Abstract
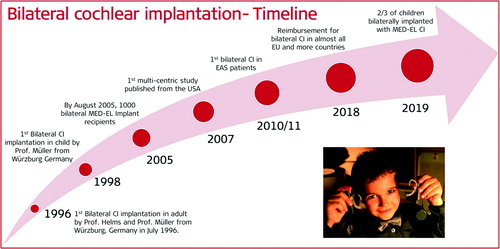
Binaural hearing has certain benefits while listening in noisy environments. It provides the listeners with access to time, level and spectral differences between sound signals, perceived by the two ears. However, single sided deaf (SSD) or unilateral cochlear implant (CI) users cannot experience these binaural benefits due to the acoustic input coming from a single ear. The translational research on bilateral CIs started in the year 1998, initiated by J. Müller and J. Helms from Würzburg, Germany in association with MED-EL. Since then, several clinical studies were conducted by different research groups from across the world either independently or in collaboration with MED-EL. As a result, the bilateral CI has become the standard of care in many countries along with reimbursement by the health care systems. Recent data shows that children particularly, are given high priority for the bilateral CI implantation, most often performed simultaneously in a single surgery, as the binaural hearing has a positive effect on their language development. This article covers the milestones of translational research from the first concept to the widespread clinical use of bilateral CI.
Graphical Abstract
Chinese abstract
双耳收听在嘈杂的环境中具有一定的听力好处。它为听者提供两只耳朵可以感知到的声音信号之间的时间、水平和频谱差异。但是, 单侧聋(SSD)或单侧CI植入患者不能感受到由于来自单耳的声音输入而带来的双耳收听的好处。双侧CI的转化研究始于1998年, 由德国乌尔茨堡市的Müller教授和Helms教授与MED-EL联营发起的。此后, 来自世界各地的不同研究小组独立地或与MED-EL合作进行了几项临床研究。结果, 随着医疗保健系统提供报销, 双侧CI已成为多个国家和地区的医疗标准。最新数据显示, 尤其是儿童, 双侧CI植入被高度重视, 在一次手术中同时进行双侧植入, 因为双耳听觉对语言发展有积极影响。本章涵盖了与MED-EL合作的围绕双侧CI主题的关键性转化研究的重点。
1.1. Introduction
The ear transmits sound waves to the brain, and having an ear on each side of the head helps with localising the direction of the sound. The term binaural hearing refers to normal hearing with two ears. The hearing has two primary functions: communication (speech recognition) and warning (acoustic source localisation). The critical task for the central auditory pathways is to break down the auditory messages sent by the two ears into auditory objects. The segregation and localisation of auditory objects constitute an essential means of separating target signals from noise and competing sources. With asymmetric or single-sided deafness, or with a cochlear implant (CI) on one side, the monaural exploitation of sound messages significantly lessens the performance compared to what it should be in a binaural situation [Citation1]. Binaural hearing in normal-hearing individuals offers speech intelligibility, sound source localisation, understanding the speech in a noisy environment, and hearing with enough loudness. Technically, the benefits or effects of binaural hearing can be brought under the terms head-shadow, squelch, summation and localisation (). In brief, the head-shadow effect results from the physical placement of the head which acts as an acoustic barrier and attenuates sound (speech or noise) on one ear if that sound (speech or noise) comes from the other ear. Squelch effect corresponds to the brain’s ability to suppress background noise and attend to a specific auditory signal that comes binaurally. Summation effect, also known as loudness summation, refers to the identical loudness perception due to balanced action potentials coming from both ears to the auditory brainstem. Localisation is the ability to perceive directions of where different sounds are coming from, and it helps with the orientation [Citation2].
To sum up, most noise reduction and acoustical orientation abilities of the human auditory system rely on the listener having access to time, level and spectral differences between sound signals, perceived by the two ears [Citation3]. However, single-side deaf (SSD) patients, asymmetric hearing loss (AHL) patients, and unilaterally implanted patients with CI cannot experience these binaural benefits due to the acoustic input coming from a single ear. Additionally, the real-world listening environment in which the signal and the unwanted competing sounds may overlap spectrally and temporally, as well as spatially, makes the listening worse. While the unilateral CI treatment in bilaterally deaf children offers significant benefit in terms of speech development, still the full binaural benefits are missing to a certain degree [Citation4], and the bilateral CI is not a luxury but rather a right to experience it.
The incidence rate of bilaterally born deaf population is approximately 0.3–1 per 1,000 births [Citation5], and the bilateral CI was not a topic of research and interest until 1995. Before that, bilateral CI was not a treatment option to restore binaural hearing – instead, it was used either as a technology upgrade in combination with an older, still functioning device with no wish of replacement or due to inadequate performance with the device in the ipsilateral ear. Early research in these accidental bilateral CI implantations showed that the auditory system has the potential to process and integrate additional information provided by two different devices [Citation6].
MED-EL takes inspiration from nature by designing its technologies to mimic it, such as with the unique concept of long electrode array length to cover the entire frequency range, flexible electrode array design to preserve the intracochlear structures, frequency-specific group delays in the sound coding strategy to mimic the natural hearing and more. In that aspect, binaural hearing is also a natural phenomenon science which MED-EL made every effort to understand by sponsoring/supporting several clinical studies across the world, and before translating it to the concept of bilateral CI. Nowadays, as a result of all translational science efforts from MED-EL, bilateral CI is highly acknowledged in several countries and reimbursed for the entire treatment.
This article will review the history of how and when MED-EL started its journey of bilateral CI, summarise fundamental research studies that are either MED-EL sponsored/supported or that involved MED-EL CI device, and which demonstrated the benefits of bilateral CI. The article will also point out the critical studies that reported on the cost-utility with bilateral CI.
1.2. Beginning of MED-EL’s bilateral CI journey
In July 1996, MED-EL’s bilateral multichannel CI journey started with the first bilateral implantation in an adult to restore binaural hearing. The surgery was performed by Prof. Helms and Prof. Müller in Würzburg in Germany ().
Figure 2. ENT surgeons from Julius-Maximilian University of Würzburg, Germany, who performed the first bilateral CI implantation with MED-EL’s CI device (in 1996).

A brief history about the patient reveals that he already had a single-channel MED-EL CI device implanted in one ear and received a multichannel MED-EL CI in the second ear. The multichannel CI device in the second ear provided him with a superior hearing experience, compared to the single-channel CI in the first ear. The circumstance encouraged him to request the replacement of the latter with a multichannel CI device. The observed hearing benefits under binaural CI condition () attracted the researchers from the Research Triangle Institute (Research Triangle Park, North Carolina, USA) to perform extensive series of audiological tests – which reconfirmed the gain in speech understanding and instilled confidence in the Würzburg ENT team to extend the bilateral CI treatment to the paediatric patient population.
1.3. The German Hochmair-Schulz-Moser sentence test
In the mid-’90s, there was no practical audiological test available to evaluate speech understanding ability of CI users in noise. The German Hochmair-Schulz-Moser (HSM) sentence test was designed and developed by Dr Ingeborg Hochmair, Dr Eckard Schulz, DI Ludwig Moser and DI Markus Schmidt () with the desire to have enough test sentences for the repeated evaluation of speech understanding of CI users in noise.
Figure 3. Engineers and audiologists who designed and developed the HSM sentence test to evaluate the speech understanding of CI users in noise. 1MED-EL and 2University of Würzburg, Germany.

The name HSM derives from the surnames Hochmair, Schulz and Moser. The test consists of thirty lists of twenty everyday sentences with the level of difficulty corresponding to sentences spoken in everyday life with background noise [Citation7]. The whole test material was made available on compact disc (CD) and Comité Consultatif International Téléphonique et Télégraphique (CCITT) noise on the second channel of the CD to mimic the real-world background noise. Over time, this test became one of the gold standards in the evaluation of speech understanding of CI users in noise.
1.4. The first paediatric patient receives bilateral CI
In January 1998, the first bilaterally implanted paediatric patient (Max, a four-year-old boy from Germany) was operated on the second ear after he had received his first CI in 1996 at the age of 2 years, by the same ENT group from Würzburg. In the year 2000, Prof. Müller and his colleagues published their experience of understanding binaural benefits from their patients implanted with MED-EL CI devices (COMBI 40 or COMBI 40+) in combination with the continuous interleaved sampling (CIS) signal processing strategy [Citation8]. shows the percentage of correct word results which were higher in the bilateral CI listening condition, compared to the monaural listening condition from the very first patient implanted bilaterally with MED-EL’s COMBI 40 device in 1996. shows significantly higher sentence test scores of bilateral CI condition in comparison to the monaural CI listening condition from four patients bilaterally implanted with COMBI 40 device. These were the very first hearing performance results of bilaterally implanted CI users with MED-EL devices, and the authors concluded that all implanted patients showed significant benefits from the second implant. Better hearing monoaural implant results (grey bars) compared to the binaural condition (red bars) (A). HSM sentence test scores in noise with S/N of 5–13dB for four bilaterally implanted adults (B). Histograms created from data given in Müller et al. [Citation8].
1.5. Early evidence of binaural hearing benefits with CI
In 2002, the same ENT group studied the binaural benefits of bilateral CI in adult patients (n = 8) who were implanted before 2001 with COMBI 40 or COMBI 40+ devices that used CIS or CIS + sound coding strategy from MED-EL [Citation9]. They quantified the gain in SNR at speech reception threshold (SRT) in a symmetrical test setup that largely minimised the interaural differences in SNR by positioning four loudspeakers at 45°, 135°, 225° and 315° azimuth, to eliminate any head shadow effects ().
Figure 5. Symmetrical test setup to quantify the gain in SNR at the SRT (A). The average gain in the SNR overtime at the speech reception threshold (ΔSNR50) of eight patients under bilateral CI condition (B). Test scheme and histogram created from data given in Schön et al. [Citation9].
![Figure 5. Symmetrical test setup to quantify the gain in SNR at the SRT (A). The average gain in the SNR overtime at the speech reception threshold (ΔSNR50) of eight patients under bilateral CI condition (B). Test scheme and histogram created from data given in Schön et al. [Citation9].](/cms/asset/a63d4932-4416-46db-ada4-cfe5135a2f8f/ioto_a_1888193_f0005_c.jpg)
The CI hearing ear was evaluated based on unilateral monosyllable scores in quiet. In patients in whom the right CI ear was the better CI ear, the speech signal was presented simultaneously from 45° to 135° azimuth, and the noise signal simultaneously from 225° to 315° azimuth. If on the other hand, the left CI ear was the better CI ear, the speech and noise loudspeakers were switched. The test results showed that patients showed a gain in SNR50 when using both implants instead of the better CI ear alone, with a mean ΔSNR50 of 4 dB, translated into an average improvement in speech reception of 28% (). This remarkable bilateral benefit was achieved despite the largely absent head shadow SNR benefit, as a result of the symmetrical test setup. Therefore, the ΔSNR50 was achieved mainly due to the combination of bilateral summation and squelch effects.
In the same year, the same ENT group performed further series of audiological tests, including sentence and monosyllabic word tests in noise, to study the head shadow, squelch and summation effects that are associated with binaural hearing [Citation3].
shows the audiological test results of comparing the monaural and bilateral CI condition. It was observed that with bilateral CI, the scores from all tests were significantly higher than in the monaural CI condition. shows the results of binaural effects. For each CI ear, the unilateral head shadow benefit was determined by subtracting the sentence test score with speech presented from the front and noise to the contralateral ear from the test score with a speech from the front and noise presented to the ipsilateral ear. From all patient results, the average head shadow showed a benefit of 20.4%. For a specific direction of noise presentation, the squelch effect contribution of 10.7% across all patients was observed by subtracting the score when listening with the better SNR ear alone from the scores when listening with both CIs. The contribution due to the bilateral summation effect was calculated for monosyllabic words in quiet by subtracting the score obtained with both CIs from the score obtained with one CI. The summation benefit accounted to 18.7% across all results.
Figure 6. The first row showing audiological test results with mean, median and standard deviation at first and third quartile (A). The second row showing binaural advantage due to head shadow, squelch and the bilateral summation effects, calculated from the first-row results [Citation3] (B). Statistical analysis: Two-tailed tests were used for all comparisons. Reproduced by permission of Wolters Kluwer Health, Inc.
![Figure 6. The first row showing audiological test results with mean, median and standard deviation at first and third quartile (A). The second row showing binaural advantage due to head shadow, squelch and the bilateral summation effects, calculated from the first-row results [Citation3] (B). Statistical analysis: Two-tailed tests were used for all comparisons. Reproduced by permission of Wolters Kluwer Health, Inc.](/cms/asset/ee096871-ec53-4cc3-90ef-69a16d876130/ioto_a_1888193_f0006_c.jpg)
Further in the year 2002, a multicentre study on bilateral CI took place between the ENT department of Ruhr University Bochum in Germany, the University of Würzburg in Germany, and the University of Bern in Switzerland [Citation10] ().
Figure 7. A collaboration between CI surgeons and audiologists from Germany (1Ruhr University Bochum, 2University of Würzburg) and Switzerland (3University of Bern) who evaluated the effectiveness of bilateral CI in postlingually deaf patients.

Altogether, seventeen postlingually deaf patients were bilaterally implanted with MED-EL COMBI 40 or COMBI 40+ device which used CIS signal processing strategy. The two CIs were implanted either simultaneously as a one-stage or sequentially as a two-stage procedure. HSM sentence test at 70 dB hearing level and with a relatively low SNR, among all patients resulted in higher scores in the bilateral CI listening, in comparison with the monaural listening with their better CI ear (). This was yet another evidence which demonstrated the binaural hearing benefits with bilateral CI.
Figure 8. Scores of HSM sentence test at 70 dB hearing level and 10 dB signal-to-noise ratio (S/N). Histogram created from the data given in Stark et al. [Citation10].
![Figure 8. Scores of HSM sentence test at 70 dB hearing level and 10 dB signal-to-noise ratio (S/N). Histogram created from the data given in Stark et al. [Citation10].](/cms/asset/d58d487e-8d40-4239-869e-4a5931d6baec/ioto_a_1888193_f0008_c.jpg)
Although these early reports on binaural hearing benefits with bilateral CI in adults were encouraging [Citation3,Citation8–10], the sequentially bilaterally implanted children had some challenges with getting used to the second CI at early stages of their bilateral CI journey, before reaching their plateau performance.
In 2002, Dr Kühn-Inacker suggested that preparing children psychologically for different hearing sensation and speech understanding with the second CI is essential [Citation11] ). To avoid any early disappointments with the second CI, it was recommended to have the first CI in use in combination with the second CI. Optimisation of the second CI speech processor should be performed with great care while keeping the first CI speech processor at constant settings. Moreover, a separate auditory training with the second CI might be necessary to align auditory competencies with both systems.
1.6. Bilateral CI in Asia
In 2003, the bilateral CI implantation with MED-EL CI device (COMBI 40+ and CIS strategy) extended to Hong Kong and that demonstrated the binaural hearing benefits in discriminating Cantonese (Chinese dialect) lexical tones in the background noise and quiet test condition by four Cantonese-speaking CI users [Citation12] (.
Cantonese, with its six contrastive tones, has a characteristic that different tones of the same phonemic segments carry a different meaning. The voice-contrastive pitch patterns produced by the vocal cord convey the lexical meanings of Cantonese tones, and these tonal changes are not detectable by lip-reading. The perception of these tones requires good temporal and spectral auditory abilities.
Figure 10. Audiologist and CI surgeons from the University of Hong Kong Medical Centre, Queen Mary Hospital, Hong Kong.

Speech was presented at 65 dB SPL in relation with speech weighted noise, at SNRs of +15, +10, +5, 0, −5, −10 and −15. shows the mean percentage of correct Cantonese lexical tone discrimination scores of the four patients in both monaural and bilateral listening conditions at various SNRs and in quiet. A score of 66.77% or above, was regarded as being significantly above the chance levels, as shown by the red horizontal line in .
Figure 11. Mean percentage of correct Cantonese lexical tone discrimination scores, obtained from four bilaterally and eight unilaterally implanted CI patients at various SNRs and in quiet. * A score of ≥66.77% was regarded as being significantly above the chance level [Citation12]. Reproduced by permission of Elsevier B.V.
![Figure 11. Mean percentage of correct Cantonese lexical tone discrimination scores, obtained from four bilaterally and eight unilaterally implanted CI patients at various SNRs and in quiet. * A score of ≥66.77% was regarded as being significantly above the chance level [Citation12]. Reproduced by permission of Elsevier B.V.](/cms/asset/958ea47b-a322-43f2-bd67-bc75237dcb2b/ioto_a_1888193_f0011_c.jpg)
In the bilateral CI condition in quiet and at SNRs of +15, +10 and +5, the discrimination scores resulted above the set value of 66.77%, whereas in monaural CI condition, the discrimination scores were correct only at SNRs of +15, +10. Only +5 dB SNR (speech stimuli 5 dB louder than the background noise) was needed for the bilateral listening condition, whereas +10dB SNR was needed for the monaural listening conditions to discriminate between Cantonese lexical tones. In the same year, another Chinese report on the binaural benefits with bilateral CI showed lower hearing thresholds and better speech discrimination scores under aided conditions, in comparison to the monaural CI condition from two patients implanted with MED-EL COMBI 40+ device [Citation13].
1.7. MED-EL’s involvement in evaluating bilaterally implanted CI patients
In 2004, MED-EL evaluated the sound localisation abilities in bilateral CI users [Citation14] (). Twenty postlingually deaf patients with an average age of forty-five years participated in the study. They were implanted either with MED-EL’s COMBI 40 or COMBI 40+ device and used the CIS + strategy, and they had at least one month of bilateral CI hearing experience before being included in the study.
Figure 12. MED-EL specialists who were involved in evaluating the sound localisation abilities of bilateral MED-EL CI users in the year 2004.

Localisation testing with both unilateral and bilateral CI listening was performed in an anechoic chamber with an array of nine loudspeakers, equally distributed throughout 180° in the frontal plane (). Bursts of speech-shaped noise were used as stimuli presented at 60-, 70- or 80-dB SPL – values considered above the automatic gain control (AGC) compression onset. The responses from all twenty participants were brought under three main patterns, as shown in . For the unilateral listening conditions, the pattern I (, first row in red) resembled a pattern of guessing by the participants where responses were scattered over all presentation azimuth ф (x-axis), and the mean values for the response azimuth Џ (y-axis) are close to 0 with high standard deviation. Pattern II (, second row in blue) showed a pattern of guessing where responses were scattered over loudspeaker positions (sound source) ф, ipsilateral to the implant only and leading to a marked bias in the mean values towards the side where the implant was used. Pattern III (, third row in green) showed a relation between Џ and ф, somewhat even for the unilateral listening conditions. Authors pointed out that among these three patterns, all forms of hybrids existed.
Figure 13. Sound localisation responses in 3 different patterns. The left column shows results for left CI only; middle column for both CIs; right column for the right CI only [Citation14]. Statistical analysis: Post hoc analysis (p ≤ 0.05). Reproduced by permission of Wolters Kluwer Health, Inc.
![Figure 13. Sound localisation responses in 3 different patterns. The left column shows results for left CI only; middle column for both CIs; right column for the right CI only [Citation14]. Statistical analysis: Post hoc analysis (p ≤ 0.05). Reproduced by permission of Wolters Kluwer Health, Inc.](/cms/asset/a8c308ac-8da7-4c17-a1d9-e8ffc99a67f0/ioto_a_1888193_f0013_c.jpg)
Under bilateral listening conditions (grey shaded middle column), the sound localisation was significantly better than in the unilateral listening conditions in all three patterns of responses. The study evidenced a substantial benefit in sound localisation under bilateral CI listening conditions in late-deafened patients.
In 2004, another important report from Würzburg clinic was published, which demonstrated improved auditory skills in a group of children (n = 18) implanted bilaterally with a MED-EL CI. The time difference between the first and the second CI ranged from zero to four years. From the standard speech audiometry in quiet, the mean word discrimination scores tested with both CIs (86.4%) showed a tendency to be significantly higher than that reached with the left CI (75.1%) or the right CI alone (71.8%) (). Based on results from the speech discrimination test, the influence of time delay between both implantations, as well as the influence of age at first CI implantation, did not affect the outcome. However, it was recommended to minimise the time before restoring hearing in the second ear, as well as before beginning with the rehabilitation program.
Figure 14. Mean of monosyllabic word discrimination scores tested in quiet with both CIs, as well as with the right CI and left CI separately. Statistical analysis: Wilcoxon test and paired t-test. Histogram created from data given in Kühn-Inacker et al. [].
![Figure 14. Mean of monosyllabic word discrimination scores tested in quiet with both CIs, as well as with the right CI and left CI separately. Statistical analysis: Wilcoxon test and paired t-test. Histogram created from data given in Kühn-Inacker et al. [].](/cms/asset/256a3611-69cc-4aec-98df-48f3e6d822f3/ioto_a_1888193_f0014_c.jpg)
In 2005, as more research works began to take place in evaluating the binaural benefits of bilateral CI, the year also marked more than one thousand bilateral MED-EL CI implantations across the world. This was an encouraging milestone for the scientific efforts led by MED-EL with the support of ENT professionals globally. The ability to detect an interaural level (loudness) difference and interaural time (lateralisation) difference combined – also known as a binaural cue – is another benefit of binaural hearing. In the same year, Dr Nopp, a signal processing engineer from MED-EL, together with clinicians from the Julius Maximilian University of Würzburg, evaluated the sensitivity of both, level and time differences, of bilaterally implanted CI patients [Citation15]. For the level difference evaluation, tests were performed with each of the two audio processors’ unbalanced loudness. The loudness unbalancing was performed by decreasing the volume on one side’s audio processor while keeping the volume on the other side unchanged. The localisation bias фB in azimuth as obtained from the localisation experiment is shown as a function of the loudness difference for four different patients (). Loudness was rated on a linear scale, consisting of five categories (very soft, soft, medium, loud, and very loud) and where one corresponded to the lowest level and fifty to the highest level. The level difference was calculated by subtracting left-CI-only loudness judgements from the right-CI-only loudness judgements, obtained at the same presentation level. The findings showed an increase in the magnitude of localisation bias (фB) with increasing the loudness difference, and the linear regression amongst four patients is evidence of bilateral CI patient’s ability to sense interaural level differences.
Figure 15. (A) Localisation bias фB as a function of loudness difference between right and left CI. (B) Mean values and standard deviation error values of lateralisation L as a function of interaural time difference τ for subject A from the previous experiment shown in graph A [Citation15]. Reproduced by permission of Wolters Kluwer Health, Inc.
![Figure 15. (A) Localisation bias фB as a function of loudness difference between right and left CI. (B) Mean values and standard deviation error values of lateralisation L as a function of interaural time difference τ for subject A from the previous experiment shown in graph A [Citation15]. Reproduced by permission of Wolters Kluwer Health, Inc.](/cms/asset/1f1fd3e2-8da0-4df3-baa4-7034fa065b1e/ioto_a_1888193_f0015_b.jpg)
Lateralisation test results are shown in for the best performer with the mean values (diamond symbol) and standard error values (error bars) of lateralisation L (left ear: L = −100%; right ear: L = 100%) as a function of interaural time difference τ (τ corresponds with the pulse on the right ear leading). For the time difference testing, a pair of pulses, separated by a specific time difference, was presented to the patients through their speech processors with one pulse directed to each side. The range of time differences used in the test was always symmetrical to 0µs, with the minimum time difference (left side pulse leading) ranging from −600 µs to −1,200 µs, and the maximum time difference (right side pulse leading) ranging from 600µs to 1,200µs. Between the minimum and maximum time difference, twelve pairs of seven equally spaced time differences, including 0µs, were tested. The patients’ judgement on time difference was recorded on a linear scale with seven equally spaced units (corresponding to seven various time differences tested) with the centre of the scale referring to the centre of the head. In the range from −540µs to 540µs, the patients showed a relatively linear increase in L with τ increasing. Beyond and below this time difference range, sensitivity to L saturated. The results seen from these two experiments demonstrated that in principle, it was possible to have ILDs and ITDs in patients implanted bilaterally with CIs.
1.8. New measures of binaural benefits with bilateral CI
An alternative measure for spatial hearing is the minimum audible angle (MAA) test, with which the smallest angular separation of two sounds is perceived to come from distinct sources. MAA is an excellent measure which is consistent and reliable in discriminating left/right task and may be applied to infants as young as few months of age, as well as older patients. In normal-hearing children and infants, the MAA can reach 12° to 19° at six months of age – which decreases to between 4° to 6° by eighteen months of age – and 1° to 2° by five years of age, at which point they are not significantly different from an adult’s MAA [Citation16]. The MAA thresholds are worse in the absence of binaural cues, and this makes MAA an indicator of the emergence of binaural abilities in children who are fitted with CI. Prof. Senn and his colleagues from Switzerland showed that adult bilateral CI users express near-normal MAAs of 3°to 8° in front and back of the head, while at the sides, relatively poor MAAs of 30° to 45° (control group’s normal hearing was 7° to 10°) were found [Citation17]. The possible reason for the poor MAAs at the sides could be the audio processor’s microphone position (positioned above pinna). In other aspects, the study pointed out the deficiency of envelope-based CIS speech coding strategy in not carrying fine structure cues. The importance of fine structure information in the coded sound signal in the modern sound coding strategy of “Fine Structure Processing” is given in article 5 within this compendium, under section 5.2.3.
In 2006, Dr Litovsky and her colleagues from the US studied binaural benefits using MAA as a measure in bilateral and bimodal listening conditions in two groups of children, with one group bilaterally implanted with CI and the other group unilaterally implanted with CI, including MED-EL devices, with the contralateral ear fitted with a hearing aid (HA) [Citation16]. In the CI–CI group, MAA thresholds were lower (better) in the bilateral mode than in the monaural mode for all paediatric patients. In the CI–HA group, the results were similar, with most patients (six out of eight) showing bilateral benefit, compared to the monaural condition, but with no statistically significant differences (). The presented results suggest that the ability of bilateral CI advancement in paediatric patients does not require prior binaural experience and may not be restricted to those who are implanted immediately after the onset of deafness. However, they cautioned that the extent to which a critical period exists during development for these abilities remains to be determined. Important recommendations, such as electrode channels distribution along the tonotopic axis of the cochlea equally in both ears, along with the speech processing strategy carrying fine structure information to specific channels along the two CI arrays matching spectrally and temporally, were made. A brand comparison results on the MAA is further given in section 1.10.
Figure 16. Group average MAA values for two groups of paediatric patients, both in bilateral and monaural CI listening condition. CI–CI = bilateral CI; CI–HA = CI on one ear and a hearing aid on the contralateral ear. Statistical analysis: Paired-sample t-tests (p < .05). Histogram created from data given in Litovsky et al. [Citation16].
![Figure 16. Group average MAA values for two groups of paediatric patients, both in bilateral and monaural CI listening condition. CI–CI = bilateral CI; CI–HA = CI on one ear and a hearing aid on the contralateral ear. Statistical analysis: Paired-sample t-tests (p < .05). Histogram created from data given in Litovsky et al. [Citation16].](/cms/asset/f8501d39-7e11-4f88-ba75-5c0ef7f717fa/ioto_a_1888193_f0016_c.jpg)
1.9. More evidence on binaural benefits with MED-EL’s bilateral CI
In 2006, Prof. Ricketts and his colleagues from the Department of Hearing and Speech Sciences at Vanderbilt School of Medicine in the US, along with the support of MED-EL through a research grant, investigated the comparison of speech recognition in noise between bilateral and unilateral CI modes among postlingually deaf adult bilateral CI recipients [Citation18]. Sixteen bilaterally implanted C40+ patients (TEMPO + audio processor with CIS + processing strategy) were recruited for this study. Both, the hearing in noise test (HINT) and speech recognition test at fixed SNRs were performed in a soundproof room with the patient sitting in the centre. Five uncorrelated, competing noise samples were played through loudspeakers placed at the 30°, 105°, 180°, 255°, and 330° azimuth relative to the position of the head. The test stimuli were presented from a loudspeaker placed directly in front of the participant (0° azimuth; ).
Figure 17. Audiological test setup (A). HINT test hearing threshold showing lower values for the bilateral CI listening condition (B). Speech recognition in noise evaluated using the CST showed higher values for bilateral CI listening condition even at long-term test period of seventeen months (C and D) [Citation18]. Statistical analysis: ANOVA test (p < .05). Reproduced by permission of Wolters Kluwer Health, Inc.
![Figure 17. Audiological test setup (A). HINT test hearing threshold showing lower values for the bilateral CI listening condition (B). Speech recognition in noise evaluated using the CST showed higher values for bilateral CI listening condition even at long-term test period of seventeen months (C and D) [Citation18]. Statistical analysis: ANOVA test (p < .05). Reproduced by permission of Wolters Kluwer Health, Inc.](/cms/asset/92af7269-d7a7-4705-9f0c-a2496edb97db/ioto_a_1888193_f0017_c.jpg)
HINT test included two ten sentence lists that were randomly selected without replacement, and the hearing threshold was measured when the participants correctly identified at least 50% of the presented sentences. Speech recognition at fixed SNRs was evaluated using the connected speech test (CST), which is a test of intelligibility for everyday speech that consists of twenty-four pairs of speech passages produced conversationally by a female speaker. Participants’ average speech-recognition in noise performance scores across the two unilateral conditions, the bilateral condition and the better unilateral condition as measured by the HINT and CST, are shown in , respectively, with bilateral condition offering better scores compared to other listening conditions. Performance data for the two unilateral conditions, the bilateral condition and the better unilateral condition measured at 4–7 months and 12–17 months after activation is shown in . Participants performed significantly better in the bilateral condition than in other listening conditions. The results of these experiments provide evidence of significant bilateral speech recognition in the noise of CI recipients in an environment with multiple noise sources. This advantage is presumed to be attributable to the combined effects of binaural squelch and summation.
In 2007, the first French report by Dr Polanski from Portmann Institute was published on the binaural benefits of bilateral listening with MED-EL CI devices in an elderly patient who was deaf for more than fifty years, as well as suffering from tinnitus [Citation19]. The patient had been implanted in February 2004 on the left side with MED-EL’s COMBI 40 device, with all twelve electrode channels fully intracochlearly. With the first activation of the device, the patient presented better conversational abilities without lip-reading and tinnitus disappeared. Two years later, the patient was implanted with the second implant on his right ear due to tinnitus complaints. shows the patient wearing both implants, and with such, his hearing scores were better than with unilateral listening condition tested at one-year post-operation, along with the complete absence of tinnitus when the device was switched on. Effects of long-term auditory deprivation were not seen on this patient whose hearing performance with CI was exceptional along with the tinnitus suppression.
Figure 18. Patient wearing MED-EL CI device on both ears. Speech recognition test results showing better hearing in bilateral listening condition [Citation19].
![Figure 18. Patient wearing MED-EL CI device on both ears. Speech recognition test results showing better hearing in bilateral listening condition [Citation19].](/cms/asset/1bf2fcda-1251-417c-bdbc-7cd0f9b76032/ioto_a_1888193_f0018_c.jpg)
2007 marked the tenth year of MED-EL’s journey in bilateral CI, as well as it saw a review article from the UK which analysed all published evidence up to then, supporting the trend towards bilateral CI. It also added recommendation to CI manufacturers to develop future CI systems with binaural hearing enhancing features in mind, as well as with the reduction of costs in mind to ensure the hearing restoration is made widely available [Citation20].
In the same year, the first multicentre study from the USA on MED-EL’s bilateral CI reported the speech perception results at one-year postoperation from a total of twenty-six postlingually deaf patients with relatively short duration of deafness [Citation21] ().
Figure 19. Clinicians from different centres in the USA evaluated the long-term effectiveness of bilateral CI in adults: 1The University of North Carolina School of Medicine, 2Vanderbilt University School of Medicine, 3University of Texas Southwestern, 4Dallas Otolaryngology Associates, 5Medical College of Wisconsin, and 6Research Triangle Institute.

Since different centres across the US were involved in this multicentre study, to create consistency in testing procedures, direct audio input (DAI) was used for the presentation of all test stimuli. The direct input was unattenuated but with microphone input attenuated by at least 30 dB, along with automatic gain control (AGC) circuit disabled. The results given in show the improvement in consonant-noun-consonant (CNC) scores over time (from one to twelve months test intervals), and superior hearing performance in the bilateral listening condition when compared with the better of the two unilateral conditions. In fact, this was the study that was used as a support at a later time, in the year 2018, when establishing the reimbursement of bilateral CI treatment in the US.
Figure 20. The distribution of CNC word scores in quiet (in %) is plotted as a function of the post-surgery test intervals. Horizontal lines indicate the median of each distribution, boxes span the 25th to 75th percentiles, vertical lines show the 10th to 90th percentile range, and stars indicate the minimum and maximum scores. Data for the worse of the two unilateral conditions are indicated with dark grey shading, those for the better unilateral condition with solid white shading, and those for the bilateral condition with grey and white hatching [Citation21]—statistical analysis: ANOVA test (one-tailed, p < .05). Reproduced by permission of Wolters Kluwer Health, Inc.
![Figure 20. The distribution of CNC word scores in quiet (in %) is plotted as a function of the post-surgery test intervals. Horizontal lines indicate the median of each distribution, boxes span the 25th to 75th percentiles, vertical lines show the 10th to 90th percentile range, and stars indicate the minimum and maximum scores. Data for the worse of the two unilateral conditions are indicated with dark grey shading, those for the better unilateral condition with solid white shading, and those for the bilateral condition with grey and white hatching [Citation21]—statistical analysis: ANOVA test (one-tailed, p < .05). Reproduced by permission of Wolters Kluwer Health, Inc.](/cms/asset/775bfbf9-893d-483a-8247-f002bdf072f4/ioto_a_1888193_f0020_b.jpg)
While the previous studies were involving standard audiological tests in laboratory conditions, in the year 2007 a team of specialists from the Washington University School of Medicine in the USA, along with the support of MED-EL through a research grant, demonstrated the binaural benefits in bilateral CI users of various CI brands under more challenging speech-perception tasks [Citation22]. They included seven bilateral CI users to their study, with three implanted with MED-EL’s COMBI 40+ device, two with Advanced Bionics HiRes 90 K device, and the remaining two with Cochlear™ Nucleus® device. The most challenging speech perception task for the CI patients was the SPIN (Speech Perception in Noise) test with CNC test at 70 dB SPL in the presence of twelve-talker speech babble with +8 SNR. The results were compared between the best unilaterally listening ear against the bilateral listening condition. As expected, all patients showed better hearing in the bilaterally listening condition (). The report suggested that with the technological advancements in the CI, it would make more sense to test the real binaural benefits of the bilateral CI under the most realistic and challenging test conditions.
Figure 21. Speech recognition scores in percentage correct for the best unilateral (black) and bilateral (grey) ear conditions for individual patients implanted with various CI brands. Subject 1: MED-EL; Subject 2: HiRes 90 K; Subject 3: MED-EL; Subject 4: MED-EL; Subject 5: Nucleus; Subject 6: Nucleus; Subject 7: HiRes 90 K [Citation22]. * indicates statistical significance between unilateral and bilateral CI condition. Reproduced by permission of Wolters Kluwer Health, Inc.
![Figure 21. Speech recognition scores in percentage correct for the best unilateral (black) and bilateral (grey) ear conditions for individual patients implanted with various CI brands. Subject 1: MED-EL; Subject 2: HiRes 90 K; Subject 3: MED-EL; Subject 4: MED-EL; Subject 5: Nucleus; Subject 6: Nucleus; Subject 7: HiRes 90 K [Citation22]. * indicates statistical significance between unilateral and bilateral CI condition. Reproduced by permission of Wolters Kluwer Health, Inc.](/cms/asset/00fe93d5-cd04-400b-af76-f6f454304019/ioto_a_1888193_f0021_b.jpg)
Between 2008 and 2011, several reports from across the world added valuable evidence to binaural benefits with bilateral implantation with MED-EL CI devices in both, children and adults [Citation23–33]. These well-designed studies in adults and children have documented significant auditory benefits for bilaterally implanted recipients when compared with monaural use and include improved speech perception in quiet and in noise, sound localisation, as well as subjective benefits.
Music appreciation by bilateral CI users is seen as another advantage of binaural hearing. A multicentre study from the UK, Germany and Switzerland showed that bilateral CI users with a MED-EL device enjoy significant advantages over unilaterally implanted CI users when it comes to appreciating, perceiving and accessing music for a variety of purposes [Citation31] ().
Figure 22. Clinicians from different centres who looked into the music perception of CI users: 1Nottingham Cochlear Implant Programme, UK; 2University of Würzburg (in 2009), Germany; 3University of Bern, Switzerland; 4University of Basel, Switzerland, and Technical University of Munich, Germany.

Dr Brockmeier developed the musical test that was sponsored by MED-EL. shows patient responses to questions on musical instrument identification, where bilateral CI users show superiority compared to the unilateral CI users in identifying the correct musical instruments. The difference between the unilateral and bilateral CI groups was not only in which instruments they reported recognising, but also in the number of instruments recognised correct by the bilateral CI group. All patients were postlingually deaf adults, familiar with musical genres mentioned in the questionnaire. Results from the study using the questionnaire indicate that bilateral CI users enjoy some significant advantages over unilateral users when it comes to appreciating, perceiving and accessing music.
Figure 23. The x-axis describes the various instruments recognised in musical pieces; the y-axis is the percentage of yes answers for normal hearing, bilateral CI users, and unilateral CI users [Citation31]. Histogram created from data given in Veekmans et al. [Citation31].
![Figure 23. The x-axis describes the various instruments recognised in musical pieces; the y-axis is the percentage of yes answers for normal hearing, bilateral CI users, and unilateral CI users [Citation31]. Histogram created from data given in Veekmans et al. [Citation31].](/cms/asset/994984a3-ab86-470b-9ba8-c87d3483ebc7/ioto_a_1888193_f0023_c.jpg)
1.10. Brand comparison on hearing quality and sound localisation with bilateral CI
Differences in CI technology, including electrode array length, number of stimulating channels, individual electrode contact separation distance, sound coding strategies, and other aspects amongst the CI brands, may result in differences with subjective experiences and benefits to the patient. Brand comparison in terms of superior hearing is a challenging topic to address as there are several factors to be considered, including age, pathology of HL and resulting neuronal cell survival, quality of the test setup, patient’s motivation on the day of testing – factors which may contribute to the variability in the test results. However, one of the best situations to study differences in hearing quality that arises from different CI brands is with bilaterally implanted CI patient with postlingual deafness, who is implanted with CIs from two different CI brands – preferably operated by the same surgeon to avoid any surgical technique factors. The postlingually deaf patients who have had the natural hearing in their past could better grade the quality of hearing through their CI by comparing it to their natural hearing experience.
In 2011, there were two scientific articles published from Australia (Royal Prince Alfred Hospital and Sydney Cochlear Implant Centre) which studied the difference in the quality of hearing between MED-EL CI and Cochlear™ CI, bilaterally implanted in postlingually profoundly deaf adult patients [Citation34,Citation35]. The first one was a case study from a sixty-three-year-old bilaterally deaf female who was implanted with CI devices from both abovementioned CI brands, one in each ear. After six weeks of activation, the patient described her experience with the first CI (Cochlear™) as being very mechanical: “Sounds are like two tins hitting together,” whereas sounds with the second CI (MED-EL) were described as being quite natural ().
Figure 24. Participant’s subjective assessment on hearing quality between MED-EL and other CI brand [Citation34,Citation35]. Reproduced by permission of Taylor and Francis Group.
![Figure 24. Participant’s subjective assessment on hearing quality between MED-EL and other CI brand [Citation34,Citation35]. Reproduced by permission of Taylor and Francis Group.](/cms/asset/bd1e6fd7-2280-46f8-91ce-9a7b6c975b98/ioto_a_1888193_f0024_c.jpg)
In another study involving five bilaterally implanted participants with MED-EL and Cochlear™ CI device in each ear, the choice of going for MED-EL device in their second ear was due to expected music appreciation. Given this reason for choosing MED-EL, this study focused on any significant differences between devices in terms of music appreciation. The subjective assessment was made in the form of visual analogue scales (VAS), with evaluation results ranging from 1–10 and assessing how natural, pleasant, distinct, tinny and reverberant music sounds, with each of their implants separately and with both implants together. Subjectively, four out of five thought their MED-EL device was better, much better, or very much better than their Cochlear™ device for music appreciation. Four out of five thought that music sounded more natural, less tinny and more reverberant with their MED-EL device, compared to their Cochlear™ device. However, the authors have cautioned that these participants received the Cochlear™ device first in their worse hearing ear, followed by MED-EL device in their better ear, and this could have contributed to subjectively favouring MED-EL device over the Cochlear™ device. Still, speech perception was also compared between the two ears, and it was not significantly different. What remains, none of the participants in this study subjectively favoured Cochlear™ device over MED-EL device [Citation34].
In 2018, Prof. Raine and his colleagues from the University of Bradford in the UK studied the effect of inter-implant interval and the onset of profound deafness on sound localisation with devices from different CI manufacturers [Citation36]. The study comprised of one hundred and twenty-seven bilaterally implanted children aged four years or older who were tested at least twelve months post-second implantation with various CI brands, both simultaneously and sequentially ().
Table 1. Number of children implanted bilaterally, either simultaneously or sequentially, with different CI brands.
Sound localisation testing was performed in a semi-circular array of loudspeakers at −60, −30, 0, +30, and +60 degrees azimuth, as shown in .
Figure 25. Sound localisation test setup with a child seated in front of the table and facing the centre of the arc of loudspeakers. Active (black) and inactive (grey) loudspeaker positions are shown in degrees azimuth; negative angles denote locations to the left, and positive angles denote locations to the right of the centre [Citation36]—statistical analysis: Linear multivariable regression model.
![Figure 25. Sound localisation test setup with a child seated in front of the table and facing the centre of the arc of loudspeakers. Active (black) and inactive (grey) loudspeaker positions are shown in degrees azimuth; negative angles denote locations to the left, and positive angles denote locations to the right of the centre [Citation36]—statistical analysis: Linear multivariable regression model.](/cms/asset/edded48a-66b4-443e-bb8d-906ab5008c7d/ioto_a_1888193_f0025_b.jpg)
The stimuli were pre-recorded female voices with the average presentation level of 70 dB. For each patient, sound-source localisation accuracy was measured via the root mean square error (RMSE) of thirty test trials. While the age at the onset of deafness and the inter-implant interval having a decreasing RMSE with increasing time are interesting findings, significant differences were obtained between the CI manufacturers as reported in this study, and these shall be given importance. On average, MED-EL systems were associated with more accurate sound localisation, with RMSE of 5.79° smaller than with Cochlear™, and 9.19° smaller than with Advanced Bionics, as calculated by the regression analysis. One of the reasons for more accurate sound localisation with MED-EL system, as reported in this article, is that maybe MED-EL’s front-end sound processing applies less compression to sounds louder than 65 dB SPL compared to Cochlear™ or Advanced Bionics, better-preserving ILD cues as a result.
The three studies mentioned above hint at the advantageous design of MED-EL CI devices in mimicking natural hearing [Citation34–36]. This may be attributed to the two unique features in MED-EL’s CI system which includes long and flexible electrode array, covering the entire frequency range electrically, and fine structure coding strategy that takes in both, place and time information along with no compression of the acoustic signal.
1.11. Bilateral CI in electric acoustic stimulation (EAS™)
With a profound acceptance of bilateral CI as a treatment option to restore binaural hearing in severely to profoundly deaf patients, the indication of bilateral CI with MED-EL devices was extended to patients with functional low-frequency residual hearing as well.
In 2010, Prof. Van de Heyning and his colleagues from the Antwerp Medical University in Belgium published a single-case study [Citation32]. With their forty-eight months’ study period, they concluded that with flexible electrodes, such as with the FLEXSOFT™, and with a nearly full intracochlear electrode insertion, the hearing preservation is feasible in bilateral CI condition ().
Figure 26. First bilateral CI treatment in an EAS patient by Prof. Paul Van de Heyning from Antwerp Medical University in Belgium in 2010, and Prof. Shin-Ichi Usami from Shinshu University in Japan in 2011.

In 2011, Prof. Usami and his colleagues from Shinshu University in Japan performed two bilateral CI surgeries in patients with functional low-frequency residual hearing, using a twenty-four-millimetre-long electrode array (FLEX24™) [Citation37]. In both patients, the low frequency was well preserved even at twelve months postoperation and demonstrated excellent hearing scores in noisy conditions, along with improved sound localisation abilities.
Both abovementioned reports encouraged the extension of bilateral CI as a means of treatment to patients with partial deafness in the low-frequency region.
1.12. Simultaneous versus sequential CI implantation
In 2010, the question of the optimal time for bilateral CI implantation in children was still unanswered. The overall goal of bilateral CI is to achieve similar levels of hearing performance on both sides, thereby bringing the benefits of binaural hearing. With paediatric patients, language development relies on their hearing ability and providing them with binaural hearing benefits with bilateral CI would be a logical choice [Citation38].
Unilaterally implanted children had mismatched timing of brainstem activity, resulting in a decrease in brainstem response latencies, which was not the case in children receiving bilateral CI simultaneously. Such unbalanced timing in unilaterally CI implanted children was resolved with the second implantation (nine months later), but the unbalanced timing issue persisted in patients with prolonged time of having only unilateral devices [Citation27]. Dr Sharma and her colleagues from the US evaluated the sensitive period on central auditory development in children with unilateral and bilateral CIs [Citation39]. Children who were implanted bilaterally early (<3.5 years of age) displayed rapid development in cortical auditory evoked potential (CAEP) waveform morphology, whereas late-implanted children (>7 years of age) showed aberrant waveform morphology. Children deprived of sound for more extended periods of time may have increased language learning difficulties when compared to those who were implanted within the critical period. As for the importance of language development, simultaneous bilateral implantation should be considered where possible – otherwise, as low as possible inter-implant interval between two CIs should be considered in children. As mentioned in the above section, a study by Prof. Raine and his colleagues showed that the RMS error was seen to increase with increasing inter-implant interval between the two CIs [Citation36]. This was another study which pointed out to the importance of short inter-implant interval if simultaneous implantation cannot be accommodated.
In 2019, Dr Karltorp and her colleagues from Karolinska University Hospital in Stockholm in Sweden and University of Oslo in Norway published their findings that investigated whether providing CI at 5–11 months of age had a stronger positive influence on spoken language development and speech recognition than providing it at 12–29 months of age [Citation40] ().
Figure 27. Dr Eva Karltorp and her colleagues from Karolinska University Hospital, Stockholm, Sweden and University of Oslo, Norway, investigated the importance of early CI treatment in infants on their spoken language development.

Another aim was to examine whether the medical risks associated with surgery were greater in younger patients. One hundred and three children were implanted with CI, out of which ninety-five were implanted with MED-EL CI device. Out of one hundred and three children, ninety-eight received bilateral CIs: seventy underwent a two-stage sequential bilateral implantation and twenty-eight children underwent a one-stage simultaneous bilateral implantation. The language performances of the children at the age of six years were compared between children who were implanted between 5–11 months and 12–29 months at the time of surgery. Peabody test was used to check the receptive vocabulary and the six-year estimation revealed a significant negative correlation between the age at the time of the first CI and receptive vocabulary of −1.3. This suggested that a one-year delay in surgery, on average, caused a delay of 1.3 years delay in receptive vocabulary at six years of age, as shown in .
Figure 28. Mean slope and delay calculated from individual regressions on receptive vocabulary, according to Peabody test. Graph created from data given in Karltorp et al. [Citation40].
![Figure 28. Mean slope and delay calculated from individual regressions on receptive vocabulary, according to Peabody test. Graph created from data given in Karltorp et al. [Citation40].](/cms/asset/41db24f4-67cd-4c56-a0a2-0d5fb14d6234/ioto_a_1888193_f0028_b.jpg)
The study concluded that fitting CI before a child’s first birthday was crucial for spoken language development at six years of age. Infants who received their implants before nine months of age had an even more age-typical language profile. The medical risks associated with CI surgery under nine months were no greater than for children who were older when they had CI surgery.
In 2020, a multicenter study from France looked into the French national registry of cochlear implantations from January 2012 to December 2016 to assess the incidence rate of bilateral CI and the results of bilateral CI in adults and children [Citation41]. They mainly looked at the results of CAP (category of auditory performance) and speech audiometry with monosyllabic and disyllabic word lists, before and after bilateral CI implantation. The database showed nine hundred and forty-two bilateral CIs out of which three hundred and fifty-four were implanted simultaneously, and five hundred and eighty-eight took place sequentially. Children and adults had an incidence rate of 59% and 41%, respectively. CAP scores are used to grade the hearing performance with their CI switched on by qualitatively grading their awareness and responses to various forms of sound and speech signals. Higher CAP scores relate to better hearing performance and vice versa. Within the simultaneously implanted group, the number of patients with CAP score <3 decreased after one year from 169 (85.8%) to 57 (58.8%), and the number of patients with CAP ≥5 (good understanding of speech) increased from 10 (5.1%) to 74 (37.6%) after implantation. Within the sequential group, 16 patients (9.7%) had a CAP score of <3 before receiving the second implant, compared to 3 (1.8%) afterwards, and 102 (61.8%) had a CAP score ≥5 before, and 139 (84.2%) after receiving a second implant. With the sequential implantation, the number of patients with a higher CAP score saw significant improvement after receiving first CI and did again with the second implant. In terms of speech discrimination results, simultaneous implantation group had 0% to 65% and 0% to 70% with monosyllabic and dissyllabic word list correct scores, respectively, when presented at 60 dB in noise. With the sequential implantation group, the monosyllabic word list correct was 56 ± 27% with first CI, and it increased to 62 ± 21%, whilst with the dissyllabic word list, the first CI resulted to 70 ± 27%, and that increased to 77 ± 26% with the second implant.
The authors concluded that simultaneous bilateral CI significantly improved hearing. For sequential CI, at one year, when auditory results were already excellent from the first implant, the hearing scores further significantly improved under bimodal condition.
In 2020, a report was published by Prof. Gao and his colleagues from the Union Medical College Hospital in Beijing in China, which demonstrated the safety of simultaneous bilateral CI in children aged 12–18 months, with applying standard CI surgical techniques and using MED-EL CI devices [Citation42] ().
Figure 29. Prof. Gao Zhiqiang and his colleagues from Union Medical College Hospital, who demonstrated the safety of simultaneous bilateral CI in children aged 12–18 months.

Twenty-one children aged between 12–18 months met the inclusion criteria and took part in this study. Ten patients received a unilateral CI. Nineteen patients received simultaneous bilateral CI and were operated with applying standard surgical technique (transmastoid facial recess approach with round window insertion). Safety was assessed via monitoring peri- and post-operative adverse events. No adverse events were reported in any of the patients and it was concluded that simultaneous bilateral CI can be performed using the same surgical technique as unilateral implantation, and poses no increased safety risk for children aged 1–2 years. This study was fully sponsored by MED-EL, including the cost of the CI devices and external accessories.
In terms of incremental cost-effectiveness ratio (ICER) which takes into account the cost associated with the CI treatment and hearing benefits it brings to the patient, the simultaneous implantation of bilateral CI was established to be more effective and economical than the sequential bilateral CI – as reported by Pérez-Martín et al. in 2017. This cost-effectiveness report – originating from Spain – included retrospective data of two hundred and seventy-three children [Citation43]. A similar finding was reported by Bond et al. from the UK in the year 2010, with including data of one hundred and thirty bilaterally implanted children [Citation44]. The British Cochlear Implant Group (BCIG) reports annually on the number of bilaterally implanted children and adults, either simultaneously or sequentially () [Citation45]. Between 2015–19, the simultaneously bilaterally implanted children represented a substantially larger group compared to sequentially and unilaterally implanted, which evidences a strong trend towards the former.
Figure 30. Data from BCIG showing the number of CI implantations in children unilaterally, simultaneously bilaterally, and sequentially bilaterally, which took place between 2015 and 2019 [Citation45]. Histogram taken from British Cochlear Implant Group.
![Figure 30. Data from BCIG showing the number of CI implantations in children unilaterally, simultaneously bilaterally, and sequentially bilaterally, which took place between 2015 and 2019 [Citation45]. Histogram taken from British Cochlear Implant Group.](/cms/asset/df57193c-ae49-4aba-a30f-30be2cc6296a/ioto_a_1888193_f0030_c.jpg)
Considering the pieces of evidence from abovementioned research studies on simultaneous versus sequential bilateral CI, the former has proven as a valuable contribution to oral communication amongst its recipients, and with minimal surgical risk. Therefore, whenever the financial aspects and patient’s medical condition accord, then simultaneous implantation is preferred, and especially so in children, as it could help them to have a more typical auditory cortex development, as well as it would avoid a second surgical procedure and the costs associated with it. Bilateral sequential implantation has shown better hearing benefits compared to unilateral implantation, and therefore when a situation does not allow for simultaneous bilateral implantation, then bilateral sequential implantation could be pursued.
Early activation of the CI audio processor is a technique that is being followed in some clinics with the aim of restoring hearing as soon as possible following the CI surgery, and as well to reduce the hospitalisation costs. CI surgery under local anaesthesia is another practice that is followed, especially in a group of patients who do not tolerate general anaesthesia. Group of clinicians from Saudi Arabia reported on the feasibility of audio processor activation one day after the CI surgery, including the group of patients that underwent CI surgery under local anaesthesia [Citation46,Citation47] ). They concluded that early implant activation did not impact the healing process of the incision site, and also the evolution of electrode impedance and stimulation levels were consistent with the standard four weeks postoperative activation.
Figure 31. Clinicians from Saudi Arabia, who were all part of the early activation and CI surgery under local anaesthesia studies.

Early activation of the CI audio processor, although it is reported safe, depends on the individual clinic and operating surgeons’ comfort of choosing such a technique or not. Nevertheless, this is one additional possibility of encouragement for bilateral CI either simultaneously or sequentially.
From all the evidences given in this section, is it clear that performing simultaneous CI implantation on both sides is safe from the surgical point of view, including in children. The trend is moving towards simultaneous rather than sequential implantation of bilateral CI and it adds cost-benefit for both, the healthcare system and the patients.
1.13. Reimbursement for bilateral CI from the healthcare systems
The therapeutic impact of CI has transformative effects on patients with severe-to-profound hearing impairment. How these benefits confer improvement in health-related quality of life, has been the focus of many clinical studies. Cost-utility is a term often used in medical device-related treatment, and it is expressed as a function of the net cost of treatment to the net effect in quality-adjusted life years. There were several studies () performed which investigated the cost-utility ratio of the CI treatment, concluding that the cost associated with the CI treatment, including the bilateral CI, is highly effective for both, the patient as well as the healthcare system in the long run [Citation48–50].
Table 2. Summary of studies that reported on the cost-effectiveness associated with bilateral CI treatment.
Originating from different parts of the world, all of the studies point towards overall cost-effectiveness of bilateral over unilateral and in particular, to the simultaneous bilateral implantation.
Health Utility Index (HUI®) is another term that relates to the generic health-related quality of life measurement tool. HUI® is the perfect health-related quality of life score. In 2008, a group from Marion and Indianapolis, USA, evaluated the improvements in quality of life of twenty-three bilaterally implanted CI recipients, implanted with various CI brands, including MED-EL [Citation51]. For all twenty-three participants from this study, HUI® showed a score of 0.33 on average before CI implantation, which increased to 0.69 after receiving their first CI. With the second CI, the HUI® score reached a mean of 0.81, which is close to 1.0 – the perfect health-related quality of life score.
The purpose of all mentioned research studies from this article is to demonstrate the benefits of binaural hearing with bilateral CI – which shall ultimately help convince the healthcare systems to reimburse the costs associated with the treatment.
Within Europe, Switzerland was the first country to reimburse the cost of bilateral CI and Prof. Mattheus Vischer was instrumental in convincing the healthcare system on the importance of bilateral CI, especially in children. In Germany, the social insurance code (SGBV) regulates adequate treatment of both ears individually. Legal counsel for early cases from the year 1997 on, lead to precedence cases and coverage of most second CIs by the health insurance before the year 2005. In Austria, it was never a problem for the patients to get the second CI cost reimbursed by the healthcare system.
In 2018, the healthcare system in the USA, Canada, and almost all of the European Union (EU) countries had agreed to reimburse the cost of bilateral CI treatment – either sequential or simultaneous – in children and adults, complimenting all the research efforts that took place since 1999.
1.14. Communicating science through gaming
Science should be easy to understand. However, concepts from the scientific community may get across as overly complicated sometimes. To simplify the context and the full benefits of bilateral CI, MED-EL has taken the challenge as an opportunity to come up with a gaming concept which is available for anyone to play and grasp. Switch-On-Life was created to help with understanding the importance of binaural hearing, what it means, and how it helps with benefiting our daily lives ().
Figure 32. Experts from Citation1Antwerp Medical University, Belgium, 2Bradford Teaching Hospitals, UK, 3Arizona State University, USA, and 4NYU Grossman School of Medicine, USA, supported the development of Switch-On-Life web-platform.

In 2020, MED-EL launched an interactive web-platform (www.switch-on-life.com) which offers a playful experience on hearing, hearing loss and hearing implant technology, and which enables the user to discover the importance of hearing with two ears. Switch-On-Life – a project conceived and led by Dr Schleich from MED-EL – aims to provide the realisation of how basic scientific findings and observations are translated to MED-EL’s CI technology and the clinical routine. Thanks to Prof. Van de Heyning, Prof. Raine, Dr Dorman and Dr Landsberger and their technical insights, this interactive web-platform was made possible.
1.15. Conclusion
In 2019, among MED-EL CI devices implanted bilaterally across the world, two-thirds were in children – this indicates the importance of bilateral CI treatment given to children as the binaural hearing helps them with success in their personal life and career at later stages. The best example is Mr Max Röder from Germany, who, in 1998, was the first child to receive bilateral CI . The binaural benefits offered by bilateral CI allowed him to speak and hear with capacities of an ordinary hearing person, which helped him throughout his journey to reach the successful academic graduation from his bachelor studies in computer sciences from the University of Würzburg in Germany in 2018. In the year 2020, Mr Röder found an employment opportunity at MED-EL and was appointed as a development engineer in the Research and Development department.
Just like Mr Röder, there are thousands of children across the world who would have benefitted from the bilateral CI, funded either by the national healthcare systems or privately. Considering the importance of binaural hearing, the bilateral CI treatment option should become the gold standard in treating bilaterally deaf patients, supported by the healthcare system in every county.
Bilateral CI restores binaural hearing in both, profoundly deaf and partially deaf patients. Scientific collaboration between clinicians from clinics across the world and researchers from MED-EL has brought the bilateral CI solution to the state-of-the-art with restoring binaural hearing. While every CI brand may claim to be technologically superior, it is the patient who uses the technology and can describe the actual CI hearing experience. The three mentioned studies which compared the CI hearing quality, saw a preference towards experiencing a naturally sounding hearing with their MED-EL CI device, over any mechanically sounding CI, as reported by the users implanted with other CI brands. Natural hearing that comes from MED-EL CI device is mainly due to its sound coding strategies, inspired from nature by mimicking both, time and place coding – the two top distinctive features of MED-EL – carrying fine structure information, as well as due to the electrode arrays with their tonotopic distribution over the entire cochlear length. While the device technology is one of the aspects for successful hearing through CI, another aspect would be the time at which it is provided to the patient. For paediatric patients, it is their first two to three years of life that plays the critical role with obtaining the optimal benefits through a CI technology, and the latter shall reach them during that time to provide them with the communication means through binaural hearing. This is exactly what happened with Mr Röder, who received his bilateral CI before the age of four in 1998, and which helped him to develop his communication means thoroughly. Today, he is as successful as anyone else with normal hearing. The journey of Mr Röder with his bilateral CI is one single success story that could well represent many other bilateral CI users’ experience. Although the healthcare system is in great shape in the Western world, there is a space for improvement in the rest of the world, and more specifically, an immense potential lays in allowing the bilateral hearing to every single patient in need, and in advancing the necessary reimbursement systems which currently obstruct this.
Acknowledgments
The authors would gratefully like to acknowledge the key contributors to the development of the subject matter. Their contributions are outlined in this article. The authors further acknowledge Reinhold Schatzer from MED-EL for his valuable input and comments during several rounds of review meetings that contributed to the final version of this article.
Disclosure statement
This article is sponsored by MED-EL and has not undergone the regular peer-review process of Acta Oto-Laryngologica. Both the authors are affiliated with MED-EL.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Avan P, Giraudet F, Büki B. Importance of binaural hearing. Audiol Neurootol. 2015;20(Suppl 1):3–6.
- Wanna GB, Gifford RH, McRackan TR, et al. Bilateral cochlear implantation. Otolaryngol Clin North Am. 2012;45(1):81–89.
- Müller J, Schön F, Helms J. Speech understanding in quiet and noise in bilateral users of the MED-EL COMBI 40/40+ cochlear implant system. Ear Hear. 2002;23(3):198–206.
- Drela M, Haber K, Wrukowska I, et al. Qualification of unilateral cochlear implant recipients for a second device. Otolaryngol Pol. 2019;73(6):8–17.
- Newborn and infant hearing screening. WHO; 2010. Available from: https://www.who.int/blindness/publications/Newborn_and_Infant_Hearing_Screening_Report.pdf?ua=1.
- Balkany T, Boggess W, Dinner B. Binaural cochlear implantation: comparison of 3M/House and Nucleus 22 devices with evidence of sensory integration. Laryngoscope. 1988;98(10):1040–1043.
- Hochmair I, Schulz E, Moser L, et al. The HSM sentence test as a tool for evaluating the speech understanding in noise of cochlear implant users. Am J Otol. 1997;18(6 Suppl):S83.
- Müller J, Schön F, Helms J. Bilateral cochlear implant- new aspects for the future? Adv Otorhinolaryngol. 2000;57:22–27.
- Schön F, Müller J, Helms J. Speech reception thresholds obtained in a symmetrical four-loudspeaker arrangement from bilateral users of MED-EL cochlear implants. Otol Neurotol. 2002;23(5):710–714.
- Stark T, Müller J, Vischer M, et al. Multicenter study on bilateral cochlear implantation. Cochlear implants: an update. The Hague, Netherlands: Kugler Publications; 2002. p. 523–526.
- Kühn-Inacker H, Shehata-Dieler W, Müller J, et al. Bilateral cochlear implants: a way to optimize auditory perception abilities in deaf children? Int J Pediatr Otorhinolaryngol. 2004;68(10):1257–1266.
- Au DK, Hui Y, Wei WI. Superiority of bilateral cochlear implantation over unilateral cochlear implantation in tone discrimination in Chinese patients. Am J Otolaryngol. 2003;24(1):19–23.
- Kong W, Yu L, Xu Y, et al. Benefit of bilateral cochlear implantation on congenital prelingually deafened Chinese-speaking children. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2003;17(10):577–579.
- Nopp P, Schleich P, D'Haese P. Sound localization in bilateral users of MED-EL COMBI 40/40+ cochlear implants. Ear Hear. 2004;25(3):205–214.
- Schön f, Müller J, Helms J, et al. Sound localisation and sensitivity to interaural cues in bilateral users of the MED-EL COMBI 40/40+ cochlear implant system. Otol Neurotol. 2005;26(3):429–437.
- Litovsky RY, Johnstone PM, Godar S. Benefits of bilateral cochlear implants and/or hearing aids in children. Int J Aud. 2006;45(sup1):78–S91.
- Senn P, Kompis M, Vischer M, et al. Minimum audible angle, just noticeable interaural differences and speech intelligibility with bilateral cochlear implants using clinical speech processors. Audiol Neurootol. 2005;10(6):342–352.
- Ricketts T, Grantham DS, Ashmead DH, et al. Speech recognition for unilateral and bilateral cochlear implant modes in the presence of uncorrelated noise sources. Ear Hear. 2006;27(6):763–773.
- Portmann D, Felix F, Negrevergne M, et al. Bilateral cochlear implantation in a patient with long-term deafness. Rev Laryngol Otol Rhinol (Bord). 2007;128(1–2):65–68.
- Murphy J, O'Donoghue G. Bilateral cochlear implantation: an evidence-based medicine evaluation. Laryngoscope. 2007;117(8):1412–1418.
- Buss E, Pillsbury HC, Buchman CA, et al. Multicenter US bilateral MED-EL cochlear implantation study: speech perception over the first year of use. Ear Hear. 2008;29(1):20–32.
- Wackym PA, Runge-Samuelson CL, Firszt JB, et al. More challenging speech-perception tasks demonstrate binaural benefit in bilateral cochlear implant users. Ear Hear. 2007;28(2 Suppl):80S–85S.
- Zeitler DM, Kessler MA, Terushkin V, et al. Speech perception benefits of sequential bilateral cochelar implantation in children and adults: a retrospective analysis. Otol Neurotol. 2008;29(3):314–325.
- Eapen RJ, Buss E, Adunka MC, et al. Hearing-in-noise benefits after bilateral simultaneous cochlear implantation continue to improve 4 years after implantation. Otol Neurotol. 2009;30(2):153–159.
- Grantham DW, Ashmead DH, Ricketts TA, et al. Interaural time and level difference threshold for acoustically presented signals in post-lingually deafened adults fitted with bilateral cochlear implants using CIS + processing. Ear Hear. 2008;29(1):33–44.
- Nava E, Bottari D, Portioli G, et al. Hearing again with two ears: recovery of spatial hearing after bilateral cochlear implantation. Neuropsychologia. 2009;47(3):928–932.
- Basura GJ, Eapen R, Buchman CA. Bilateral cochlear implantation: current concepts, indications, and results. Laryngoscope. 2009;119(12):2395–2401.
- Budenz CL, Roland JT, Jr, Babb J, et al. Effect of cochlear implant technology in sequentially bilaterally implanted adults. Otol Neurotol. 2009;30(6):731–735.
- Migirov L, Kronenberg J. Bilateral, simultaneous cochlear implantation in children: surgical considerations. J Laryngol Otol. 2009;123(8):837–839.
- Uchanski RM, Davidson LS, Quadrizius S, et al. Two ears and two (or more?) devices: a pediatric case study of bilateral profound hearing loss. Trends Amplif. 2009;13(2):107–123.
- Veekmans K, Ressel L, Mueller J, et al. Comparison of music perception in bilateral and unilateral cochlear implant users and normal-hearing subjects. Audiol Neurootol. 2009;14(5):315–326.
- Kleine Punte A, Vermeire K, Van de Heyning P. Bilateral electric acoustic stimulation: a comparison of partial and deep cochlear electrode insertion. A longitudinal case study. Adv Otorhinolaryngol. 2010;67:144–152.
- Obrycka A, Skarzynski H, Lorens A, et al. Assessment of benefit after bilateral cochlear implantation in children. Cochlear Implants Int. 2010;11(Suppl 1):79–82.
- Withers SJ, Gibson WP, Greenberg SL, et al. Comparison of outcomes in a case of bilateral cochlear implantation using devices manufactured by two different implant companies (Cochlear Corporation and Med-El). Cochlear Implants Int. 2011;12(2):124–126.
- Harris RL, Gibson WP, Johnson M, et al. Intra-individual assessment of speech and music perception in cochlear implant users with contralateral Cochlear™ and MED-EL™ systems. Acta Otolaryngol. 2011;131(12):1270–1278.
- Killan C, Scally A, Killan E, et al. Factors affecting sound-source localisation in children with simultaneous or sequential bilateral cochlear implants. Ear Hear. 2019;40(4):870–877.
- Moteki H, Kitoh R, Tsukada K, et al. The advantages of sound localization and speech perception of bilateral electric acoustic stimulation. Acta Otolaryngol. 2015;135(2):147–153.
- Gordon KA, Deighton MR, Abbasalipour P, et al. Perception of binaural cues develops in children who are deaf through bilateral cochlear implantation. PLoS One. 2014;9(12):e114841
- Sharma A, Nash AA, Dorman M. Cortical development, plasticity and re-organization in children with cochlear implants. J Commun Disord. 2009;42(4):272–279.
- Karltorp E, Eklöf M, Östlund E, et al. Cochlear implants before 9 months of age led to more natural spoken language development without increased surgical risks. Acta Paediatr. 2020;109(2):332–341.
- Puechmaille M. The French national cochlear implant registry (EPIIC): bilateral cochlear implantation. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137:S1879–S7296.
- Gao Z, Wang S, Yang H, et al. Simultaneous bilateral cochlear implantation in children aged 12‒18 months is safe and can be performed using standard cochlear implant surgical techniques. Eur Arch Otorhinolaryngol. 2020;277(8):2193–2197.
- Pérez-Martín J, Artaso MA, Díez FJ. Cost-effectiveness of pediatric bilateral cochlear implantation in Spain. Laryngoscope. 2017;127(12):2866–2872.
- Bond M, Mealing S, Anderson R, et al. The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model. Health Technol Assess. 2009;13(44):1–330.
- https://www.bcig.org.uk/wp-content/uploads/2019/02/2018.09.18-Report-to-Council-Data-Collection-FY17-18a.pdf.
- Hagr A, Garadat SN, Al-Momani M, et al. Feasibility of one-day activation in cochlear implant recipients. Int J Audiol. 2015;54(5):323–328.
- Aldhafeeri AM, Saleh S, Almuhawas F, et al. Feasibility of day surgery for cochlear implantation under conscious sedation with same-day fitting. Int Adv Otol. 2020;16(3):303–308.
- Smulders YE, van Zon A, Stegeman I, et al. Cost-utility of bilateral versus unilateral cochlear implantation in adults: a randomized controlled trial. Otol Neurotol. 2016;37(1):38–45.
- Chen JM, Amoodi H, Mittmann N. Cost-utility analysis of bilateral cochlear implantation in adults: a health economic assessment from the perspective of a publicly funded program. Laryngoscope. 2014;124(6):1452–1458.
- Trinidade A, Page JC, Kennett S, et al. Simultaneous versus sequential bilateral cochlear implants in adults: cost analysis in a US setting. Laryngoscope. 2017;127(11):2615–2618.
- Bichey BG, Miyamoto RT. Outcomes in bilateral cochlear implantation. Otolaryngol Head Neck Surg. 2008;138(5):655–661.




