Abstract
Background: Inflammatory bowel disease (IBD) is a chronic, inflammatory relapsing disease with increasing incidence. IBD research and long-term follow-up of patients have, however, been hampered by lack of detailed data on disease phenotype, patient-reported outcome measures, Physician Global Assessment, disease activity, and hospital-administered drugs.
Aim: To review the Swedish IBD quality register (SWIBREG).
Methods: Review of SWIBREG including questionnaire data from users and patients.
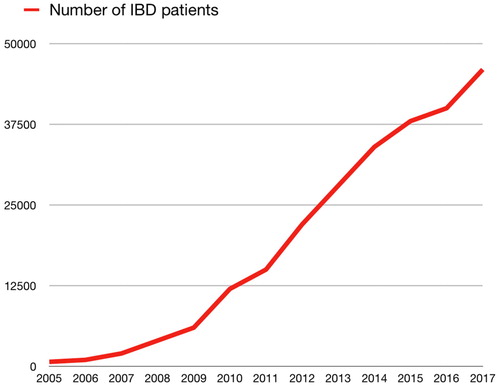
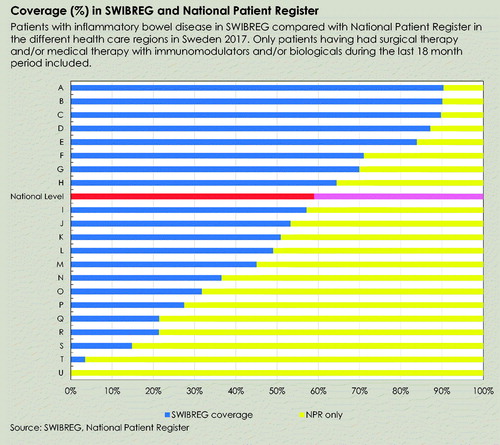
Results: SWIBREG was launched in 2005, and as of April 2019, contains 46,400 patients with IBD (Crohn’s disease: n = 15,705, ulcerative colitis: n = 21,540, IBD unclassified and other colitis (including e.g., microscopic colitis): n = 9155). Of these IBD patients, 7778 had been diagnosed in childhood (16.8%). Earlier research has shown that combining SWIBREG and the Swedish National Patient Register (NPR) yields a positive predictive value of 100% (95%CI = 95–100%) for having a diagnosis of IBD. Moreover, out of all patients in the NPR with a diagnosis of IBD plus either IBD-related surgery or immunomodulatory/biological treatment during the past 18 months, SWIBREG covers 59.0%. SWIBREG records not only information on conventional therapies but also on biological treatment, surgery, smoking, disease activity, patient-reported outcome measures (PROMs), and patient-experienced measures (PREMs). Data are presented through a graphical decision support system.
Conclusion: SWIBREG benefits patients with IBD, and offers an ideal opportunity for healthcare personnel and researchers to examine disease phenotype and activity, PROMs/PREMs, and hospital-administered drugs in patients with IBD.
Introduction
Inflammatory bowel disease (IBD) is an umbrella term for chronic inflammation disorders of the gastrointestinal tract. Crohn's disease (CD) and ulcerative colitis (UC) are two of the most common types of IBD. A less common disease entity is unclassified IBD (IBD-U). IBD may occur at any age, including childhood [Citation1–3], but the incidence peaks between ages 15 and 35 years [Citation4]. Patients require regular check-ups and are sometimes admitted to the hospital [Citation5]. In recent years, targeted drugs, including biological agents, have become more frequent, despite limited data on potential long-term side effects.
The incidence of IBD is still increasing in recently industrialised countries, even though plateauing or even declining incidence rates have been reported in some regions of the world [Citation6]. Changes in incidence cannot be solely explained by genetic variants given such components are stable over time (except for the contribution from migration). Instead, aetiological research on the changing incidence of IBD has focussed on environmental factors, such as smoking [Citation7], diet, and the microbiota [Citation8] (the latter being influenced by, for instance, antibiotic use [Citation9]). IBD affects men and women almost equally [Citation10] and has a substantial heritability [Citation11].
Management of IBD is based on patient symptoms, signs, laboratory measures, endoscopy, imaging, and histopathology. However, healthcare personnel cannot easily retrieve data on either individuals or groups of IBD patients. In addition, current government-administered registers offer few opportunities for benchmarking and between-site comparisons of quality of care. Many relevant parameters are not available through Swedish national government-administered registers. Finally it has been suggested that ‘real-world’ data may better reflect routine clinical care than controlled trials [Citation12], and, hence, also research might benefit from an IBD quality register (QR).
For these reasons, several Swedish physicians with a special interest in IBD started the Swedish QR for IBD (SWIBREG) in 2005. Since then, it has also become clear that access to detailed digital patient data coupled with the parallel growth of computing-power and use of medical algorithm, lends itself to the creation of medical decision systems to the benefit of patients.
This paper describes key aspects of the Swedish IBD QR to improve quality of care, decrease disease activity, prevent disease complications, facilitate an equal healthcare for IBD patients, and enhance the quality of life (QoL) in both paediatric and adult patients with IBD in Sweden.
The Swedish patient data law defines QRs as follows [Citation13,Citation14]:
A QR is an automated and structured collection of personal data that was initiated with the purpose to systematically and continuously develop and safeguard quality of care. A national or regional QR refers to a QR in which personal data have been collected from several caregivers and which allows for comparisons within healthcare at a national or regional level.
Results
SWIBREG currently covers 46,400 patients with IBD (CD: n = 15,705, UC: n = 21,540, IBD-U and other colitis (including e.g. microscopic colitis): n = 9155).
Diagnostic data in the register were recently validated against the Copenhagen IBD criteria [Citation15,Citation16]. This validation found that, for patients with an IBD diagnosis in SWIBREG plus the Swedish NPR, the positive predictive value was 100% (95%CI = 95–100%), with a high value also specifically for UC (97%; 95%CI = 82–100%) but lower for CD (87%; 95%CI = 72–96%) when diagnoses were defined according to the Copenhagen criteria [Citation17].
To promote and facilitate the use of SWIBREG, educational activities are an integral part of the work of the steering group. In the past 5–10 years, many new users have been added. Education usually takes the form of annual national and local workshops, lectures, and educational films. A webpage (www.swibreg.se) with links to relevant professional websites displays the number of included patients and contains resources for professionals involved in IBD care.
History of SWIBREG
SWIBREG was launched in 2005. Initially, the register contained three modules: module A primarily contained information on personal identity number (PIN), diagnosis, address, and surgery; module B focussed on individual visits, including drug use, surgery, ongoing medication, and QoL; and module C which was without content in 2006. In 2012, a decision was made to change the platform of the register and at that time SWIBREG merged with a web-based clinical decision support model called IBD Care. This merger allowed the register to integrate an online support tool for all clinicians offering an intuitive overview of each patient’s disease history while simultaneously offering each unit to benchmark the outcome of their care with other units as well as with a national average. Over time, an increasing number of departments have joined SWIBREG and the number of patients included in the QR has increased significantly, attaining a national coverage of 59.0% in 2018 (). presents the coverage in 2017 according to calculations by the National Board of Health and Welfare (see table legend for a description of the denominator). The coverage of SWIBREG at different hospitals ranges between 0 and 100% of the patients in the NPR [Citation18]. Four hospitals have 100% coverage and 12 have more than a 90% coverage using the NPR as the gold standard.
Structure of the register
Steering group
The SWIBREG steering group consists of physicians, nurses, and two representatives from relevant patient organisations (Mag- och tarmförbundet and ILCO – Tarm-uro och stomiförbundet). The following associations are represented in the steering group: the Swedish Society of Gastroenterology, the Swedish Society for Colon and Rectal Surgeons, the Swedish Society of Paediatrics, and the Swedish Society for Nurses in gastrointestinal (GI) Diseases. Formally, one member of the steering group is a lawyer representing the region of Östergötland, the healthcare region that is legally responsible for SWIBREG. The steering group seeks the equal representation of men and women and to have representatives from both small and large hospitals. Since 2013, SWIBREG collaborates with the Registry and Competence Centre of Southeast Sweden (RSCO). This centre offers advice on legal, IT, and statistical matters. SWIBREG also receives support from the National PROM Centre. Members of the steering group can be found on the SWIBREG website: www.swibreg.se.
Patient perspective
The Swedish Patient Organisation for gastrointestinal disease, Mag- och tarmförbundet (web page: http://www.magotarm.se) and ILCO, a patient organisation focussing on patients who have received a stoma (web page: http://www.ilco.nu), are both actively engaged in the development of SWIBREG and in the future direction of this QR. Each of the societies is represented on the steering board of SWIBREG, with the main goal of implementing a collective vision for patient-centred healthcare. Among the challenges facing Swedish IBD care and SWIBREG are geographic differences in access to IBD care and the quality of this care.
Funding of SWIBREG
Since 2012, SWIBREG is co-funded by the Swedish government, as well as by the Swedish Association of Local Authorities and Regions (SALAR).
Ethics
The legal regulations for QRs stipulate that a patient must be informed about SWIBREG before being recorded in the register. Patients, without giving reasons, can decline participation in the QR. The non-compulsory nature of SWIBREG contrasts with compulsory participation in the National Healthcare Registers [Citation19]. Additional details of the legal framework are presented in the QR overview by Emilsson et al. [Citation14]. Participants always have the right to exit SWIBREG.
Decision support system
A mainstay of SWIBREG is the decision support system (). The system is graphical and has the following major elements: inflammatory markers, drug treatment, measures of clinical disease activity, endoscopic activity, surgery, and QoL. In addition, the legend below the graph presents information on date of diagnosis, age at first diagnosis, whether the patient is included in any SWIBREG-administered study, and anatomic distribution of inflammation and CD behaviour [Citation20].
In a typical adult patient, the graph shows the temporal relationship between faecal calprotectin, the Mayo and Walmsley score for UC, and HBI for CD, and start and stop of medications (in the Figure prednisolone, Pred-clysma, Colifoam, Purinethol, Azathioprine, Stelara, Humira, and Entyvio are listed). The trends signal improvements (downwards = lower values) or exacerbations (upwards = higher values). The relationship between the lines representing disease activity and medication use can guide the clinician to detect patterns and poor vs. good response to certain drugs. At the same time, the graph can help patients and their family better understand the disease trajectory, and potentially even predict future disease activity (everything moving towards either the better or the worse). Importantly, the overview of medications minimises the risk of medication errors because patients can easily verify whether they use the drugs registered in the graph or not. Finally, the graph can be used at multi-disciplinary team conferences when patients are discussed or when patients are transferred from one unit to another.
The dashboard also includes information on the Physician Global Assessment (PGA) (as part of the Mayo Score) and the patient-reported QoL measure Short Health Scale (SHS). These variables (as well as endoscopy and surgery) are registered in two content domains (date of measurement and actual value/level). Red colour signals poor wellbeing and poor function while green colour denotes good wellbeing (note the corresponding faecal calprotectin levels). For endoscopy recording in the graph, red is equal to more severe disease activity.
While not tied to the graph, additional data are recorded in an accumulative view below the graph, allowing the physician to compare values over time (e.g., haemoglobin levels, leukocytes, thrombocytes, C-reactive protein, albumin, and creatinine). Single clinical symptoms are recorded in a similar fashion and include the number of stools per day, the number of loose stools per day, nightly stools, urgency, bloody stools, abdominal pain, wellbeing, and abdominal mass. Serum levels of biologics are recorded in the register but not tied to the graph.
Differences in degree and extent of inflammation explain some of the differences in disease symptoms between patients. In UC, bloody diarrhoea is a cardinal symptom, but accompanying symptoms may include abdominal pain, and in severe cases fever, malnutrition, and weight loss. In CD, symptoms are usually more difficult to interpret. Abdominal pain is common in CD, but also occurs in healthy individuals, and mild/early CD may be misinterpreted as functional abdominal pain, especially in the absence of elevated inflammatory markers. Typical of CD is also peri-anal disease, malnutrition, and poor growth.
In both CD and UC, a substantial proportion of patients suffer from extraintestinal manifestations from, for example, joints, the skin, eyes, and the biliary tract [Citation21]. All these symptoms are recorded in SWIBREG.
Web interface and question tool
SWIBREG is only available to registered users (selected healthcare personnel in Sweden). User names and passwords are obtained at a request from the local SWIBREG administrator. After logging in, the user is greeted by several tabs: Patient search, Patient lists, Patient data, Quality assurance, Question tool, My data, and finally, About SWIBREG.
To the upper left of the welcome page is a patient search box. In the QR, the patients are listed by name, PIN [Citation22], and a unique SWIBREG number to maximise clarity.
Patients can be identified by the care-givers at the patients’ treating unit through searching for any of these terms.
Through the web page, all users can access a question tool. Using a combination of search terms, it is possible to identify the number of relevant patients (e.g., number of girls aged <18 years). For instance, the user can create his/her own cohort of female UC patients with biological treatment and investigate how they score their health-related QoL (HRQOL). Alternatively, he/she can study another cohort with all patients with CD in the small bowel to investigate how many are treated with biologics or have perianal disease, as well as those who have undergone surgery.
Patient lists
The next tab allows the users to study certain groups of patients (Swedish: Patientlistor). Here, it is possible to access all patients or the last 10 patients. Patient groups can also be created according to disease activity, type of treatment, participation in SWIBREG-administered studies, home monitoring of disease activity, and patients who have signed on to the electronic communication tool called 1177 Health Care Guide’s e-services (Swedish: 1177 vårdguidens e-tjänster). Finally, it is possible to create cohorts of patients for which data need to be supplemented (e.g., patients who might be candidates for certain treatments or studies).
Patient lists can be sorted according to disease activity, type of treatment, ongoing medication, and last healthcare contact. The lists allow the caring physician or nurse to concentrate on patients with the most severe disease or, for example, to focus on both biological and immunomodulating therapy.
Parameters measured in SWIBREG
Disease phenotypes
The disease phenotype is categorised based on the Montreal classification for adults and the Paris classification for children) [Citation20,Citation23], including anatomic distribution of inflammation, behaviour, and severity.
Endoscopy
Besides symptoms and laboratory measures, endoscopy constitutes an important means for follow-up and assessment. It allows physicians to clarify patients according to the Montreal classification. Among patients with UC, each segment is scored according to the endoscopic Mayo score [Citation24]. Correspondingly, the presence of ulcers is recorded for each segment among patients with CD and predicts the 10-year-risk of IBD surgery [Citation25].
Medications
Although the Swedish Prescribed Drug Register started in July 2005 [Citation26], it does not usually cover intravenously administered biological treatment. Exceptions occur, and some infusion drugs are also registered in the NPR (100% of biologics are currently recorded in Stockholm County). An estimated 30% of infusion biologics given in Sweden are currently recorded in all registers combined, while the overall coverage of all biologics is estimated to be >70% [Citation27]. An increasing number of counties and hospitals register >90% of all IBD biologics, including infusion biologics. Apheresis is also recorded in SWIBREG.
Targeted therapies
The introduction of biologics for the treatment of patients with moderate to severe CD and UC has translated into major changes of the treatment landscape of IBD and led to marked improvements in disease control and QoL. Even though the efficacy of biologics has been clearly demonstrated in randomised clinical trials, some aspects of their long-term efficacy and potential side effects are less well characterised. Although the Swedish Prescribed Drug Register offers opportunities to follow-up drug treatment, SWIBREG contains more granular data, including data on intravenous use of biological drugs.
Biological drugs are defined as medications produced using living cells or tissues. The first effective biological drugs inhibited TNF-alpha [Citation28]. Currently, there are three TNF inhibitors in use in Sweden: Infliximab, Adalimumab, and Golimumab.
In recent years, Vedolizumab (alpha4beta7-integrin-inhibitor [Citation29–31]) has been introduced in Sweden. In 2016, according to SWIBREG, 336 patients had used vedolizumab in that year. In late 2016, also Ustekinumab was introduced in Sweden and so far 554 patients have been registered with this drug through SWIBREG; compared with 84 patients on tofacitinib. Research in newer biological drugs has focussed on switching between drugs and drug-specific efficacy.
Surgery
SWIBREG aims to record all incident surgery. From a research perspective, the QR still has low coverage. IBD surgery is rare and in the whole of Sweden only 471 IBD patients underwent IBD-related abdominal surgery between July 1, 2017 and December 31, 2018 (personal communication from the Swedish National Board of Health and Welfare, 2019). Surgery for IBD is often regarded as a failure of medical treatment, but should rather be seen as an important complement and can sometimes be life-saving and significantly enhance the QoL of patients [Citation32,Citation33]. Given the complexity of IBD surgery and the large costs involved, IBD surgery is more and more concentrated to a small number of regional, or even national centres. This is not formalised in Sweden, e.g., like restorative procedures after subtotal colectomy in Denmark [Citation34], but is currently being discussed. Only a minority of IBD patients undergoing colectomy have undergone reconstructive surgery [Citation35].
Until 2019, there were 3248 colectomies recorded in SWIBREG (colectomies in UC: n = 2022; in CD: n = 1155; in IBD-U: n = 71). In addition, 973 small bowel resections in patients with IBD were recorded. Small bowel resections are sometimes replaced by strictureplasty or endoscopic balloon dilatation, and until 2019, 124 and 365 have been reported, respectively. Perianal surgery (mainly in CD) was reported in 987 patients until 2019.
Smoking
With the exception of the Medical Birth Register [Citation36], none of the government-administered registers in Sweden contain data on smoking. Smoking has been inversely linked to UC and positively linked to CD [Citation37]. Until recently, smoking information was only available in a subset of individuals (7% of patients in 2012), but in 2018 there were smoking data on 46% of patients recorded in SWIBREG.
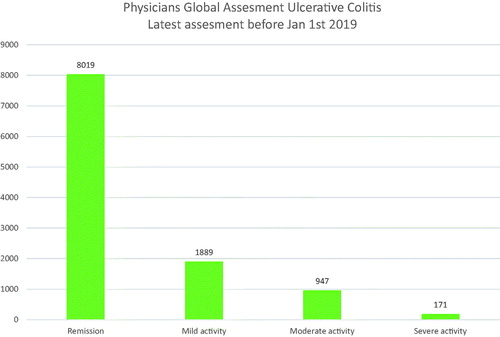
Disease activity and quality of life (HRQoL)
IBD is a chronic disease and there is currently no curative treatment. Hence, most patients will suffer from relapsing or continuous disease activity. As expected, IBD affects the health-related quality of life (HRQoL) in patients [Citation38]. SWIBREG records a number of disease indices, the most important being in adults: the Harvey Bradshaw Index (HBI) for CD and the Mayo Score/Partial Mayo Score for UC. In children, the Paediatric Ulcerative Colitis Activity Index (PUCAI) in UC, and the short Paediatric Crohn’s Disease Activity Index (PCDAI) and HBI in CD are recorded in SWIBREG. The PGA is available for all children with IBD.
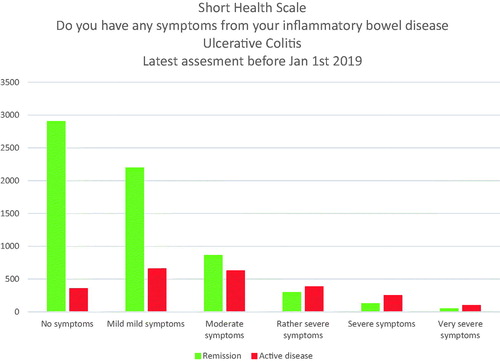
Unique to the Swedish setting is the SHS [Citation39–41] (). This is a patient-derived QoL scale measured using a six-point Likert scale. The SHS is based on four dimensions:
How severe are the symptoms you suffer from your bowel disease?
How much worry does your bowel disease cause?
How is your general feeling of well-being?
Do your bowel problems interfere with your activities in daily life?
SHS is also used in children [Citation42].
The vast majority of IBD patients are in remission (), with most reporting no or only mild symptoms ().
In addition to SHS, which is a disease-specific questionnaire, SWIBREG also records EQ-5D. EQ-5D is a standardised instrument developed by the EuroQol Group as a measure of health-related QoL that can be used in a wide range of health conditions and treatments (https://euroqol.org/euroqol). The EQ-5D consists of a descriptive system and the EQ VAS.
SWIBREG is meant to be the working tool for all healthcare personnel involved in IBD. Since 2015, the register records data on patient-reported experience measures (PREMs) and before that also on PROMs. Patients, their families, and the healthcare professionals often regard these measures as vital to deliver effective and good healthcare. PROMs include, for instance, patient-reported symptoms and general wellbeing. PREMs include questions about experience regarding given information, participation, accessibility, and the behaviour of healthcare professionals. Three- and four-point Likert scales are used. A delicate issue in recording patient-reported measures is that the patient must be assured that critical responses (‘I lack trust in my physician’) will not affect their future care. Between 2015 and 2019, PREM data were recorded in 5087 patients. PROM measurement is recommended before or at every contact with healthcare professionals. We aim to measure PREMs annually.
Data quality and quality control
In its early phase, SWIBREG’s primary ambition was to identify all patients with IBD. Now, the QR has raised the bar, increasingly focussing on phenotypic data, medication use, and quality of data. The QR has recently introduced a data quality scale from 0 to 10, with 0 denoting very poor data quality and 10 denoting excellent data quality. All centres are graded according to this scale. The data quality in SWIBREG in 2019 was, on average, 5.6 (moderate quality).
SWIBREG records patient accessibility to IBD centres. These data are patient-reported and graded as very poor, rather poor, rather good, and very good. The majority of patients report very good (65% in 2019) or rather good (30% in 2019) accessibility to healthcare.
The register also enables users to examine the completeness of a number of variables: diagnosis (generally very high), disease extent (moderately high) (), having a first-degree relative with IBD, and surgical resections (both of low or moderately low completeness).
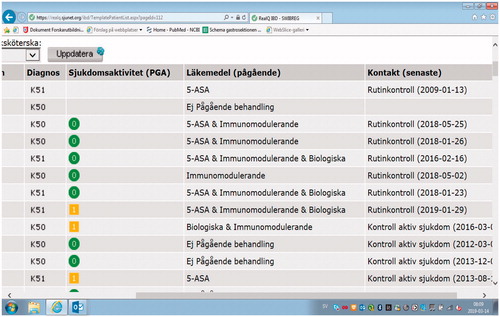
Figure 6. SWIBREG contains information on diagnosis, disease activity, ongoing medical treatment, and date of last check-up.
Quality assurance is also examined for variables regarded to be more advanced, such as weight, PGA, SHS, haemoglobin levels, faecal calprotectin, and disease activity indices (Walmsley, Mayo or HBI in adults, PUCAI or short PCDAI in children) [Citation43,Citation44].
Age-specific follow-up
Some Swedish QRs have decided to focus on only adult populations. This strategy contrasts with SWIBREG’s approach to following patients from birth to old age.
A recent paper by Everhov et al. [Citation5] reports that the elderly (≥60 years) patients with IBD have less IBD-specific outpatient healthcare but more IBD-related hospitalisations and overall healthcare use than younger IBD patients. Compared to patients with paediatric or adult-onset IBD, elderly patients use fewer biologics and immunomodulators but more systemic corticosteroids [Citation5]. Lesser use of biologics may have several explanations, including risk of polypharmacy and an increased risk of side effects. While we urge caution when interpreting the differences in drug use in relation to age, SWIBREG serves as an important instrument to follow-up elderly patients with IBD. There are currently 15,756 elderly (≥60 years) patients with IBD in the register. The sex distribution in SWIBREG conforms to international findings showing that about 50% of patients are women [Citation10].
Specific aspects of children with IBD
The incidence of paediatric CD is increasing worldwide, with Sweden being a high-prevalence country [Citation1]. The goal of both paediatric CD and UC treatment is to induce and maintain clinical remission and mucosal healing. Childhood IBD, which occurs nearly equally in boys and girls, is characterised by severe abdominal pain, diarrhoea, fever, weight loss, often growth retardation, and sometimes delayed puberty [Citation45].
IBD with an onset in childhood is often more extensive [Citation46] and severe [Citation47–49]. Children with IBD typically undergo more immunomodulatory therapy [Citation5,Citation50] and seem to be at high risk of malignancy [Citation3]. SWIBREG can, therefore, serve as an important tool for transition [Citation51] between paediatric and adult care. As of 2019, SWIBREG contains data on 1461 children (0–19 years) with IBD. The number of patients with childhood onset is, however, larger (some of these individuals have as of today turned 18 years old). In recent years, the structure of SWIBREG has been adjusted to accommodate a larger number of paediatric IBD patients. Accordingly, height and weight data are now recorded in SWIBREG because, in children, growth is an important marker of health and disease (growth data are available in 566 patients since 2019). The paediatric modification of the Montreal classification for adults is the Paris Classification [Citation23].
Currently, there is no known cure for CD. Treatment for the condition traditionally focuses on remission of symptom to improve the QOL, but inflammatory control is now being recognised as an important goal to change the disease course and risk of complications. To induce remission of CD, exclusive enteral nutrition (EEN) therapy is the recommended first-line treatment in children [Citation52]. EEN is a non-pharmacological treatment option for induction of clinical remission and mucosal healing in CD [Citation53]. In EEN, oral standard enteral nutrition products are used as the only source of nutrition for 6–8 weeks. EEN is highly effective in newly diagnosed paediatric CD [Citation52].
SWIBREG has a special module that allows for the recording of enteral nutrition.
For maintenance of CD remission, immunomodulating drugs (e.g., thiopurines) are recommended.
SWIBREG has developed into a tool for paediatric IBD through the inclusion of the PUCAI for childhood UC and the short PCDAI (Paediatric Crohn’s Disease Activity Index) for CD. We also use the HBI for a paediatric CD to facilitate the transition into adult IBD care. The reason for using the short PCDAI rather than the full PCDAI is that the short version does not require blood testing and rectal examination and, therefore, minimises pain and discomfort in children.
Clinical use, data input, and user value
For the purpose of this paper, we sent out a web questionnaire to SWIBREG users in healthcare in spring 2019. Of 141 respondents and users, 79 (56.0%) were physicians with nurses constituting 40% (n = 56). Six users had other professions.
Excluding two individuals who claimed filling out the register in ‘0 min’, the median time to fill out relevant SWIBREG data at patient visit was 5 min (average 5.6 min) with the range being 0.5–20 min (one individual reported 20 min, no other individual reported >15 min; n = 118).
Of IBD patients seen by healthcare in 2019, it was estimated that some 62% had their data entered at the time of the visit. Some 10 users (7%, n based on 134) reported never filling out any SWIBREG data for patients while 46 (34%) filled out data for at least 90% of all patients. Since one IBD unit may be represented by several users, we urge caution when interpreting these data.
Of the 129 healthcare professionals responding to our question on the value of SWIBREG, 44 (34.1%) said that the healthcare benefited from SWIBREG, 50 individuals (38.9%) that the time requested to fill out the data equated the clinical benefits of SWIBREG, while 35 (27.1) thought that the time needed to fill out SWIBREG was disproportionate.
When users were asked about the most important feature of SWIBREG, facilitating the contact and follow-up of the patients was ranked first. Other areas where SWIBREG was regarded as particularly useful were to follow-up specific groups of patients including those on biologics, but also that it was thought to improve patient participation. A few individuals indicated comparisons between different clinical units and research as important features of SWIBREG.
Extraction of data
Extraction of data is of key importance to a register that seeks to have an impact on clinical management. SWIBREG allows individual clinics to download their own data.
Improvement care
It is clear from SWIBREG data (geographical differences) that there is room for improvement on a national level, but we believe that IBD healthcare may also differ within sites regarding access to outpatient care, surgery, and the interval between patient visits. To fully penetrate differences, data from our QR should ideally be linked to national databases (such as the longitudinal integrated database for health insurance and labour market studies (LISA)) [Citation54] for information on income, education, and sex, three parameters that are often linked to healthcare use.
A prerequisite for an effective collaboration between patients, families, and healthcare professionals is a well-functioning communication. Together with Telia (a Swedish telecommunication company) and 1177 (a government-run national health care portal), SWIBREG has launched a patient-administered application to retrieve patient-reported data. Such communication seeks to prevent relapse because early signals of deterioration in the patient’s health can be met with intensified treatment.
A QR contains copious amounts of data but data alone will not be useful and improve care. Evidence-based medicine should be co-produced by staff and patients, with a joint commitment of improving care continuously and in a sustainable way [Citation55]. In SWIBREG, we have identified three interrelated goals: (a) better outcomes, (b) better systems performance, and (c) better professional development [Citation56]. These goals may be reached as a QR slowly transforms into registry-based improvement networks [Citation36].
Inspired by the Improve Care Now Learning Network [Citation57,Citation58], seven local outpatient clinics, each with patients on the teams (out of 52 units participating in SWIBREG) have identified outcomes that matter. The main goal is to increase the proportion of patients in clinical remission as indicated by PGA.
A learning network is based on the joint commitment of patients, healthcare practitioners and researchers, all with a mean to improve the patient’s outcome. This joint effort is offered by focussing on outcomes, building communities, using data effectively, and employing multiple learning systems as presented by Lannon et al. [Citation36].
Research based on SWIBREG
The primary aim of SWIBREG is to serve as a tool for quality improvement of Swedish IBD care. However, recorded data can also be used for research. Several ongoing studies have centred around drug effectiveness, with a focus on newer targeted therapies [Citation29,Citation59]. As already mentioned, these studies were preceded by a validation study of IBD diagnoses [Citation17].
SWIBREG aims to involve patients and their families in the IBD research agenda. Together with the Swedish Patient Organisation for gastrointestinal disease, the QR carried out a web questionnaire in 2016 with IBD patients and their families. Topics prioritised for research by the patient community are listed in 112 respondents).
Table 1. Research priorities indicated by the IBD patient community.
Discussion
SWIBREG, launched in 2005, is Sweden’s QR for IBD. It already covers more than 46,000 individuals of varying ages. This QR has become an instrument for benchmarking between different hospitals and regions in Sweden, and we believe it can help homogenise IBD care in Sweden, just as the IBD Benchmarking tool of the IBD Standards has done in the UK [Citation60].
SWIBREG offers access to real-world data on novel therapies [Citation29,Citation59]. The integrated real-time decision support system, IBD-care, has also become a key-tool in daily clinical practice for many healthcare providers in Sweden, and the recently launched e-health based communication system represents a facilitating step towards patient empowerment at a national level.
Why SWIBREG was started
While the Swedish NPR contains a large amount of data on diseases, including IBD [Citation17], granular data on disease activity, anatomic distribution of inflammation, infusion drugs, and QoL are missing or registered with few details [Citation14]. Nor can NPR data be used in a clinical decision support system. In contrast, SWIBREG data are presented in a graphical format to help the patient and his/her physician to make optimal decisions. The idea of providing the health care provider with a system that can guide clinical decision-making represents a cornerstone of SWIBREG and was the main rational for integrating the decision support system IBD-care in year 2012. Importantly, users also ranked ‘facilitating the contact and follow-up of the patients’ as the most important feature of the QR.
Differences compared to other databases
While we are aware of several descriptions of IBD databases, a few other QRs are accompanied by decision support systems, and do not typically include data on user experience. Hence, we are unable to compare our findings with that of IBD professionals in other countries. However, from a patient view, it is comforting that communication and follow-up with patients rank high, since earlier research demonstrates the importance of communication between healthcare and patient [Citation61]. Facilitating communication might also help align treatment goals of patients and physicians, as well as increase the focus on QoL [Citation62]. Our data on EQ5D-5L allow for comparisons of QoL with other diagnoses, also outside the gastrointestinal tract.
SWIBREG offers highly granular data, including data on the use of infusions with biologics. However, it should be noted that SWIBREG is not limited to patients on biologics but aim to cover a national non-selected IBD population. The true population-based nature of our QR is particularly important in studies on prognosis, where disease severity and course of disease may differ between those with mild and severe disease (and with and without biologics [Citation63]). SWIBREG includes patients across a variety of care, including university hospitals, regional hospitals, district hospital, and private IBD clinics, reflecting the average patient thereby greatly increasing the external validity of its data. This contrasts with e.g., Swiss-IBD that is limited to university clinics, with a consequent risk of selection bias and skewed prognosis (http://www.ibdcohort.ch/index.php/home-21.html, accessed August 19, 2019) [Citation64]. SWIBREG has already become an important source for nationwide registry-based research [Citation65,Citation66].
SWIBREG is run by physicians, nurses, and representatives from relevant patient organisations, and was initiated by representatives of Swedish healthcare. This contrasts with some IBD registers that were coordinated by the pharmaceutical industry (for instance the TREAT registry (https://clinicaltrials.gov/ct2/show/NCT00553176, accessed August 19, 2019) [Citation67] sponsored by Janssen). The scientific independence of SWIBREG minimises the risk of publication bias when effects and adverse outcomes of drugs are studied. A paper from neighbouring Denmark found that routine database registration of therapy substantially increased the reporting of adverse events [Citation68]. As opposed to some registers (e.g., the Long-Term Registry of Humira® (Adalimumab) sponsored by Abbott (https://clinicaltrials.gov/ct2/show/NCT01848561, accessed August 19, 2019) and the Cimzia ® Crohn's Disease Post-Marketing Registry (SECURE, https://clinicaltrials.gov/ct2/show/NCT00844285, accessed August 19, 2019) sponsored by UCB Pharma), SWIBREG was not initiated to examine targeted therapies and to fulfil strict criteria for phase 4 studies set up by government agencies (e.g., EMA and FDA), but to allow clinicians and researchers to examine any treatment given to IBD patients.
Challenges for the future
As part of this review, we performed a web questionnaire to collect data from SWIBREG users. The median time to fill out relevant SWIBREG data at the patient visit was 5 min (average 5.6 min). While the majority of healthcare users thought the time spent reasonable or benefited healthcare we acknowledge that one in four users reported that the time needed to fill out SWIBREG was disproportionate. Similar concerns have been highlighted by for instance the Rotherham IBD database user group [Citation69], that also found that they had underestimated the time needed to fill out and maintain an IBD register, and that this limited real-time use of the database. Time restraints may have been one reason for the cessation of the British Paediatric IBD Register that, starting in the late 1990s ended a couple of years later [Citation70,Citation71]. Swift completion of the SWIBREG web form has been identified as a key concern, and we are currently undertaking a number of efforts to reduce time expenditure, especially by eliminating any double entry of data.
Apart from a recent patient chart validation (showing that SWIBREG has high specificity), there are little data on the completeness, coverage, or validity of the different variables in the register. One way of better understanding the quality of SWIBREG is to carry out comparisons with the NPR [Citation18]. Also, other databases have used comparisons with other data sources for external validation [Citation67]. Compared to the MedStat MarketScan insurance claims database, patients in the TREAT database had similar rates of CD-related hospitalisations but a higher risk of surgery, indicating that TREAT patients may represent a more severe subset of patients (due to increased need of surgery) than average patients in insurance databases [Citation67].
SWIBREG records information on medications, including biological treatment, endoscopies, surgery, faecal calprotectin, and other laboratory measurements. It also records information on smoking, disease activity, QoL, and PROMs. Among the weaknesses of SWIBREG is the low coverage on some of these parameters. However, the percentage of SWIBREG patients with recorded smoking data (46%) was identical to that of the UK IBD database (by the Rotherham database user group: data available in 5237/11,432 = 46%) [Citation69].
Another weakness is the varying coverages between centres and geographical differences in IBD management. Over time, coverage has improved in Swedish IBD centres and today four hospitals have 100% coverage and 12 have more than a 90% coverage using the NPR as the gold standard.
In conclusion, the Swedish IBD QR SWIBREG benefits patients with IBD and offers an ideal opportunity for healthcare personnel and researchers to examine disease phenotype and activity, PROMs/PREMs, and hospital-administered drugs in patients with IBD.
Author contributions
Guarantor of the article: PM
Specific author contributions: JFL conceived and designed the study with input from the other authors. JFL also wrote the first draft of the paper and supervised the project. PM, JFL and MO analysed the data. All authors interpreted the data and contributed to the writing of the manuscript. All authors revised and approved the final version.
All authors approved the final version of the manuscript.
Transparency
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Licence for publication
The corresponding author has the right to grant on behalf of all authors and does grant on behalf of all authors, a worldwide licence to the Publishers and its licensees in perpetuity, in all forms, formats and media (whether known now or created in the future), to (i) publish, reproduce, distribute, display, and store the Contribution; (ii) translate the Contribution into other languages, create adaptations, reprints, include within collections and create summaries, extracts and/or, abstracts of the Contribution; (iii) create any other derivative work(s) based on the Contribution; (iv) to exploit all subsidiary rights in the Contribution; (v) the inclusion of electronic links from the Contribution to third party material wherever it may be located; and (vi) licence any third party to do any or all of the above.
| Abbreviations | ||
| CD | = | Crohn’s disease |
| GI | = | gastrointestinal |
| IBD | = | inflammatory bowel disease |
| IBD-U | = | IBD unclassified |
| NPR | = | National Patient Register |
| PGA | = | Physician Global Assessment |
| PREM | = | patient-reported experience measure |
| PROM | = | patient-reported outcome measure |
| QoL | = | quality of life |
| QR | = | quality register |
| SHS | = | Short Health Scale |
| SWIBREG | = | Swedish Inflammatory Bowel Disease Register |
| UC | = | ulcerative colitis |
Disclosure statement
Dr Ludvigsson coordinates a study on behalf of the Swedish IBD quality register (SWIBREG). None of the other authors have declared any conflicts of interest with regards to this manuscript.
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf
Data sharing
Other researchers can apply for our data through the steering group of SWIBREG (see address to corresponding author Myrelid).
Additional information
Funding
References
- Ludvigsson JF, Busch K, Olen O, et al. Prevalence of paediatric inflammatory bowel disease in Sweden: a nationwide population-based register study. BMC Gastroenterol. 2017;17(1):23.
- Olen O, Askling J, Sachs MC, et al. Increased mortality of patients with childhood-onset inflammatory bowel diseases, compared with the general population. Gastroenterology. 2019;156(3):614–622.
- Olen O, Askling J, Sachs MC, et al. Childhood onset inflammatory bowel disease and risk of cancer: a Swedish nationwide cohort study 1964–2014. BMJ. 2017;358:j3951.
- Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504–1517.
- Everhov AH, Halfvarson J, Myrelid P, et al. Incidence and treatment of patients diagnosed with inflammatory bowel diseases at 60 years or older in Sweden. Gastroenterology. 2018;154(3):518–528 e15.
- Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–2778.
- Parkes GC, Whelan K, Lindsay JO. Smoking in inflammatory bowel disease: impact on disease course and insights into the aetiology of its effect. J Crohns Colitis. 2014;8(8):717–725.
- Imhann F, Vich Vila A, Bonder MJ, et al. Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease. Gut. 2018;67(1):108–119.
- Ortqvist AK, Lundholm C, Halfvarson J, et al. Fetal and early life antibiotics exposure and very early onset inflammatory bowel disease: a population-based study. Gut. 2019;68(2):218–225.
- Shah SC, Khalili H, Gower-Rousseau C, et al. Sex-based differences in incidence of inflammatory bowel diseases-pooled analysis of population-based studies from western countries. Gastroenterology. 2018;155(4):1079–1089 e3.
- Ellinghaus D, Bethune J, Petersen BS, et al. The genetics of Crohn's disease and ulcerative colitis–status quo and beyond. Scand J Gastroenterol. 2015;50(1):13–23.
- Silverman SL. From randomized controlled trials to observational studies. Am J Med. 2009;122(2):114–120.
- Swedish Patient Data Law (Patientdatalagen). 355. Sect. 7 2008.
- Emilsson L, Lindahl B, Koster M, et al. Review of 103 Swedish Healthcare Quality Registries. J Intern Med. 2015;277(1):94–136.
- Munkholm P. Crohn's disease-occurrence, course and prognosis. An epidemiologic cohort-study. Dan Med Bull. 1997;44(3):287–302.
- Langholz E. Ulcerative colitis. An epidemiological study based on a regional inception cohort, with special reference to disease course and prognosis. Dan Med Bull. 1999;46(5):400–415.
- Jakobsson GL, Sternegard E, Olen O, et al. Validating inflammatory bowel disease (IBD) in the Swedish National Patient Register and the Swedish Quality Register for IBD (SWIBREG). Scand J Gastroenterol. 2017;52(2):216–221.
- Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11(1):450.
- Ludvigsson JF, Haberg SE, Knudsen GP, et al. Ethical aspects of registry-based research in the Nordic countries. Clin Epidemiol. 2015;7:491–508.
- Satsangi J, Silverberg MS, Vermeire S, et al. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55(6):749–753.
- Magro F, Gionchetti P, Eliakim R, et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and Ileo-anal Pouch disorders. J Crohns Colitis. 2017;11(6):649–670.
- Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, et al. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659–667.
- Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011;17(6):1314–1321.
- Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317(26):1625–1629.
- Froslie KF, Jahnsen J, Moum BA, et al. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007;133(2):412–422.
- Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register – opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–735.
- Olen O, Askling J, Sachs MC, et al. Mortality in adult-onset and elderly-onset IBD: a nationwide register-based cohort study 1964–2014. Gut. 2019. DOI:10.1136/gutjnl-2018-317572
- Targan SR, Hanauer SB, van Deventer SJ, et al. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn's disease. Crohn's Disease cA2 Study Group. N Engl J Med. 1997;337(15):1029–1035.
- Eriksson C, Marsal J, Bergemalm D, et al. Long-term effectiveness of vedolizumab in inflammatory bowel disease: a national study based on the Swedish National Quality Registry for Inflammatory Bowel Disease (SWIBREG). Scand J Gastroenterol. 2017;52(6–7):722–729.
- Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn's disease. N Engl J Med. 2013;369(8):711–721.
- Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369(8):699–710.
- Umanskiy K, Fichera A. Health related quality of life in inflammatory bowel disease: the impact of surgical therapy. World J Gastroenterol. 2010;16(40):5024–5034.
- Gionchetti P, Dignass A, Danese S, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 2: surgical management and special situations. J Crohns Colitis. 2017;11(2):135–149.
- Mark-Christensen A, Erichsen R, Brandsborg S, et al. Pouch failures following ileal pouch-anal anastomosis for ulcerative colitis. Colorectal Dis. 2018;20(1):44–52.
- Nordenvall C, Myrelid P, Ekbom A, et al. Probability, rate and timing of reconstructive surgery following colectomy for inflammatory bowel disease in Sweden: a population-based cohort study. Colorectal Dis. 2015;17(10):882.
- Cnattingius S, Ericson A, Gunnarskog J, et al. A quality study of a medical birth registry. Scand J Soc Med. 1990;18(2):143–148.
- Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205–217.
- Jaghult S, Saboonchi F, Johansson UB, et al. Identifying predictors of low health-related quality of life among patients with inflammatory bowel disease: comparison between Crohn's disease and ulcerative colitis with disease duration. J Clin Nurs. 2011;20(11–12):1578–1587.
- Stjernman H, Granno C, Jarnerot G, et al. Short health scale: a valid, reliable, and responsive instrument for subjective health assessment in Crohn's disease. Inflamm Bowel Dis. 2008;14(1):47–52.
- McDermott E, Keegan D, Byrne K, et al. The Short Health Scale: a valid and reliable measure of health related quality of life in English speaking inflammatory bowel disease patients. J Crohns Colitis. 2013;7(8):616–621.
- Hjortswang H, Jarnerot G, Curman B, et al. The Short Health Scale: a valid measure of subjective health in ulcerative colitis. Scand J Gastroenterol. 2006;41(10):1196–1203.
- Abdovic S, Pavic AM, Milosevic M, et al. Short health scale: a valid, reliable, and responsive measure of health-related quality of life in children with inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(4):818–823.
- Walmsley RS, Ayres RC, Pounder RE, et al. A simple clinical colitis activity index. Gut. 1998;43(1):29–32.
- Harvey RF, Bradshaw MJ. Measuring Crohn's disease activity. Lancet. 1980;1(8178):1134–1135.
- Mason A, Malik S, McMillan M, et al. A prospective longitudinal study of growth and pubertal progress in adolescents with inflammatory bowel disease. Horm Res Paediatr. 2014;83(1):45–54.
- Malmborg P, Grahnquist L, Idestrom M, et al. Presentation and progression of childhood-onset inflammatory bowel disease in Northern Stockholm County. Inflamm Bowel Dis. 2015;21(5):1098–1108.
- Van Limbergen J, Russell RK, Drummond HE, et al. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008;135(4):1114–1122.
- Vernier-Massouille G, Balde M, Salleron J, et al. Natural history of pediatric Crohn's disease: a population-based cohort study. Gastroenterology. 2008;135(4):1106–1113.
- Gower-Rousseau C, Dauchet L, Vernier-Massouille G, et al. The natural history of pediatric ulcerative colitis: a population-based cohort study. Am J Gastroenterol. 2009;104(8):2080–2088.
- Pigneur B, Seksik P, Viola S, et al. Natural history of Crohn's disease: comparison between childhood- and adult-onset disease. Inflamm Bowel Dis. 2010;16(6):953–961.
- Sebastian S, Jenkins H, McCartney S, et al. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: differing perceptions from a survey of adult and paediatric gastroenterologists. J Crohns Colitis. 2012;6(8):830–844.
- Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn's disease. J Crohns Colitis. 2014;8(10):1179–1207.
- Zachos M, Tondeur M, Griffiths AM. Enteral nutritional therapy for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2007;(1):CD000542.
- Ludvigsson JF, Svedberg P, Olen O, et al. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;34(4):423–437.
- Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25(7):509–517.
- Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007;16(1):2–3.
- Ovretveit J, Keller C, Hvitfeldt Forsberg H, et al. Continuous innovation: developing and using a clinical database with new technology for patient-centred care – the case of the Swedish quality register for arthritis. Int J Qual Health Care. 2013;25(2):118–124.
- Rejler M. Nätverk förbättrar vården för patienter med kroniska sjukdomar; 2014. Hälsohögskolan, Högskolan i Jönköping, HHJ. Kvalitetsförbättring och ledarskap inom hälsa och välfärd Stockholm: Sweden, Europe. [cited 2019 Aug 29]. Available from: http://hj.diva-portal.org/smash/get/diva2:781567/FULLTEXT01.pdf
- Rundquist S, Eriksson C, Nilsson L, et al. Clinical effectiveness of golimumab in Crohn's disease: an observational study based on the Swedish National Quality Registry for Inflammatory Bowel Disease (SWIBREG). Scand J Gastroenterol. 2018;53(10–11):1257–1263.
- IBD standards: Benchmarking tool. [cited 2019 Aug 12]. Available from: https://ibduk.org/ibd-benchmarking-tool
- Maly RC, Liu Y, Liang LJ, et al. Quality of life over 5 years after a breast cancer diagnosis among low-income women: effects of race/ethnicity and patient-physician communication. Cancer. 2015;121(6):916–926.
- Rubin DT, Dubinsky MC, Martino S, et al. Communication between physicians and patients with ulcerative colitis: reflections and insights from a qualitative study of in-office patient-physician visits. Inflamm Bowel Dis. 2017;23(4):494–501.
- Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010;362(15):1383–1395.
- Zankel E, Rogler G, Andus T, et al. Crohn's disease patient characteristics in a tertiary referral center: comparison with patients from a population-based cohort. Eur J Gastroenterol Hepatol. 2005;17(4):395–401.
- Everhov AH, Khalili H, Askling J, et al. Work loss before and after diagnosis of Crohn's disease. Inflamm Bowel Dis. 2019;25(7):1237–1247.
- Everhov AH, Khalili H, Askling J, et al. Sick leave and disability pension in prevalent patients with Crohn's disease. J Crohns Colitis. 2018;12(12):1418–1428.
- Lichtenstein GR. The TREAT Registry: evolution of knowledge from 1999 to 2017: lessons learned. Clin Gastroenterol Hepatol. 2017;15(9):1319–1321.
- Hetland ML, Unkerskov J, Ravn T, et al. Routine database registration of biological therapy increases the reporting of adverse events twentyfold in clinical practice. First results from the Danish Database (DANBIO). Scand J Rheumatol. 2005;34(1):40–44.
- Bardhan KD, Simmonds N, Royston C, et al. A United Kingdom inflammatory bowel disease database: making the effort worthwhile. J Crohns Colitis. 2010;4(4):405–412.
- Sawczenko A, Sandhu BK, Logan RF, et al. Prospective survey of childhood inflammatory bowel disease in the British Isles. Lancet. 2001;357(9262):1093–1094.
- Taylor L, Casson D, Platt MJ. Issues and experience around the Paediatric Register of Inflammatory Bowel Disease. Arch Dis Child. 2003;88(10):891–893.