?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
The aim of this systematic review was to evaluate the assessment of trabecular bone patterns in dental radiographs, for fracture risk prediction, compared with the current diagnostic methods.
Methods
The PRISMA guidelines were followed. According to predefined inclusion criteria (PICO), literature searches were focussed on published studies with analyses of trabecular bone patterns on intraoral and/or in panoramic radiographs, compared with Dual X-ray Absorptiometry (DXA) and/or Fracture Risk Assessment Tool (FRAX), with the outcomes; fracture and/or sensitivity and specificity for osteoporosis prediction. The included studies were quality-assessed using the QUADAS-2 tool and the certainties of evidence was assessed using the GRADE approach.
Results
The literature searches identified 2913 articles, whereas three were found to meet the inclusion criteria. Two longitudinal cohort studies evaluated the use of trabecular bone patterns to predict bone fractures. In one of the studies, the relative risk of fracture was significantly higher for women with sparse bone pattern, identified by visual assessment of dental radiographs, and in the other study by digital software assessment. Visual assessment in the second study did not show significant results. The cross-sectional study of digital analyses of trabecular bone patterns in relation to osteoporosis reported a sensitivity of 0.70 and a specificity of 0.69.
Conclusion
Based on low certainty of evidence, trabecular bone evaluation on dental radiographs may predict fractures in adults without a prior diagnosis of osteoporosis, and based on very low certainty of evidence, it is uncertain whether digital image analyses of trabecular bone can predict osteoporosis.
Background
Osteoporosis is an asymptomatic systemic skeletal disease characterized by low bone mineral density (BMD) and micro-architectural deterioration of bone tissue. Consequently, osteoporotic patients have an increased susceptibility to fractures by low-energy mechanical forces, such as falls from a standing height [Citation1]. The risk of fracture affects especially the proximal femur (hip), vertebrae (spine), humerus (upper arm) and distal forearm (wrist) [Citation2]. As it is asymptomatic, osteoporosis causes no pain in itself and does not become evident until a fracture occurs. More than 75 million people in the United States, Europe and Japan were affected by osteoporosis in 2010, 27.6 million of whom in the EU. Osteoporosis causes more than 8.9 million fractures annually worldwide and over one third of all osteoporotic fractures occur in Europe at an annual cost of 37 billion euros [Citation3].
Fragility fractures are shown to be risk factors for increased mortality [Citation4], and a marker for comorbid conditions in the elderly population. Following a hip fracture, the relative risk of dying in the next 4 years was almost nine times greater, and almost six times greater following a spine fracture [Citation4], mainly explained by comorbidity, specifically thrombosis, due to inactivity after a fracture event. Hip fractures entail the highest morbidity and mortality, contribute to the highest direct costs for the health service and cause disability, pain and reduced quality of life [Citation5]. Age increases the fracture incidence exponentially [Citation2] and with an ageing population, the incidence of osteoporotic fractures will probably increase.
The most widely validated technique for BMD assessments used today is dual-energy x-ray absorptiometry (DXA). Bone density levels more than 2.5 standard deviations below the young adult reference mean fulfil the criteria for defining osteoporosis. For osteopenia, the levels should be between −1 and −2.5 SD [Citation6,Citation7]. Although only BMD tests have been shown to have high specificity in the detection of individuals at high risk of fracture, the test has low sensitivity [Citation8]. The fracture risk is higher in osteoporotic subjects, but the majority of fractures will occur in osteopenic subjects and individuals with normal BMD, since the majority in the general population are not osteoporotic. Thus, general screening with BMD assessments using DXA will not improve the fracture burden in society.
A web-based questionnaire for Fracture Risk Assessment (FRAX), based on data generated from The World Health Organization (WHO) Collaborating Centre for Metabolic Bone Diseases, was developed by The University of Sheffield in 2008. The FRAX tool is used together with BMD measurements to predict the probability of a fracture. It estimates the 10-year fracture risk and is used internationally. The Swedish National Board of Health and Welfare recommends thresholds for the FRAX-determined fracture risk of > 15% for medical and DXA examinations, and a FRAX-determined fracture risk of > 30% for medication with bone-active drugs. The recommended intervention thresholds are country-specific due to local differences but the majority of countries globally have a threshold around FRAX 20% [Citation9]. The following clinical risk factors are included in the FRAX model: age, gender, body mass index (BMI), previous fracture, parent fractured hip (heredity), current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, and alcohol intake [Citation10].
Osteoporosis is currently underdiagnosed and undertreated. In a population-based study of older Swedish women, only 22% of women eligible for treatment according to national guidelines were treated with osteoporosis medication [Citation11]. Dental radiographs are commonly included in dental examinations for a large proportion of the adult population and have been suggested as a method to identify individuals with high fracture risk [Citation12,Citation13]. Both digital software, such as Jaw-X [Citation14–16] and Bone Texture [Citation14,Citation15,Citation17], as well as visual assessments [Citation17–20] of trabecular bone patterns have been evaluated.
In the present systematic review, intraoral and panoramic radiographs were evaluated. On the intraoral radiograph, a relatively limited area is imaged, typically showing two to three teeth and the adjacent jawbone, but with high resolution, whereas the panoramic radiograph covers a bigger area for an overview, including both the jaws and surrounding tissues. On the other hand, it has reduced resolution and is less detailed than the intraoral image.
Improved detection of increased fracture risk is important to reduce the risk due to skeletal fragility, thereby also reducing the accompanying burden on society. In the past decades, efforts have been made by different healthcare providers to find new diagnostic and prognostic tools to identify individuals with high fracture risk. Although there are some established recommendations for fracture prevention, there is no established consensus on an effective screening method for populations in order to identify individuals with a high fracture risk.
The aim of this systematic review was to evaluate the assessment of trabecular bone patterns on intraoral and panoramic radiographs, with regard to fracture risk prediction, compared with DXA and/or FRAX.
Materials and methods
The predefined objective of this systematic review was, ‘Can analysis of trabecular bone patterns on an intraoral radiograph and/or panoramic radiograph predict the fracture risk in adults without diagnosed osteoporosis, compared with DXA or FRAX?’.
The Population, Interventions, Controls, Outcome (PICO) methodology was used to create a protocol and define the review objective:
Population: Adults without diagnosed osteoporosis.
Intervention: Analysis of trabecular bone pattern on an intraoral radiograph and/or on panoramic radiograph.
Controls: Current diagnostic methods DXA and/or FRAX.
Outcomes: Fracture, test sensitivity and specificity.
After the protocol was adopted (April, 2018), the predefined question at issue and the PICO strategy were not changed. The studies had to concur with the protocol to be included.
Selection and inclusion criteria
The inclusion criteria were limited to systematic reviews, randomized controlled trials (RCTs), cohort studies, case series (≥500 patients) and cross-sectional studies published after January 1, 1990, and written in English, Swedish, Danish, Norwegian or Finnish.
Literature searches
Systematic literature searches were performed electronically (April 2018) in Medline, Embase, the Cochrane Library and a number of national health technology assessment (HTA) databases, as well as the Clinical Trials database (www.clinicaltrials.gov) (September 2018). Reference lists of relevant articles were also scrutinized for additional references. Searches were conducted by two authors (IS, AL), who are also librarians at the HTA centre of Region Västra Götaland at the Sahgrenska University Hospital, Gothenburg, Sweden and are specially trained in search strategies for health technology assessments and systematic reviews. After performing the literature searches, they selected studies and, independently of each other assessed the obtained abstracts and made a first selection of articles for inclusion or exclusion. The resulting selection was sent to all review authors, who read the articles independently of each other and decided in a consensus meeting which articles to include. The searches were updated using the same criteria in March 2020.
Rating of quality of individual studies
The included studies were critically assessed individually according to their scientific quality using the QUADAS-2 tool for quality assessment of diagnostic accuracy studies [Citation21], which was deemed to be the most suitable tool for the cohort studies.
QUADAS enables transparent rating of the bias risk, applicability and reporting quality of the diagnostic studies included in the review. The evaluation comprised four different phases of a QUADAS-based assessment: (1) summarizing of the review question, (2) tailoring of the tool and development of review-specific guidance, (3) production of a flow diagram for the primary study, and (4) assessment of bias and applicability. The last phase (4) consisted of four key domains concerning (a) patient selection, (b) index test, (c) reference standard, and (d) flow and timing, and was rated as high, moderate or low. Thereafter, individual phase and domain assessments were performed by each author, followed by a consensus meeting including all review participants, in which an overall quality rating was determined.
Rating of evidence across studies
The quality and certainty of evidence across studies was assessed using the GRADE system [Citation22,Citation23], applicable to diagnostic tests and strategies. Each study and the evidence for each outcome variable included in this review, were assessed collectively by all the participants. Disagreements were resolved by consensus. The GRADE ratings were based on the following key elements: study design, study quality, consistency and directness. A last assessment was then agreed upon, to determine the overall certainty of evidence across all included studies. The certainty of evidence was categorized in four levels: High certainty ⊕⊕⊕⊕ (further research is unlikely to have an important impact on the confidence in the estimate of effect), Moderate ⊕⊕⊕○ (further research is likely to have an important impact), Low ⊕⊕○○ (further research is very likely to have an important impact), or Very low ⊕○○○ (any estimate of effect is very uncertain).
Results
Search results
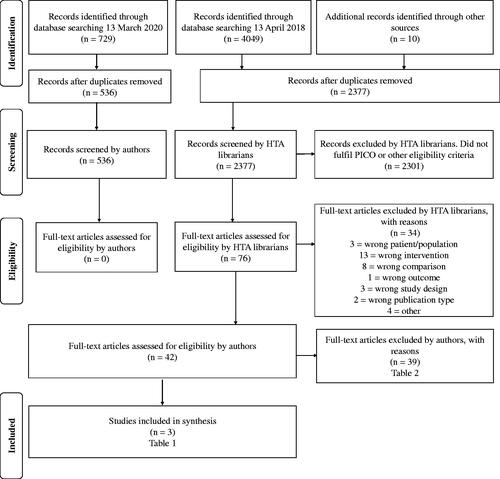
The literature searches identified a total of 2913 articles after removal of duplicates. After excluding studies that did not fulfil the inclusion criteria, three articles, two referring to cohort studies [Citation12,Citation14] and one to a cross-sectional study [Citation24], were finally included in the review. A graphic flow chart of the selection process and search results is presented in . presents the included studies, their design and patient characteristics. In , the excluded studies with the main reasons for exclusion are listed and numbered with superscript.
Table 1. Included articles – characteristics of included studies.
Table 2. Excluded articles and main reason for exclusion.
Of the 39 full-text articles read and excluded by the authors, six were excluded immediately as their focus was different from ours: three articles concerned periodontal issues,2,8,25 two dealt with methodological issues,3,5 and one concerned radiolucent periapical lesions.24
The P in PICO was ‘adults without diagnosed osteoporosis’; therefore, studies including participants with a diagnosis of osteoporosis18,19,23,28,32,34,35,39 were excluded.
The intervention chosen, the I, was analysis of trabecular patterns, and therefore all studies concerning cortical thickness,15,27,32,37 the degree of cortical erosion as well as bone density1,4,6,17,29,31,33 were excluded. Twenty-four articles focussed on trabecular bone, 15 used periapical radiographs and nine used panoramic radiographs or both. In addition to the two included articles, visual assessment of trabecular bone was used in eight articles, one of which was excluded because osteoporotic individuals were included,23 and five articles were excluded because they emanated from the same material as Jonasson and Billhult (2013)7,9–11 and Sundh et al. (2017).12 Studies using morphological features14,20–22,30,36 and classifiers16,26 were also excluded, as they are still not applicable in the clinic.
Main findings
In and , the findings of each study have been summarized and are presented per outcome. A summary result per outcome and the associated certainty of evidence are presented in a Summary-of-findings table ().
Table 3. Outcome variable – fracture prediction.
Table 4. Outcome variable – sensitivity and specificity for osteoporosis measured with DXA.
Table 5. Summary of findings.
Fracture prediction
Fracture was reported as an outcome in both cohort studies [Citation12,Citation14]. The studies had low precision due to small to moderate sample sizes and few fracture events. The two studies, which differed with regard to their settings, evaluated the use of trabecular bone pattern on intraoral or panoramic radiographs for prediction of bone fractures in women.
In Jonasson and Billhult (2013), the result of the visual assessment of the trabecular bone was a significant predictor of the total fracture risk, i.e. previous and future fractures, RR= 2.22 (95% CI: 1.06–4.61), but not of future fractures alone, RR = 1.52 (95% CI: 0.56–4.11). When sparse trabecular bone patterns were identified by digital software assessments, the relative risk using Bone Texture, was significant for both total fractures, RR = 3.16 (95% CI: 1.27–7.86), and future fractures, RR= 4.74 (95% CI: 1.49–15.04), however with Jaw-X only, the relative risk was a significant predictor of total fractures, RR = 2.18 (1.01–4.72), but not of future fractures, RR = 1.87 (0.73–4.71). Bone mineral density assessed with DXA of the forearm also showed a significant relative risk of total fractures, RR = 2.83 (95% CI: 1.39–5.78), but not for future fractures, RR = 2.37 (95% CI: 0.93–6.02). In our GRADE rating, due to PICO, only future fracture risk was considered. The description of the study population in Jonasson and Billhult (2013) was considered unclear regarding selection and exclusion of study participants.
In the study by Sundh et al. (2017) including three age cohorts examined in 1980 and 1992, the absolute fracture incidence rates were 14.2% in 1980 and 16.3% 12 years later in 1992. Women with a sparse trabecular bone pattern, identified by a dentist through visual assessment of dental radiographs, showed a significantly higher relative risk of future fracture than those with alternating dense and sparse trabeculation and those with dense trabeculation.
In 1980, the relative fracture risk for 499 women, using sparse trabeculation as a predictor of the 10-year fracture risk, was 2.09 (95% CI: 1.3–3.5). For fracture prediction with FRAX alone (threshold > 15%), the corresponding RR was 1.85 (95% CI: 0.7–5.6).
Twelve years later, in 1992, 412 of the initial 499 women were examined again. Now, in this aged group, the risk of fracture in the next 10 years using sparse trabeculation and FRAX as fracture predictors was RR = 3.7 (95% CI: 2.2–6.4) and RR = 4.1 (95% CI: 2.4–7.2), respectively. When the Fracture Assessment tool (FRAX) was combined with the visual assessment, the relative risk increased considerably in both periods. However, given the PICO, the results for combinations of FRAX and sparse trabeculation were not considered in the GRADE ratings. The certainty of the evidence according to GRADE was low (GRADE ⊕⊕○○).
Specificity and sensitivity
One cross-sectional study by Verheij et al. (2009), using radiographs from 607 women, evaluated whether morphological, digital image analysis of trabecular bone correlated to osteoporosis. Osteoporosis, defined as a BMD T-score ≤ −2.5, was assessed by DXA scanning of the lumbar spine and hip. For digital image analysis of the mandibular trabecular bone pattern as an indicator of osteoporosis, the study reported a sensitivity of 0.70 (95% CI: 0.62–0.78) and a specificity of 0.69 (95% CI: 0.64–0.73), which corresponded to the prediction using age only. Twenty-six radiographic variables of four regions of interest were used, two on the panoramic radiograph and one on each intraoral radiograph. Combining age with the trabecular pattern increased the sensitivity from 0.70 to 0.75 (95% CI: 0.67–0.82) and the specificity from 0.69 to 0.78 (95% CI: 0.75–0.82), the latter increase being statistically significant. However, age as a contributing factor was not part of the objective of this review and GRADE rating. The certainty of the evidence was very low (GRADE ⊕○○○).
Discussion
Based on the low certainty of evidence, the main finding in the review was that trabecular bone evaluation on dental radiographs may predict fractures in women without a prior diagnosis of osteoporosis. Moreover, it was found to be very uncertain that digital image analysis of trabecular bone could predict osteoporosis (DXA BMD T-score ≤ −2.5).
Except for the outcome itself, there is no gold standard established for predicting an actual fracture event. However, DXA measurement of hip bone mineral density and FRAX alone or combined are well investigated methods that are frequently used in the primary care for prevention and therefore chosen as the reference standard for predicting fracture risk.
The strength of this literature review is that it used and adhered to a strict methodology applying the PICO format, QUADAS-2 [Citation21] and the GRADE system [Citation23], for a systematic evaluation of the literature with regard to its content and scientific quality. Another strength is the evaluated outcome; fracture event, and not osteoporosis diagnosis, since most fractures occur in patients with BMD (T-score) ≤ −2.5.
A limitation may be that in one study [Citation14], the questionnaires did not include all parameters used to calculate FRAX, i.e. amount of alcohol consumption. Furthermore, the study populations in all included articles consisted of elderly female subjects. Consequently, they are not representative for the general population, thereby limiting the generalizability of results. Thus, there is a need for research that also includes men, as well as a wider range of older ages since people today tend to live longer. Moreover, this systematic review had to be based on only three scientific publications of which only two reported the same outcome; thus, no meta-analysis could be performed.
In a recent systematic review [Citation25], the potential use of dental imaging of trabecular bone structure for systemic disorder screening was evaluated. Regarding osteoporosis, they found 14 eligible articles. They included articles with osteoporotic groups and excluded studies in which trabecular bone patterns were evaluated by visual assessment, due to the subjectivity of this methodology. However, inclusion of known osteoporotic patients, i.e. the population with highest fracture risk, could potentially lead to a false positive result of the evaluated assessment of the trabecular bone pattern, and thereby limit the generalizability of the results.
In a previous study [Citation26], cortical parameters have been used and it was concluded that dentists have enough radiological information to be able to screen patients for osteoporosis. This conclusion is based on the assumption that panoramic radiographs are taken in routine examinations. Normally, in Sweden, general dental practices may not have the equipment needed for panoramic radiographs, nor is it allowed to use the technique as a routine examination according to the Swedish Radiation Safety Authority. Sundh et al. (2017) recommended periapical radiographs for evaluating the trabecular pattern due to higher resolution than in panoramic radiographs, and as assessments based on panoramic radiographs require more training [Citation27]. Moreover, analysis of cortical bone can only be assessed on panoramic radiographs and this technique was thus omitted, due to the definition of the technology at issue.
In Sundh et al. (2017), it was found that a combination of assessment of the sparse trabecular bone pattern in the mandible together with other readily available information on risk factors can improve the fracture predictive value, especially with increased age. Furthermore, the same study showed that having no risk factor was associated with a very low fracture risk (1.5%), while a combination of various risk factors increased the relative risk (by 16–23 times). However, these increased risk levels are a consequence of very few fracture events in the group without risk factors and should be observed in that context. Many other studies have reported that including age significantly improved osteoporosis and fracture prediction [Citation24,Citation28–30].
The cross-sectional study by Verheij et al. (2009) used a hypothesis-generating design, to evaluate the potentially best sensitivity and specificity for an osteoporosis diagnosis. Thus, this design entails a risk of results being significant by chance. Even if the sensitivity and specificity are high, the method should be tested in other populations in order to be validated. Also, the study of Lee and White (2005) had a hypothesis-generating design. It was a cross-sectional study with osteoporosis as the outcome. Age and trabecular pattern were correlated to the DXA of the hip and spine, and for the combination, the sensitivity was 0.86 and the specificity 0.86.
Lindh et al. (2008) evaluated visual assessments of trabecular patterns on intraoral radiographs in the premolar region as a potential method to identify women at risk of osteoporosis. For sparse trabeculation as a predictor of osteoporosis, the sensitivity was found to be low (28.2%), whereas the specificity was high (90.8%). The reported results were comparable to the observations reported in the included cohort study by Jonasson and Billhult (2013) (sensitivity 27%, specificity 88%) but, here, sparse trabeculation was used as the fracture predictor. If, in the future, dentists are to play a role in identifying patients at risk of fracture, it is important that the specificity is high to avoid an unnecessary workload in the medical clinics that handle possible referrals.
A combination of a FRAX score >15% and sparse trabeculation in mandibular bone may predict major fractures. FRAX is easily assessed and with training, visual trabecular pattern on intraoral radiographs could be assessed in dental clinics. Firstly, they all have devices to perform intraoral radiography and, secondly, dentists are well trained in interpreting dental radiographs as well as working with prevention.
Using intraoral radiographs as fracture risk detectors can also be appropriate because of the trabecular bone remodelling rate. According to Kanis et al. (1994), the remodelling rate of trabecular bone is much higher than that of cortical bone, and the mandibular alveolar bone remodelling rate is higher than that of trabecular bone in other parts of the skeleton [Citation31].
The literature revealed a rich variation of advanced methods to assess osteoporosis and fracture risk without the use of DXA or in combination with DXA. Most methods have not yet been sufficiently developed for use in the clinic, but it is obvious that a reliable, fully objective, cheap and simple method is desirable. However, this is difficult since the trabecular structure varies in different regions and one may speculate that it changes with loadings from mastication and paranormal function like bruxism. There is undeniable an element of subjectivity when the trabecular pattern is evaluated. It is not an unusual situation for dentists who daily use subjective assessments of caries and bone pathology. Lindh et al 2008 found that intraobserver agreement of 5 observers’ assessments was moderate or good but with a wide range between the highest and lowest. Probably, sparse trabecular pattern could be used complementary together with either FRAX or sustained previous fracture. Research groups are developing various texture analysis methods to measure trabecular spacing, connectivity and trabecular volume, using computed tomography, magnetic resonance, and cone beam-computed tomography, but the cost and complexity of these methods limit their usefulness in the clinic and as screening methods.
Besides the large number of false positive and negative test results that can be expected, trabecular bone pattern assessments on dental radiographs to estimate the fracture risk, applied as a technology in general dentistry, may be time-consuming, may lead to increased referrals to primary care and possibly DXA measurement and may cause referred patients a feeling of uncertainty and worry [Citation32]. These consequences, together with the health economic aspects of the technology, must be evaluated together with its potential benefits, considering the prevalence of the osteoporotic fracture risk and the specificity and sensitivity of the predictive tests.
Conclusion
In conclusion, based on low certainty of evidence (GRADE ⊕⊕○○), trabecular bone evaluation on dental radiographs may predict fractures in adults without a prior diagnosis of osteoporosis, and based on very low certainty of evidence (GRADE ⊕○○○), it is uncertain whether digital image analyses of trabecular bone can predict osteoporosis. Larger prospective and long-term studies in varying settings with fracture as the outcome are warranted, in order to better understand the potential role of trabecular pattern assessments on radiographs for identifying those with high risk of future fracture.
Author contributions
AJ, GJ, MH, contributed to conception, design, data acquisition, analysis and interpretation, drafted and critically revised the manuscript; HL, SB, JH, HD, AL, CP, IS, CW, PS, contributed to conception, design, data acquisition, analysis, interpretation and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgements
The Public Dental Service in Region Västra Götaland supported the study. The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article. The co-authors were not involved in the evaluation of their respective articles.
This publication is based on an HTA-report published as Johanen A, Bernhardsson S, Hagman J, Hakeberg M, Hange D, Jonasson G, Laine C, Liljegren A, Lund H, Persson C, Svensson M, Stadig I, Svensson M, Wartenberg C, Sjögren P. Trabecular bone pattern assessment in dental radiographs for prediction of fracture risk [Utvärdering av trabekulärt benmönster i tandröntgenbilder för prediktion av frakturrisk].Göteborg: Västra Götalandsregionen, Sahlgrenska Universitetssjukhuset, HTA-centrum, Sweden; 2019. Regional activity based HTA 2019:104.
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
All data generated and analysed in this review are included within the article.
References
- Kanis JA, Oden A, Johnell O, et al. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int. 2001;12:417–427.
- World Health Organization. WHO Scientific Group on the assessment of osteoporosis at primary health care level. 2004. Available from: https://www.who.int/chp/topics/Osteoporosis.pdf
- Hernlund E, Svedbom A, Ivergård M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136.
- Cauley JA, Thompson DE, Ensrud KC, et al. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561.
- Borgström F. [Osteoporosis in health economic perspective]. Lakartidningen. 2006;103:2963–2965.
- Kanis JA, Melton LJ 3rd, Christiansen C, et al. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–1141.
- Kanis JA, McCloskey EV, Johansson H, et al. A reference standard for the description of osteoporosis. Bone. 2008;42:467–475.
- World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Technical report series. No 843. Geneva (Switzerland): WHO; 1994.
- Kanis JA, Harvey NC, Cooper C, et al., Advisory Board of the National Osteoporosis Guideline Group. A systematic review of intervention thresholds based on FRAX : A report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos. 2016;11:25.
- Kanis JA, Johnell O, Oden A, et al. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397.
- Lorentzon M, Nilsson AG, Johansson H, et al. Extensive undertreatment of osteoporosis in older Swedish women. Osteoporos Int. 2019;30:1297–1305.
- Sundh V, Hange D, Ahlqwist M, et al. FRAX and mandibular sparse trabeculation as fracture predictors: a longitudinal study from 1980 to 2002. Eur J Oral Sci. 2017;125:135–140.
- Jonasson G, Sundh V, Ahlqwist M, et al. A prospective study of mandibular trabecular bone to predict fracture incidence in women: a low-cost screening tool in the dental clinic. Bone. 2011;49:873–879. Oct
- Jonasson G, Billhult A. Mandibular bone structure, bone mineral density, and clinical variables as fracture predictors: a 15-year follow-up of female patients in a dental clinic. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:362–368.
- Hassani-Nejad A, Ahlqwist M, Hakeberg M, et al. Mandibular trabecular bone as fracture indicator in 80-year-old men and women. Eur J Oral Sci. 2013;121:525–531.
- Jonasson G, Lindberg F, Jorge A, et al. Mandibular trabecular bone structure in adults with Crohn’s disease. Clin Oral Investig. 2014;18:423–428.
- Jonasson G, Jonasson L, Kiliaridis S. Changes in the radiographic characteristics of the mandibular alveolar process in dentate women with varying bone mineral density: a 5-year prospective study. Bone. 2006;38:714–721.
- Lindh C, Petersson A, Rohlin M. Assessment of the trabecular pattern before endosseous implant treatment: diagnostic outcome of periapical radiography in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:335–343.
- Lindh C, Horner K, Jonasson G, et al. The use of visual assessment of dental radiographs for identifying women at risk of having osteoporosis: the OSTEODENT project. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:285–293.
- Jonasson G, Bankvall G, Kiliaridis S. Estimation of skeletal bone mineral density by means of the trabecular pattern of the alveolar bone, its interdental thickness, and the bone mass of the mandible. Oral Surgery Oral Med Oral Pathol Oral Radiol Endodontol. 2001;92:346–352.
- Whiting PF, Rutjes AWS, Westwood ME, et al., QUADAS-2 Group. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann Intern Med. 2011;155:529–536.
- Atkins D, Best D, Briss PA, et al., GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
- Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406.
- Verheij JG, Geraets WG, van der Stelt PF, et al. Prediction of osteoporosis with dental radiographs and age. Dentomaxillofac Radiol. 2009;38:431–437.
- Pachêco-Pereira C, Almeida FT, Chavda S, et al. Dental imaging of trabecular bone structure for systemic disorder screening: a systematic review. Oral Dis. 2019;25:1009–1026.
- Vlasiadis KZ, Skouteris CA, Velegrakis GA, et al. Mandibular radiomorphometric measurements as indicators of possible osteoporosis in postmenopausal women. Maturitas. 2007;58:226–235.
- Pham D, Jonasson G, Kiliaridis S. Assessment of trabecular pattern on periapical and panoramic radiographs: a pilot study. Acta Odontol Scand. 2010;68:91–97.
- Lee BD, White SC. Age and trabecular features of alveolar bone associated with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:92–98.
- White SC, Atchison KA, Gornbein JA, et al. Change in mandibular trabecular pattern and hip fracture rate in elderly women. Dentomaxillofac Radiol. 2005;34:168–174.
- Licks R, Licks V, Ourique F, et al. Development of a prediction tool for low bone mass based on clinical data and periapical radiography. Dentomaxillofac Radiol. 2010;39:224–230.
- Huja SS, Fernandez SA, Hill KJ, et al. Remodeling dynamics in the alveolar process in skeletally mature dogs. Anat Rec. 2006;288A:1243–1249.
- Hvas L, Reventlow S, Jensen HL, et al. Awareness of risk of osteoporosis may cause uncertainty and worry in menopausal women. Scand J Public Health. 2005;33:203–207.