of combined chemotherapy and radiation therapy (CRT).Citation2
1.1 Tissue characteristics
On T2WI, the viable tumour tissue exhibits typically intermediate signal intensity; that is expressing the signal intensity between the muscularis propria and mucosa.Citation3 Rectal mucinous adenocarcinoma (RMAC) is admixed with areas of high SI of mucin.Citation4
DWI-MRI plays an important role in visual identification of the tumour based on high signal intensity and also quantitative data based on tissue cellularity of which based on low ADC value. Also the ADC value has an established role in evaluation and monitoring of tumour tissue response following neo-adjuvant therapy.Citation5
1.2 Distal resectability
According to the distance of the lowest edge of the tumour from the anal verge which is considered to be useful reference point for the surgeons, the height of the tumour is described and classified as upper, middle and lower rectal tumors.Citation6
Initial pre-treatment MRI in rectal cancer must define the status of the sphincteric complex in low rectal tumours, whether it's invaded or not. Following CRT, abdomino-perineal resection procedures can be replaced with ultralow resection followed by colo-anal anastomosis.Citation7
1.3 Circumferential resectability
Staging of rectal cancer using MRI is precisely based on identification of T2 signal intensity differences between the tumour, sub-mucosa, muscular layer, and meso-rectum.Citation7 According to the extra-mural depth of tumour spread beyond muscular propria into meso-rectal fat, the more recent rectal cancer staging from the American Joint Committee on Cancer (2010) and MR imaging classification proposed by Smith and brown concerned T3 tumours sub-classification.Citation7 Smith and brown TNM staging.
Further specific T staging for low rectal tumours is performed using evaluation of the coronal T2-weighted images.Citation9 Ano-rectal staging.
Evaluation of the mesorectal nodes, nodules as well as extramesorectal adenopathies: It is essential to define any suspicious regional pelvic lateral side wall lymph node and describe its exact location, number, size and shape in T2WI. Also detection of any other non-regional extra-mesorectal nodes is essential (considered as M1) including common and external iliac nodes, para-aortic nodes, obturator nodes and lastly inguinal nodes in low rectal tumors.Citation10
Extramural vascular invasion (EMVI): Presence of malignant cells in the meso-rectal fat blood vessels beyond the muscularis propria refers so as to be EMVI.Citation11
Circumferential resection margin (CRM) and Distance from mesorectal fascia (MRF): Any tumour lying within 1 mm of MRF is considered positive CRM. It is essential to describe its location precisely using axial T2WI in clock wise direction.Citation12
Desmoplastic reaction: This can be defined by the presence of any low T2 signal tumor speculations projecting into meso-rectal fat.Citation11
Evaluation of anterior peritoneal reflection: It is essential to describe relation of the tumour tissue (mainly middle and upper rectal neoplasms) to anterior peritoneal reflection. Invasion of which is considered T4a tumour and carries high rate of recurrence.Citation11
Evaluation of pelvic side wall and other pelvic organs: It is essential also to depict any invasion of the pelvic organs which is considered as T4b tumor. Urinary bladder and uterus can be invaded in cased of upper or middle rectal neoplasms. While lower rectal tumours can invade the levator muscles, the prostate, the vagina, the seminal vesicles, the sacrum, and coccyx.Citation3,Citation6
1.4 Post neoadjuvant CRT MRI changes and tumour regression grading (TRG)
Schematic presentation of MRI tumour regression grading (TRG) was performed based on tumour volume and changes of T2 signal with either low signal depicting tumour fibrosis or high signal depicting mucin.Citation11 Dworak Tumor regression grade.
It is essential to detect any morphologic changes following CRT regarding the tumour, rectal wall, tumour-mesorectal fat interface, metastatic lymph nodes and EMVI. These morphological changes could be either due to fibrosis, mucin production or colloid response. Also it is important to depict the inflammatory morphological changes including sub-mucosal edema, tissue necrosis and pseudo-tumour.Citation13
2 Aim of the work
To assess to the initial stage of cancer rectum then its response to neoadjuvant therapy using MRI, prior to operative interference. This is followed by post-operative histo-pathological data correlation.
3 Patients and methods:
This retrospective study included 50 patients with rectal carcinoma. All patients were imaged using external phased array surface coils on 1.5 T superconducting magnet MRI machines including 2 patients imaged by Philips Gyroscan Intera (Best, The Netherlands), 2 patients imaged by GE Signa HDxt (Milwaukee, USA) and 46 patients imaged by Siemens Magnetom Avanto (Erlangen, Germany).
This study was limited to patients having rectal cancer diagnosed by either CT colonography or endoscopy and histopathology.
High-resolution T2-weighted images were obtained using non-breath hold turbo-spin-echo sequence. According to tumour height, all planes were examined including; sagittal plane, axial plane perpendicular to tumor axis, coronal plane parallel to tumor axis or anal canal. Diffusion weighted images (DWI) were also obtained in the axial plane. Rectal luminal distension using sonographic gel done when needed in some cases.
A post neoadjuvant therapy follow up MRI study was performed in all patients after 6–8 weeks (with the same above mentioned sequences).
Correlation with histo-pathological data carried out after the surgical management.
Rectal cancer patients without the pre neoadjuvant therapy MRI examinations were excluded from the study as adequate assessment of response to neoadjuvant therapy will be limited.
4 Results
4.1 Initial pre-neoadjuvant therapy staging of the tumor
The present work included 50 patients presented with rectal carcinoma. They were 23 males and 27 females with near ratio 0.46:0.54 respectively. Their ages ranged between 20 and 80 years with a mean age of 50 years. The peak age was targeting the 7th decade. All patients considered the examination acceptable, with no discomfort or complications reported.
Around 94% of these patients complained from bleeding per-rectum while 86% of them complained also from altered bowel habits. 70% of patients showed generalized symptoms of cachexia. Abdominal pain was present in 32% of patients. None of these patients presented by intestinal obstruction or distant organs metastatic lesions of unknown primary.
According to distance of the lower border of the tumour from ano-rectal junction (ARJ); tumour location is categorized into either upper rectal neoplasm (>10 cm), middle rectal neoplasm (5–10 cm), lower rectal neoplasm (<5 cm), widespread upper and middle involvement, widespread middle and lower involvement) and diffuse ano-rectal involvement ().
Table 1 Distribution of patients according to location of the tumour.
Initial TNM staging of the tumour was performed in all patients ().
Table 2 Distribution of patients according to initial TNM staging.
Regarding (nodes-N); 43 patients showed suspicious metastatic nodes. All of them exceeds 5 mm in short axis diameter. 36 patients of them showed irregular contour and internal necrosis.
Regarding (metastasis-M) determined by presence or absence non-regional metastatic nodes or mesenteric soft tissue masses: Stage M1 was depicted in five patients (10%), four of them with non-regional metastatic looking lymph nodes.
Ano-rectal tumours were specifically staged into stage I to IV ().
Table 3 Distribution and initial specific staging of patients with ano-rectal tumors.
Low T2 signal of the tumour was found in four patients, while intermediate signal was found in 40 patients, high and mixed signals were found in three patients each. ADC value of the tumour found to be ranging from 0.4 to 1 × 10−3 mm2/s with mean value 0.7 × 10−3 mm2/s.
Sphincteric mechanism was intact in 30 patients. Invasion of internal sphincter only found in nine patients. Invasion of internal sphincter and IP was found in four patients. While invasion of both external and internal sphincters was found in seven patients. CRM was positive in 28 patients and negative in 22 patients ().
Table 4 Distribution of patients according to initial status of sphincteric mechanism.
Only five patients showed negative involvement of the MRF while 45 patients showed positive involvement; 39 patients showed positive MRF depth of involvement via nodal lesions, 15 patients showed positive MRF depth of involvement and positive EMVI, only eight patients showed initial invasion of the anterior peritoneal reflections, also only seven patients showed initial invasion of the surrounding viscera ().
Table 5 Distribution of patients according to MRI detailed characteristics of positive MRF involvement.
13 patients initially had suspicious extra-mesorectal adenopathies. Nine patients showed only regional extra-mesorectal suspicious adenopathies. While four patients showed mixed regional and non-regional extra-mesorectal suspicious adenopathies. Regional nodes included inferior mesenteric artery (IMA) nodes and internal iliac nodes while the none-regional nodes included external iliac nodes, obturator nodes, inguinal nodes and para-aortic nodes (see –).
Fig. 1 (Initial MRI study): A 62 years old male patient presented with bleeding per rectum and the PR examination revealed a rectal mass. MRI study with rectal distension using sonographic gel; (a) and (b) Sagittal high resolution T2WIs showing the lower rectal mass lesion (red arrows) about 3.5 cm from the anal verge. (c) and (d) Axial high resolution T2WIs showing the rectal mass with intermediate signal intensity extending from 9 to 3o'clock, no extension beyond the muscularis propria with implication of the internal sphincter from 11 to 1o'clock (green arrow). (e) Coronal high resolution T2WI showing extension 8 mm below puborectalis sling. (f) ADC map showing hypointense signal of the rectal mass denoting restricted diffusion (0.8 × 10−3 mm2/s). The preliminary imaging based staging was c T2 N0.
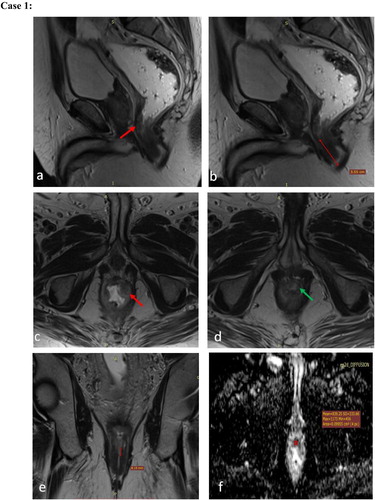
Fig. 2 (Post-neoadjuvant therapy MRI study): for the same patient after 5?months showed a non-responding lower rectal mass lesion with same tissue characteristics at T2WI and ADC maps, same dimensions and distal resectability features; resulting in TRG 5 and imaging based staging yc T2N0. Post CRT MRI study. (a) Sagittal high resolution T2WI and (b) ADC map showing the lower rectal mass lesion with the intermediate T2 signal (red arrow in a) and ADC values about 0.8?×?10−3?mm2/s denoting restricted diffusion. The patient performed abdominoperineal resection with the post-operative histopathology revealed a moderately differentiated rectal adenocarcinoma, 10 out of 10 nodes excised was free, margins free.
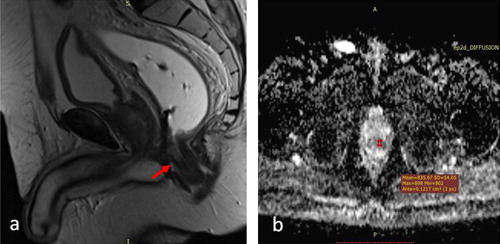
Fig. 3 (Initial MRI study): A 66?years old male patient diagnosed as rectal mass and referred from the oncology department for initial staging. MRI study; (a) and (b) Sagittal high resolution T2WIs, (c) and (d) axial high resolution T2WIs, (e) Coronal and (f) Axial high resolution T2WIs, (g) and (h) DWI and ADC maps showing a low third rectal mass lesion with intermediate SI, about 2.7?cm from the anal verge, crossing the puborectal sling by 7?mm, involving the four quadrants circumferentially with focal interruption of the musculosa at 9o'clock (red arrow in c) and implication of the upper 7?mm of the internal sphincters from 11 to 1o'clock (green arrows in d). An extramesorectal regional right internal iliac suspicious node is noted (blue arrow in f). Resticted diffusion was noted at DWI with ADC values about 0.8?×?10−3?mm2/s. The preliminary imaging based staging is cT3a (below APR, CRM−ve) Nx, stage 2 anal complex invasion.
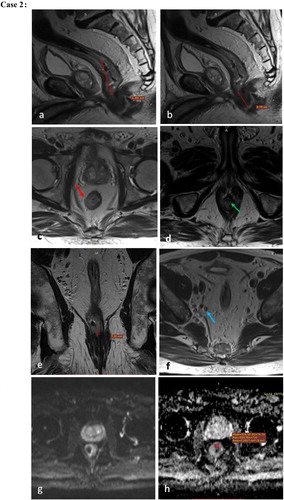
Fig. 4 (Post-neoadjuvant therapy MRI study): after 4?months revealed marked therapeutic Response (TRG?=?2: Dense fibrosis with absent or minimal residual disease). Spared sphincters. The preliminary imaging based staging is yc T0-2N0. MRI study with rectal distension using sonographic gel. (a) Sagittal high resolution T2WI, (b) and (d) Axial high resolution T2WIs, (c) Coronal high resolution T2WI, (e) and (f) DWI and ADC maps showing the lower third rectal lesion currently displaying low SI at T2WI denoting fibrosis, 6?cm from the anal verge, involving three quadrants circumferentially (red arrow in b) with no implication of the anal sphincteric complex (best depicted in c). The pathologically enlarged nodes. DWI showed no restriction. The patient performed low anterior resection (LAR) with the histopathology revealed moderately differentiated rectal adenocarcinoma, Mandrad grade 2 with 7 out of 7 nodes excised free, margins free and donuts free.
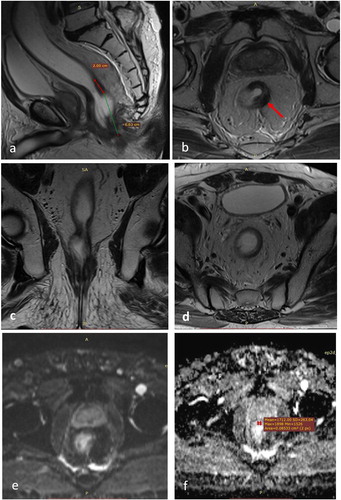
Fig. 5 (Initial MRI study): A 67?years old male patient presented with bleeding per rectum and diagnosed as rectal mass by endoscopy. Initial MRI study; (a) and (b) Sagittal high resolution T2WI, (c) and (d) axial high resolution T2WI, (e) and (f) DWI and ADC maps showing an upper rectal mass lesion, opposite to the spared APR (yellow arrow in b), about 3?cm in maximum length, 10.8?cm from the anal verge and 5.6?cm from the puborectalis sling, extending circumferentially from 7 to 12o'clock with 4?mm extramural depth of invasion (EMDI) beyond the muscularis propria into mesorectal fat. Restricted diffusion is seen in DWI with hyperintense signal and ADC values about 0.8?×?10−3?mm2/s. The preliminary imaging based staging is c T3b Nx. Opposite to APR and CRM spared.
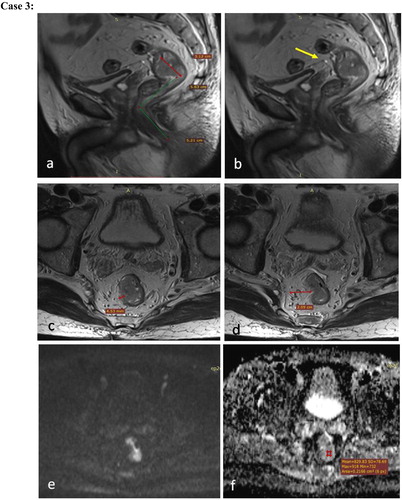
Fig. 6 (Post-neoadjuvant therapy MRI study): The post-neoadjuvant CRT MRI study after 4?months revealed partially responding upper third rectal neoplasm (TRG?=?3). The preliminary imaging based staging is yc T1 or T2 N0. Post neoadjuvant MRI study; (a) and (b) Sagittal and axial high resolution T2WI respectively, (c) and (d) DWI and ADC maps showing the previously noted upper rectal mass lesion, currently regressed in size about 2?cm in maximum length and 8.7?mm in maximum thickness, extending from circumferentially from 7 to 9o'clock with no evident of EMDI at current study, foci of restricted diffusion was seen with ADC values about 0.8?×?10−3?mm2/s. The patient performed left hemicolectomy with low anterior resection. The post-operative histopathology revealed moderately differentiated rectal adenocarcinoma, with 14 out of 14 nodes excised were free, margins free.

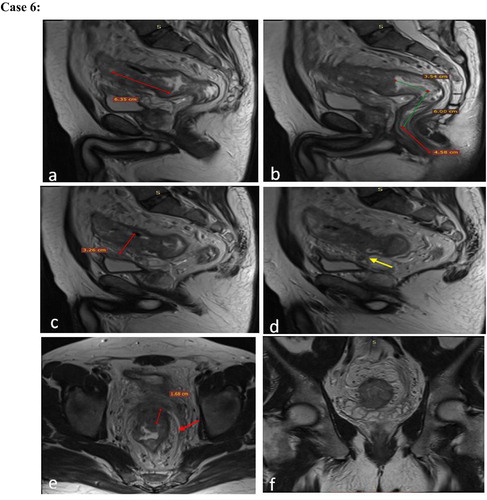
Fig. 7 (Initial MRI study): A 51?years old female patient diagnosed as rectal mass and referred from the oncology department for initial staging. Initial MRI with rectal distension using sonographic gel. (a) Sagittal high resolution T2WI, (b), (c) and (e) Axial high resolution T2WI, (d), (f) Coronal high resolution T2WI, (g) and (h) DWI and ADC maps showing an upper rectal mass lesion, about 5?cm in maximum length, 10?cm from the anal verge, showing intermediate signal intensity with involvement of the four quadrant of the rectal wall circumferentially. EMDI is noted all around the rectal wall with about 2?mm from the MRF at 8o'clock (red arrow in b). Suspected EMVI is noted at 9o'clock (yellow arrow in c). Multiple mesorectal adenopathies were seen (blue arrow in c, d, e) around the tumor and averaging 6?mm in size with some abutting the mesorectal fascia (red arrow in e). Inferior mesenteric extramesorectal regional node was seen, averaging 7?mm im size (green arrow in f). Restricted diffusion noted with ADC about 0.8?×?10−3?mm2/s. Preliminary imaging based staging is c T3c N2b (CRM+).
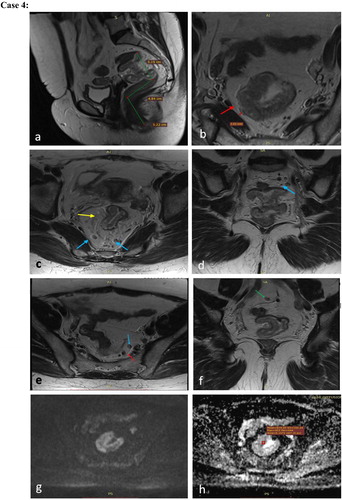
Fig. 8 (Post-neoadjuvant therapy MRI study): Post neoadjuvant CRT MRI study after 4?months revealed complete radiological response (TRG 1) yc T0-2N0. Post neoadjuvant CRT MRI with rectal distension using sonographic gel. (a), (b) and (c) Sagittal, coronal and axial high resolution T2WIs respectively showing complete response of the rectal mass lesion with no EMDI, EMVI or pathologically enlarged mesorectal nodes noted. The patient performed low anterior resection (LAR) with post-operative histopathology revealed a moderately differentiated rectal adenocarcinoma with Mandrad grade 1, 10 out of 10 nodes excised were free, Donuts free and margins free.
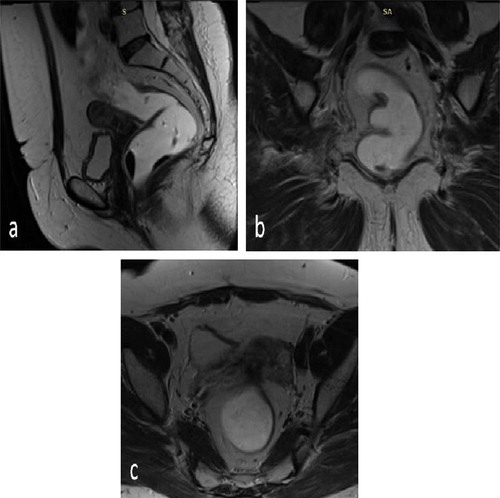
Fig. 9 (Initial MRI study): A 49?years old male patient diagnosed as rectal mass and referred from the oncology department for initial staging. Initial MRI study; (a) and (g) Sagittal high resolution T2WI, (b) through (f) Axial high resolution T2WI, (h) ADC maps showing a middle third rectal mass lesion, about 7.5?cm in maximum length, 7.8?cm from the anal verge, showing internal signal mixed with areas of cystic necrosis, involving four quadrants circumferentially; from 10 to 7o'clock. Sizable EMDI was seen with exophytic lesion about 3.2?cm in size extending from 2 to 5o'clock and invading the MRF (red arrow in b). EMVI noted at 4o'clock (yellow arrow in c). Multiple mesorectal adenopathies noted (blue arrow in d) abutting the MRF at 7o'clock (red arrow in d). Multiple extra mesorectal inferior mesenteric nodes were seen (orange arrow in e and f). The APR was noted at the upper edge of the tumor, yet not infiltrated (pink arrow in g). Restricted diffusion with ADC values about 0.8?×?10−3?mm2/s seen. The preliminary imaging based staging is c T3d N2, below APF, CRM involved.
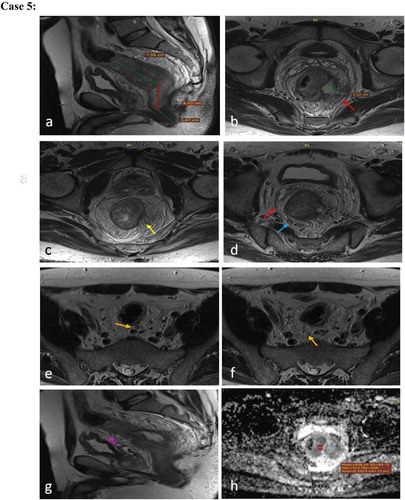
Fig. 10 (Post neoadjuvant therapy MRI): Post neoadjuvant CRT MRI study after 4?months revealed markedly responding middle rectal mass lesion …Markedly responding middle third rectal mass (TRG 2), −ve CRM, preliminary imaging based staging yc T0-2N0 Mx. Post neoadjuvant MRI study; (a) Sagittal high resolution T2WI, (b), (c) and (d) Axial high resolution T2WI, (e) and (f) DWI and ADC maps showing markedly responding middle rectal mass lesion, about 4?cm in length, 11?cm from the anorectal junction, showing predominantly hypointense SI denoting fibrotic response. The previously noted EMDI replaced by hypointense fibrotic strands (blue arrow in d), contiguous with MRF (red arrow in c). No definite diffusion restriction with ADC values 1?×?10−3?mm2/s. The patient performed total mesorectal excision (TME) with post-operative histopathology revealed a moderately differentiated rectal adenocarcinoma, 8 out of 8 nodes excised were free with fibrotic strands, Donuts free, margins free.
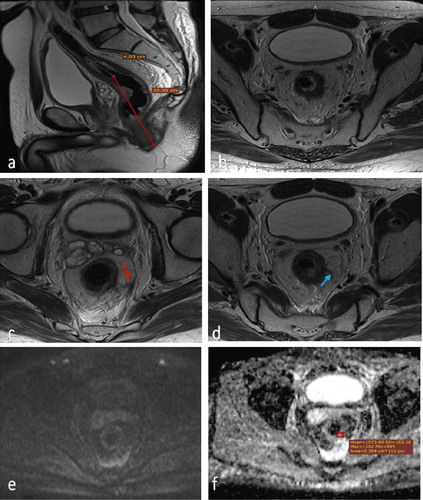
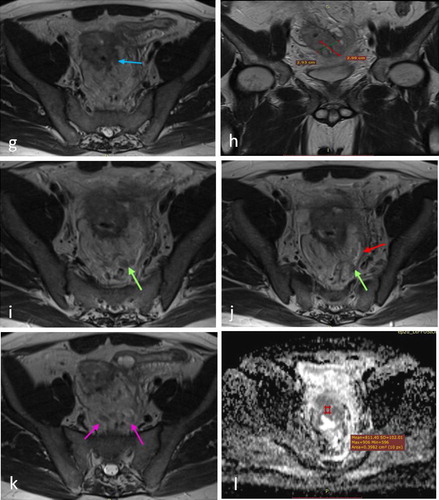
Fig. 11 (Initial MRI study): A 54?years old male patient presented with bleeding per rectum and diagnosed as rectal mass by endoscopy. Initial MRI study with rectal distension using sonographic gel; (a) through (d) Sagittal high resolution T2WI, (e), (g), (i), (j) and (k) Axial high resolution T2WI, (f) and (h) Coronal high resolution T2WI, (l) ADC maps all showing a rectosigmoid mass lesion, about 6.3?cm in maximum length, 3.2?cm in maximum thickness, about 14?cm from the anal verge, showing intermediate SI, its upper 2/3 involving the rectal wall circumferentially while its lower third involving the rectal wall from 8 to 4o'clock. EMDI was noted at lower third about 16?mm beyond the MP with invasion of the MRF (best depicted in e and f). Its upper 2/3 was associated with extramural component about 3?×?3 cm in size infiltrating the APR which was seen thickened (yellow arrow in d). EMVI was noted at 5o'clock (blue arrow in g). Multiple mesorectal (green arrows in i and j) and inferior mesenteric (pink arrow in k) adenopathies were noted, some abutting the MRF (red arrow in j). Resticted diffusion was noted with ADC values about 0.8?×?10−3?mm2/s. Preliminary imaging based staging T4a N2 Mx, +ve CRM, infiltrated APR.
Fig. 12 (Post neoadjuvant therapy MRI): after 2?months revealed moderately responding rectosigmoid mass (TRG 3) with infiltrated APR, +CRM, preliminary imaging based staging T4a N2 Mx. MRI study with rectal distension using sonographic gel. (a) and (b) Sagittal high resolution T2WI, (c), (f) and (g) Axial high resolution T2WI, (d) and (e) Coronal high resolution T2WI, (h) ADC maps all showing moderately responding rectosigmoid mass lesion, still averaging 6?cm in length and 14?cm from the anal verge, but its maximum thickness regressed to 1.6?cm. it showed mixed intermediate and hypointense signal denoting fibrotic changes. The EMDI noted at its lower third regressed to 8?mm with multiple fibrotic strands contiguous with the MRF (red arrow in c); best depicted in c and d. Regression of the extramural component at its upper 2/3 was noted as well, averaging 2?×?1?cm in size still infiltrating the APR (best depicted in e). Regression in size of the inferior mesenteric (yellow arrow in f) and mesorectal adenopathies (green arrow in g) were seen; with distance from MRF about 2?mm. Small foci of restricted diffusion were noted with ADC values about 0.9?×?10−3?mm2/s. The patient performed trans-sphincteric resection with coloanal anastomosis, the post-operative histopathology revealed a moderately differentiated rectal adenocarcinoma, 8 out of 12 nodes excised showed malignant cells, −ve EMVI with margins free.
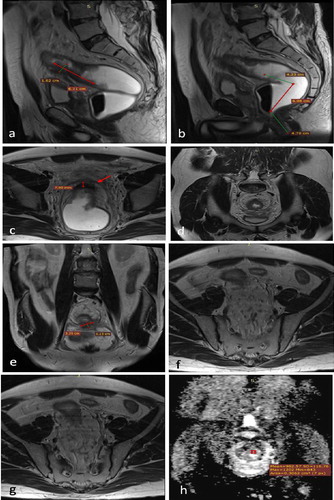
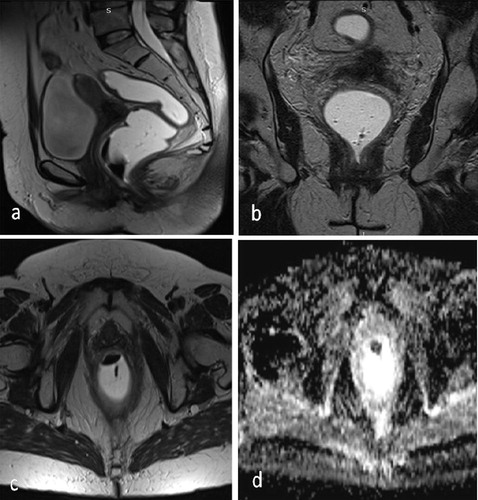
Fig. 13 (Initial MRI study): A 59?years old female patient presented with bleeding per rectum and diagnosed as rectal mass by endoscopy. Initial MRI study with rectal distension using sonographic gel. (a) Sagittal high resolution T2WI, (b) Coronal high resolution T2WI, (c) and (d) Axial high resolution T2WI, (e) and (f) DWI and ADC maps showing a lower rectal and upper anal mass lesion, about 5.3?cm in length, 3?cm in maximum thickness and about 3.3?cm from the anal verge with intermediate T2IW SI. Suspected infiltration of the puborectalis on the right side (9o'clock) was noted (yellow arrow in b). Infiltration of the rectal wall anteriorly was noted opposite to 10–11o'clock with loss of fat plane between the lesion and the posterior vaginal wall raising the possibility of local infiltration (red arrows in c). A mesorectal node showing low signal but suspicious spiculations of its contours was seen at 11o'clock (blue arrow in d). Restricted diffusion was depicted with ADC values about 0.6?×?10−3?mm2/s. The preliminary imaging based staging is c T4b N2.
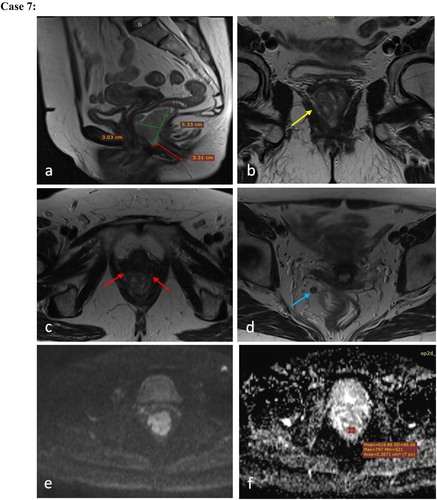
Fig. 14 (Post neoadjuvant therapy MRI): Post neoadjuvant CRT MRI study after 3 months revealed: …Complete radiologic response. No evidence of residual tumor on imaging basis: Grade 1 tumor regression grade. Imaging based staging yc T0-2N0. Post neoadjuvant MRI study with rectal distension using sonographic gel. (a), (b) and (c) Sagittal, Coronal and Axial high resolution T2WI respectively (d) ADC maps all showing total resolution of the rectal mass lesion with no suspicious adenopathies, areas of diffusion restriction or pelvic organ infiltration. The patient performed abdomino perineal resection with the post-operative histopathology revealed moderately differentiated rectal adenocarcinoma, Perineal invasion +ve, 2 out of 9 nodes excised showed malignant cells, EMVI −ve, circumferential resection margin free.
4.2 Following neoadjuvant therapy staging of the tumor
Regarding tumour regression grade (TRG): according to TRG; down staging was classified into five categories. 41 patients (after first course of neoadjuvant therapy) and overall 45 patients (after additional clinically indicated course) that showed TRG1,2&3 expressed significant elevation of the ADC value. 13 patients of them showed no tumor. 16 patients of them showed pure low T2 signal due to post-management fibrotic changes. 12 patients showed mixed low T2 signal of the fibrotic response and intermediate signal of the residual tumor, 3 patients showed high T2 signal due to edema and mucinous changes, meanwhile 1 patient showed mixed low and high T2 signal. Further neo-adjuvant therapy sessions were clinically indicated and prescribed for two patients with TRG4 and four patients with TRG5 ().
Table 6 Distribution of patients according to TRG (tumour response after initial and further indicated post-Neoadjuvant therapy).
ADC value of the tumour found to be ranging from 1 to 1.2 × 10−3 mm2/s in 45 patients with mean value 1.1 × 10−3 mm2/s.
Regarding nodal disease; five patients showed stationary nodal disease, 12 patients showed regressive course while 26 patients showed totally resolved previous nodes, confirmed by DWI.
Regarding extra-mesorectal nodes; five patients with suspicious extra-mesorectal adenopathies showed stationary nodal disease, two patients showed regressive course while six patients showed totally resolved previous nodes.
Regarding CRM; five patients showed persistent positive CRM (three of them showed local recurrence and distant omento-peritoneal spread with high morbidity in further post-operative follow up CT studies) while 45 patients showed negative CRM.
Regarding EMVI; four patients showed persistent positive EMVI while 46 patients showed negative EMVI.
Regarding status of surrounding viscera; three patients showed persistent positive invasion of the surrounding viscera while 47 patients showed clear fat plane of cleavage ().
Table 7 Distribution of patients according to post-Neoadjuvant therapy response.
Types of operations: According to surgical management and choice of operations; LAR was performed in 18 patients, while left hemi-colectomy and LAR were done to seven patients, trans-sphincteric procedure done to one patient, TME done to ten patients and APR done to 14 patients.
4.3 Correlation to post-operative histo-pathological laboratory results
Nine patients showed positive nodal disease; only seven of them were reported positive in MRI. Four patients showed positive extra-mesorectal adenopathies (all reported positive in MRI. Only two patients showed positive resection margin while 48 patients showed negative resection. Four patients showed positive EMVI (three of them were positive in MRI and one not). Only two patients showed positive invasion of the surrounding viscera (both reported in MRI).
4.4 Statistical analysis following correlation of post-neoadjuvant MRI findings and post-operative histo-pathological laboratory data
MRI showed high specificity for detection of EMVI and invasion of surrounding viscera and high sensitivity for detection invasion of surrounding viscera, meanwhile it showed moderate sensitivity for detection of EMVI, also moderate specificity and sensitivity for detection of nodal response ().
Table 8 Sensitivity, specificity and predictive values of the MRI:
5 Discussion
Keeping with Taylor,Citation6 localized affection of either upper, middle or lower thirds of the rectum was found in this study in 44% of patients, while 56% of our patients showed widespread involvement of different parts of the rectum and 42% of patients that showed diffuse ano-rectal involvement.
Also keeping with Smith & Brown who had described in details the TNM staging of cancer rectum Citation6 and regarding the tumour (T) of the TNM staging; T2, 3 and 4 stages were included in this study. T3c stage was predominant, seen in 30% of our patients. N0, 1 and 2 stages were also included in this study; N2b stage was predominant seen in 58% of our patients.
21 patients in this study that showed diffuse ano-rectal involvement had further staging and 42.9% of them showed stage 4. Initially intact sphincteric mechanism was seen in 60% of patients while isolated internal sphincteric involvement (stage 1,2) was seen in 18% of patients, involvement of the internal sphincter and inter-sphincteric plane (stage 3) was seen in 8% of patients and deep involvement of both internal and external sphincters (stage 4) was seen in 14% of patients. This was totally keeping with Shihab Citation9 who described the further staging of ano-rectal carcinoma with stage III depicts invasion of more than 1 mm of the inter-sphincteric space and stage IV means invasion of the external sphincter or beyond.
90% of patients in this study showed negative metastatic surveillance (M0), while 10% showed positive metastatic disease (M1) seen in five patients; four of them depicted by non-regional extra-mesorectal metastatic nodes including external iliac nodes, obturator, inguinal and para-aortic nodes (each depicted in one patient). In our study, the morphology of the affected nodes was more important than their size. 83% of patients with affected nodes showed irregular speculated contours with internal necrotic foci, while all patients showed increase in their size (>5 mm). These signs were seen in both the regional meso-rectal as well as extra-mesorectal adenopathies. According to Allen,Citation14 the regional nodal spread in cancer rectum to involve; superior, middle, inferior and peri-rectal, pre and lateral sacral, sigmoid and inferior mesenteric as well as internal iliac nodes. Other nodes are considered non-regional and metastatic.
In this study, initially intermediate T2 signal of the tumour was predominant seen in 80% of patients. While initially low ADC value of the tumour ranging from 0.4 to 1 × 10−3 mm2/s was also characteristic (mean = 0.7 × 10−3 mm2/s). ChunCitation3 had also described that viable rectal tumour initially exhibit intermediate T2 signal between the signal intensity of the muscularis propria and mucosa.
Extramural depth of invasion (EMDI) was assessed in our study according to the classification of T3 tumours to T3a, T3b, T3c and T3d with or without implication of meso-rectal fascia by the rectal wall tumour itself. EMDI was identified by the extension of the intermediate signal intensity of the tumour beyond the outer low signal intensity layer of the muscularis propria within the hyper-intense meso-rectal fat. Associated desmoplastic reaction was described in some of the cases in our study as hypo-intense speculations around the rectal wall tumour within the meso-rectal fat with accurate clock wise description mentioned.
In this study: Initially positive MRF depth of involvement was seen in 90%; 86.7% of them showing positive nodal involvement, only 33.3% showing positive EMVI. Invasion of the anterior peritoneal reflection was depicted only in 16% of our patients and invasion of the surrounding viscera was depicted only in 14%. Finally at initial pre-management evaluation, 56% of patients showed initially positive CRM while 44% were negative.
Extramural vascular invasion (EMVI) is an important independent risk factor for local and distant recurrence and was seen mostly associated with T3 tumours in our study. Normally the meso-rectal vein was seen as fine linear hypo-intensities within the meso-rectal fat all around the rectal wall. In our study EMVI was identified by the expansion of meso-rectal veins with the intermediate signal intensity of the rectal mass. Nodularity of the affected vein was seen in more severe cases denoting invasion beyond the wall of the affected veins resulting in the so called “tumour deposits” within the meso-rectal fat.
Distance of the rectal wall tumour or the EMVI or enlarged meso-rectal nodes from the meso-rectal fascia is important dependent factor for operative decision i.e either sphincter saving procedures would be accomplished or not because the meso-rectal fascia is considered as the surgical circumferential resection margin (CRM) for the total meso-rectal excision (TME) which is an important part of the recent advances in the rectal cancer surgeries. The circumferential resection margin (CRM) was said to be involved or positive if tumoral tissue (either from the rectal wall its self or EMVI or enlarged meso-rectal nodes) seen within 1 mm from the meso-rectal fat. Positive CRM was described in all of the cases in our study, both in the initial and post neoadjuvant CRT MRI studies.
The anterior peritoneal reflection (APR) is an important entity to be commented upon while assessing a case of rectal cancer as its affection denoted T4a rectal tumours. It was identified as thin linear hypo-intensity extending from the upper posterior border of the urinary bladder dome to the junction of the upper two third and lower third of the rectum. In females, it had a variable attachment; may be as low as 5 cm from the anal verge. In our study, it was said to be affected if thick linear hypo-intensity was seen at the anatomical site of the APR in the initial pre-neoadjuvant MRI study. Its assessment in the post-neoadjuvant studies was done in all of our cases to compare the status of its affection to the initial study or whether post-irradiation changes had occurred, seen as De novo hypo-intense thickening of the APF together with the hypo-intense fibrotic response of the tumor.
Invasion of the surrounding viscera is an important entity to be assessed in every case of rectal cancer as their affection denoting T4b rectal tumours and requires additional interference of the gynaecology or the surgical urology staff during the rectal cancer procedure. This detailed and concluded evaluation at our pre-management MRI assessment is keeping with statement of MERCURY study groupCitation15 who reported that clearance or involvement of the surgical resection margin could be accurately performed using high resolution MRI.
Following neo-adjuvant therapy, down-staging took place in more than 90% of patients in this study. TRG2&3 was predominant, each seen in 32% of patients, both showing either low T2 signal of the tumour because of fibrosis or high T2 signal of the tumour because of edema, also both showing relative elevation of the ADC value and relative non-restriction. 26% of patients showed TRG1 and only 10% showed minimal or no improvements (TRG4&5). Describing the response of the rectal wall tumour to the neoadjuvant therapy in our study, the rectal wall tumours either showed total resolution with no evidence of rectal wall tumour or hypo-intense signal replacing the intermediate SI denoting fibrotic response; associated with thick hypo-intense scarring contiguous with meso-rectal fascia or thin linear fibrotic reaction within the meso-rectal fat. Colloid or mucinous response of the rectal mass lesion was seen all well.
This study showed significant relation between elevation of the ADC value of the tumour denoting relative non-restriction (ranging 1–1.2 × 10−3 mm2/s, with mean value 1.1 × 10−3 mm2/s) and degree of tumour response to CRT and this is totally keeping with KimCitation16 who concluded that adding DWI to conventional MRI is important to increase accuracy of evaluation of post CRT tumour response and also keeping with NougaretCitation2 who confirmed the above mentioned relation and in addition they use single-section ROI method and histogram analysis to decreased routine measurements bias. SunCitation17 also clarify that DWI importance is also extending to involve detection of response as early as possible. Also BlazicCitation5 who stated that post-CRT evaluation of the ADC value should extend to involve the whole volume including areas of necrosis and fibrosis in order to verify the complete response of the tumour.
Regarding the overall nodal response following neo-adjuvant therapy in this study, we found total resolution of affected nodes in 60.5% of patients, size regression in 27.9% while only five patients showed stationary course (11.6%). Van HeeswijkCitation18 stated that DWI is a reliable method for assessment of nodal involvement in rectal cancer patients and DWI free image from nodal involvement could be accurately used to diagnose nodal free status (N0).
Regarding the extra-mesorectal nodal response following neo-adjuvant therapy among the affected 13 patients in this study, we found total resolution of affected nodes in six patients in DWI (46.2%), size regression in two patients (15.4%) while only five patients showed stationary course (38.4%). We agreed to LeeCitation19 who emphasize on the fact that metastatic nodal sterilization is the main factor determining process of down-staging.
In this study, post-operative histo-pathological assessment revealed that seven patients out of 17 (41.1%) showed positive overall nodal involvement and also two patients reported as negative MRI showing positive affection. Post-operative histo-pathological assessment also revealed that four patients out of seven (57.1%) showed positive extra-mesocolic nodal involvement, all reported in MRI. Statistical analysis of this study after correlation to post-operative histo-pathological evaluation regarding the nodal involvement revealed that MRI had 77.8% sensitivity and 75% specificity while positive predictive value accounts for 41.2% and negative predictive value accounts for 93.9%. According to LahayeCitation20, discrepancy between MRI and histo-pathological results regarding the positively MRI reported nodes could be either due to any of the following scenarios. First, False interpretation of a small vascular structure or fibrotic area as a lymph node. Second, the real nodes reported in MRI are not depicted at histo-pathological assessment. Third, real nodes are found during histo-pathological assessment but showing equivocal characteristics.
Regarding the CRM status following neo-adjuvant therapy in this study; 23 patients out of pre-management positive 28 patients (82%) showed negative post-management CRM status and only five patients showed persistent positivity (among those we found three patients to have local recurrence and distant omento-peritoneal tumour spread in further post-operative follow up CT studies). In this study, post-operative histo-pathological assessment revealed that two patients showed positive resection margin. Again we confirmed statement of LEECitation19 who reported that we face much better outcome in those patients who showed negative conversion of initially positive CRM following neo-adjuvant therapy, while those who showed persistently positive CRM face worse outcome with higher rate of recurrence, morbidity and mortality.
Regarding the EMVI following neo-adjuvant therapy in this study; 11 patients out of 15 (73.3%) showed total resolution and only four patients showed persistent affection. Post-operative histo-pathological assessment revealed that four patients showed EMVI; one of them was negative in MRI. Regarding the EMVI involvement, statistical analysis revealed that MRI had 75% sensitivity and 97.8% specificity while positive predictive value accounts also for 75% and negative predictive value accounts for 97.8%. According to PatelCitation13, good response to CRT will be manifested by disappearance of EMVI or replacement by low signal intensity fibrotic streaks within mesorectal fat.
Regarding the invasion of the surrounding viscera following neo-adjuvant therapy in this study; one patients out of four showed total resolution and three patients showed persistent affection in MRI. Post-operative histo-pathological assessment revealed that two patients showed only positive invasion of the surrounding viscera, both reported in MRI. Hence statistical analysis revealed that MRI regarding invasion of surrounding viscera had 100% sensitivity and 97.9% specificity while positive predictive value accounts for 67.7% and negative predictive value accounts for 100%. According to DresenCitation21, Pre-operative MRI evaluation of tumour invasion of the surrounding pelvic visceral structures showed 53–100% positive and 93–100% negative predictive values, hence pre-operative MRI evaluation is considered accurate imaging tool for prediction of absence of invasion of the surrounding pelvic visceral structures.
From our study we concluded that for accurate and systematic evaluation of a case of rectal cancer (pre or post CRT assessment), should fulfil the following items: ().
Table 9 Suggested detailed MRI approach of evaluation of cancer rectum.
6 Conclusion
MRI is irreplaceable for initial staging of cancer rectum and evaluation after neoadjuvant therapy to detect tumour response grade which greatly affect the choice of the operation plan and decrease local recurrence thus improving surgical results and survival rate.
Conflict of interest
The authors have no conflict of interest to declare.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 9 August 2018
References
- R.G.H.Beets-tanG.L.BeetsRectal cancer review with emphasis on MR ImagingRadiology2322004335346
- S.NougaretH.A.VargasY.LackmanIntravoxel incoherent motion derived histogram metrics for assessment of response after combined chemotherapy and radiation therapy in rectal cancerRadiology2802016446454
- H.K.ChunD.ChoiM.J.KimJ.LeeS.H.YunPreoperative staging of rectal Cancer: comparison of 3-T High-Field MRI and endorectal sonographyAJR187200615571562
- S.H.ParkJ.S.LimJ.LeeH.Y.KimW.S.KoomRectal mucinous adenocarcinoma: MR imaging assessment of response to concurrent chemotherapy and radiation therapy, a hypothesis generating studyRadiology28512017124133
- I.M.BlazicG.B.LilicM.B.GajicQuantitative assessment of rectal cancer response to neoadjuvant combined CRTRadiology0002016111
- F.G.M.TaylorRobert I.SwiftL.BlomqvistG.BrownA systematic approach to the interpretation of preoperative staging MRI for rectal cancerAJR191200818271835
- P.RouanetB.Saint-AubertC.LemanskiRestorative and nonrestorative surgery for low rectal cancer after high-dose radiation: long-term oncologic and functional resultsDis Colon Rectum4532002305313
- N.SmithG.BrownPreoperative staging of rectal cancerActa Oncol47120082031
- O.C.ShihabP.HowN.WestCan a novel MRI staging system for low rectal cancer aid surgical planning?Dis Colon Rectum5410201112601264
- S.B.EdgeD.R.ByrdC.C.ComptonAJCC Cancer Staging Handbook7th ed.2010SpringerNew York173206
- S.NougaretC.ReinholdH.W.MikhaelP.RouanetF.BibeauG.BrownThe use of MR imaging in treatment planning for patients with rectal carcinoma: have you checked the “distance”?Radiology2682013330344
- G.EnginR.SharifovMagnetic resonance imaging for diagnosis and neoadjuvant treatment evaluation in locally advanced rectal cancer: a pictorial reviewWorld J Clin Oncol832017214229
- U.B.PatelL.K.BlomqvistF.TaylorMRI after treatment of locally advanced rectal cancer: how to report tumor response; the MERCURY experienceAJR1992012W486W495
- S.D.AllenA.R.PadhaniA.S.Dzik-JuraszRectal carcinoma MRI with histopathological correlation before and after chemoradiation therapyAJR1882007442451
- MERCURY Study GroupDiagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational studyBMJ2006 doi:10.1136
- S.H.KimJ.M.LeeS.H.HongLocally advanced rectal cancer added value of diffusion weighted MR imaging in the evaluation of tumor response to neoadjuvant chemo and radiation therapyRadiology2532009116125
- Y.S.SunX.P.ZhangL.TangLocally advanced rectal carcinoma treated with preoperative chemoradiotherapy: preliminary analysis of DW MR for early detection of tumor histopathologic downstagingRadiology2542010170178
- M.M.Van HeeswijkD.M.LambregtsW.M.PalmDWI for assessment of rectal cancer nodes after chemoradiotherapy: Is the absence of nodes at DWI a proof of a negative nodal statusAJR2082017W1W6
- N.K.LeeC.Y.KimY.J.ParkClinical implication of negative conversion of predicted circumferential resection margin status after preoperative chemoradiotherapy for locally advanced rectal cancerEJR832014245249
- M.J.LahayeG.L.BeetsS.M.E.EngelenLocally advanced rectal cancer MR imaging for restaging after neoadjuvant radiation therapy with concomitant chemotherapy. Part II: what are the criteria to predict involved lymph nodes?Radiology25220098191
- R.C.DresenM.KustersA.W.Daniels-GooszenAbsence of tumor invasion into pelvic structures in locally recurrent rectal cancer prediction with preoperative MR imagingRadiology2562010143150