Abstract
Aim: Narrative medicine has been promoted as an innovative and effective means of stimulating medical students’ professional development by teaching them to approach their patients’ experiences of illness with more understanding and compassion. This systematic literature review aims to answer the following question: what evidence of effect is available in the literature about models for teaching narrative medicine?
Methods: We conducted a narrative review of 36 articles and used the Best Evidence in Medical Education (BEME) Global Scale and Kirkpatrick Scale for strength and importance of evidence to categorize reported assessment strategies and to evaluate the effectiveness of their narrative medicine programs.
Results: We found evidence that narrative medicine is an effective pedagogic tool with a clear and replicable structure and methodology. We also determined that a positive impact could be measured when pertaining to participation and modification of attitudes, knowledge, and skills. However, unequivocal evidence of the effect of narrative medicine on students’ behavior or ongoing interaction with colleagues and patients is still lacking.
Conclusion: While many recent publications describe the goals and virtues of a narrative-based approach, more research is needed to determine whether or not there is an ideological consensus undergirding this approach. In addition, it is still unclear whether the long-term impact of narrative medicine classroom interventions are felt by patients, or whether such interventions positively impact patient care.
Introduction
With the increasingly prominent role that technology and big data play in clinical interactions, the risk is that less attention will be paid to the singularity and significance of each patient’s illness narrative. It is not unconceivable that the rise of digital medicine may correspond with the emergence of two sorts of competing narratives: the digital narratives collected via digital technologies and the experiential, personal narratives of the patients using such technologies.
Narrative medicine, or narrative-based medicine, constitutes “an approach to medicine that employs narrative skills to augment scientific understandings of illness” (Lewis Citation2011) and can thus be seen as one means of preventing this narrative schism. Those who teach and practice narrative-based medicine claim that it is not intended to be an alternative to modern, technologically enhanced, medicine. Rather, it is seen as a means of revealing to medical professionals that evidence-based practices can and should be paired with the personal evidence that emerges in a dialogic clinical encounter between a doctor and patient (Holmgren Citation2011; Chin-Yee Citation2018). Proponents claim that better attention to and appreciation of narratives in the clinical setting can help doctors bridge the gap between their mediopathological knowledge and the experiential knowledge contained in their patients’ stories (Greenhalgh Citation1999; Greenhalgh and Hurwitz Citation1999; Launer 1999; Hurwitz Citation2000).
Narrative medicine educational interventions thus serve as an important means of preparing medical students’ to engage in the shared-decision making process with their patients (Charon Citation2008; Charon and DasGupta Citation2011) by increasing their “narrative competence” (Charon Citation2007). Such interventions aim to help students hone their listening and observation skills, stimulate their empathic abilities, and increase their capacity for reflection and perspective-taking (Marchalik Citation2017). In addition, narrative medicine’s supporters contend that it is not only geared toward the stimulation of a more interactive and empathetic doctor-patient engagement; the dividends of a concerted training in self-reflective practices combined with an exposure to the arts—be it film, music, paintings, sculpture, or literature—will supposedly lead to a better sense of self as well as better and more meaningful relationships with one’s colleagues and the public (Charon Citation2001; Citation2006; Yu Citation2017).
A steady output of studies continues to valorize the use of narrative-based practices in the training of health care professionals. Recent systematic reviews have attempted to synthesize and analyze the impact of these studies. Haidet et al.’s (Citation2016) systematic review of arts-based courses in medical education, which included studies reporting on Columbia’s narrative medicine program, found that such courses could be linked to increased empathy, communication, observation, and ethical reasoning skills in medical students. Barber and Moreno-Leguizamon’s (Citation2017) literature review of narrative medicine education included only nine studies, but nevertheless found evidence of four emergent themes in these publications: a stress on communication skills, in particular increased empathy; personal and professional growth; pleasure, or enjoyment on the part of participating students; and a noticeable educational structure of small group settings led by skilled facilitators. While the authors acknowledge the value of these reported results, they conclude that “there is insufficient large-scale data to establish a higher clinical value” (p. 202) of narrative medicine education. Wieżel et al.’s (Citation2017) study of narrative medicine in medical school education was more expansive in its scope, in this case reviewing 31 relevant publications. Like Barber, the authors acknowledge the value and potential benefits of narrative medicine interventions on students’ reflective, empathic, interpersonal, and intersocial capabilities, yet they conclude that “based on the collected data, there is no structured model of NM [narrative medicine] approach in the medical education” (p. 564).
This study aims to fill a persistent knowledge gap by offering a comprehensive answer to the question: what evidence of effect is available in the literature about models for teaching narrative medicine?
Methods
Our goal is to ascertain whether or not the pedagogic strategies proposed in the theoretical publications about narrative-based medicine were systematically applied in health education settings. For this reason, our health education systematic review (Gordon Citation2018) will focus on articles that report on specific narrative medicine interventions in medical education or in the continuing professional development of medical practitioners, not on articles that describe the use of narrative medicine in clinical settings or in non-health education settings. This review will attempt to answer the following three sub-questions: first, is there evidence of a structured model for narrative-based medicine in health education, and if so, is it consistently applied? Second, is there evidence that narrative-based classroom interventions result in measurable outcomes? Finally, what is the quality and nature of the reported outcomes?
Literature search
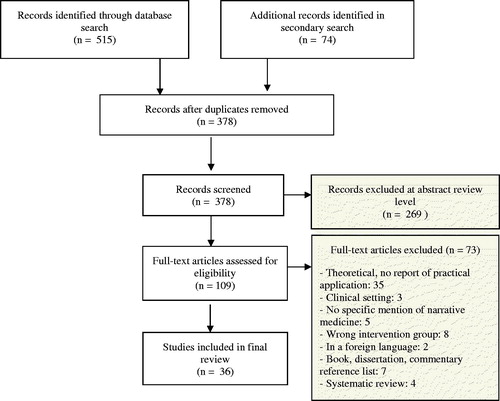
Our systematic review was executed in two phases: first, we searched electronic databases; second, we ran an iterative search targeting key authors and articles related to narrative medicine. Articles in the first phase were obtained from the following electronic databases: PubMed, Medline, Psychinfo, EBSCO Academic Search Premier, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). A list of the separate search strings can be found in the Supplementary Appendix; as a means of retrieving the most relevant sources, we searched for articles that included “narrative medicine” or “narrative-based medicine” in the title, abstract, or keywords. We also limited our search to articles published from 2000 onwards as the first theoretical publications describing narrative medicine or narrative-based medicine as a concept and potential classroom intervention were published in 1999. Once we had reached consensus about the search terms, one author (M.M.) ran an initial search on November 6, 2017. This search was repeated on May 31, 2018.
For the second phase, we ran a separate search on PubMed by author, in this case for the co-founders of Columbia University’s Narrative Medicine Program—Rita Charon, Sayantani DasGupta Craig Irvine, and Maura Spiegel—in order to identify key articles about narrative medicine classroom interventions. We then examined the reference lists of these articles for further relevant sources. We also examined the works cited in systematic reviews on narrative medicine, empathy, and the arts in medical education to identify any additional articles that could be relevant to our research questions (Kuper Citation2006; Batt-Rawden et al. Citation2013; Cowen Citation2016; Barber and Moreno-Leguizamon Citation2017; Wieżel et al. Citation2017). After removing duplicates, 378 articles remained.
Article selection
Two authors (M.M and G.v.T.) independently identified relevant articles for full-text review in Covidence by scanning the titles and abstracts on the basis of the following eligibility criteria.
Inclusion criteria: publications that describe narrative medicine curricula, courses, seminars, or teaching practices in a medical or paramedical classroom setting at the undergraduate, graduate, or postgraduate level; studies describing a faculty development professional development intervention for health care providers; publications that attempt to test the impact of narrative medicine as a pedagogic tool with qualitative and/or quantitative assessment.
Exclusion criteria: publications that report on the use of narrative medicine in a clinical setting; publications that theorize about narrative medicine but do not describe its use in a specific classroom setting; publications that describe the use of narrative medicine in a non-medical setting (for example, veterinary school); publications that do not explicitly mention and use narrative medicine as a pedagogic tool; non-English publications; systematic literature reviews.
After meeting to compare inclusion lists and resolving any conflicts, one researcher (M.M.) conducted a full-text analysis for eligibility. In total, 36 studies reporting on a narrative medicine classroom intervention were included in the final analysis. contains a flow diagram of the search process.
Data extraction
One author (M.M.) reviewed the full texts and extracted the following general information: authors, year of publication, site of classroom intervention, type of study (report of intervention, qualitative and/or quantitative assessment component), the narrative medicine course level and field, type of course (elective, required, faculty development), the duration of course, and the number of participants, if mentioned. In addition, the extraction recorded more detailed aspects of the reported narrative medicine course content. This included: specific art forms or theoretical texts used in the course, specific writing assignments as well as formal and informal assessment tools used in the course itself (for example, peer feedback or writing workshop sessions with a physician-writer and expert). Finally, the extraction also recorded the methods, objectives, and outcomes reported in the studies that included a qualitative and/or quantitative assessment of a pedagogic intervention.
Evidence grading
Studies that attempted to assess the outcomes of a narrative medicine classroom intervention were rated using the Best Evidence in Medical Education (BEME) Global Rating Scale, which includes both a Kirkpatrick-based outcomes scale and a strength of evidence scale (Hammick et al. Citation2010). Originally conceived as a means of assessing training programs in business organizations (Kirkpatrick Citation1959, Citation1976, Citation1996), the Kirkpatrick model has become a standard tool for gauging the effectiveness of programs in higher education (Praslova Citation2010) including medical education (Issenberg et al. Citation2005; Littlewood et al. Citation2005; Steinert et al. Citation2006; Colthart et al. Citation2008; Tochel et al. Citation2009; Sullivan Citation2011). The BEME Global Scale can be found in .
Table 1. Best Evidence Medical Education (BEME) coding scheme for strength of evidence and Kirkpatrick-based outcomes.
After completing the data extraction, one author (M.M.) coded the included articles using the BEME Global Scale. Once this step was completed, a second author (G.v.T.) completed an independent grading of 5 randomly selected articles. The two authors then met to compare their scores and resolve disagreements. Supplementary Table 2 provides key information from the data extraction as well as the BEME strength of evidence and outcome scores.
Results
Evidence of structured model for narrative-based medicine interventions
Theoretical publications about narrative medicine in health education typically describe a pedagogic strategy consisting of three basic steps. The first step involves a reflective engagement with a patient narrative, literary text, film fragment, art work, or piece of music. At Columbia’s Narrative Medicine Program, this step includes a close reading—or critical analysis—of the art form and is considered the signature method in their narrative medicine classrooms (Charon, DasGupta, et al. Citation2016, p. 181). The insights gained during this engagement are reinforced in the second step of the pedagogic strategy by means of a corresponding writing assignment or personal reflection. The encounter is further enriched in the third step, which consists of sharing and discussing these small acts of self-reflection (Balmer and Richards Citation2012, p. 2). In other words, a narrative medicine classroom intervention entails encountering and/or analyzing an art form or narrative, reflecting upon this encounter, and sharing one’s discoveries with others in carefully monitored and supportive environment (Charon, DasGupta, et al. Citation2016).
Of the studies in this review that reported on their use of narrative medicine as a pedagogic tool (N = 36), evidence of this three-step process of (close) reading-reflecting-responding could be found in the majority of the articles (N = 22). A minority of courses only included reflective writing and discussion (N = 12). A very small minority did not include written reflection (N = 2).
Evidence of measurable outcomes
In this review, 23 studies assessed the impact of their narrative medicine classroom interventions; a brief summary of the findings categorized according to the Kirkpatrick model can be found in . A detailed description of the measures and outcomes of these studies can be found in the Supplementary Appendix.
Table 2. Data extraction from included articles (N = 36).
Level one: participation
The majority of the studies included level one or two assessments. Studies that included level one outcome measures (N = 14) overwhelmingly relied on surveys or feedback forms as outcome measures but reported positive student reactions to the narrative medicine interventions themselves (Winkel Citation2010; Ross Citation2014) and positive effects, such as a sense of gratitude, hope, satisfaction, or pleasure (DasGupta and Charon Citation2004; Feigelson and Muller Citation2005; Garrison Citation2011; Chretien Citation2015).
Level two: modification of attitudes, perceptions, knowledge, or skills
Studies that reported on modification of participants’ attitudes or perceptions (level 2a; N = 16) found, for example, increased identification with their peers and the broader professional community (Feigelson and Muller Citation2005; Balmer and Richards Citation2012; Al-Imari et al. Citation2016), more satisfaction with their work and sense of wellness (Feigelson and Muller Citation2005; Graham Citation2009), or a better awareness of cultural diversity (DasGupta et al. Citation2006). Chretien’s (Citation2015) assessment study of a narrative medicine patient storytelling course for third-year medical clerkship students provides an illustrative example. During the course, students had to interview patients, write up their interview as a narrative, and share this written work with their interviewees. Focus groups and interviews with both students and participating patients were conducted after the course was completed. Students reported that the exercise helped them discover that patients are more than their disease, made them more open to taking the opportunity to slow down and listen, and made clear to them that stories can positively impact patient care.
A considerable number of studies also assessed the modification of knowledge or skills as a direct result of the narrative medicine intervention (level 2b; N = 14). Liben (Citation2012) reported that faculty participants in a narrative medicine workshop demonstrated the acquisition of narrative terms in a follow-up test and later applied these narrative skills in teaching and clinical settings. Similarly, Ross (Citation2014) recorded significant improvement in a narrative skills assessment administered before and after the completion of a narrative medicine course (mean scores 51.6–71.5, p < 0.001). Cunningham (Citation2018) found that students addressed the following themes in their written narrative reflections: self-awareness, empathy, and balancing emotional distance and compassion. Other studies reported an enhanced understanding of and capability in communication (Garrison Citation2011; Arntfield et al. Citation2013; Welch Citation2016).
A number of studies reported that students had an increased sense of empathy for and connection to their patients (DasGupta and Charon Citation2004; Maurer Citation2006; Vannatta and Vannatta Citation2013; McDonald Citation2015). Sands (Citation2008) also found an improvement in empathic concern (p = 0.056) according to baseline and post-intervention assessments using the Interpersonal Reactivity Index. This being said, not all attempts to assess empathy levels before and after a narrative medicine intervention resulted in positive results. Winkel et al.’s (Citation2016) hypothesis that attending narrative medicine seminar sessions would reduce burnouts, enhance empathy, increase reflective capabilities, and help residents process the multiple stressors the encountered on the job, was tested by means of a Maslach Burnout Inventory, Interpersonal Reactivity Index, and Self-Care Inventory administered at the baseline and one year after participants’ completion of the narrative medicine seminars. The study reported a small increase in empathic concern after the narrative medicine intervention (+0.76, p = 0.01). Yet at the aggregate level, the authors found no significant difference in scores, although burnout levels remained high.
Level three: behavioral change
Three studies included in this review designed and executed tests to explicitly measure behavioral change as a result of a narrative-based medicine intervention (Balmer and Richards Citation2012; Arntfield et al. Citation2013; Bhavaraju and Miller Citation2014). These studies included multiple measurement tools and two of the three included data triangulation (Balmer and Richards Citation2012; Arntfield et al. Citation2013). Using pre- and post-intervention Likert Scale questionnaires to assess the impact of a narrative medicine faculty training intervention, Bhavaraju found an increase in participants’ confidence in writing and leading writing exercises (3.1–4.2) and increased confidence in leading literary discussions (3.7–4.4). Participants also reported integrating narrative medicine tools in their teaching (2.0–2.7). Balmer’s analysis of a faculty training program found evidence of professional growth (learning teaching strategies, applying these strategies to multiple courses), personal growth (perspective taking), and collective and communal support (seeing the “other,” affiliation, and a sense of rich connectedness). Arntfield’s assessment of an undergraduate narrative medicine elective course used three means of data collection and analysis: an anonymous pre-intervention survey, a focus group, and a follow-up survey 1.5 years after the intervention. The outcomes of this study could thus be categorized on multiple levels of the Kirpatrick model, but participants reported behavioral changes in the form of enhanced understanding of and capability in communication.
Level four: change in organizational practice or patient interaction
Two studies attempted to measure the long-term results of a narrative medicine classroom intervention on clinical skill development (Balmer and Richards Citation2012; Arntfield et al. Citation2013). Regarding changes in organizational practice, participants in Arntfield’s study reported better delivery of care in the form of a better awareness of patients’ perspectives. The goal of Balmer’s study was to explore the impact of an ongoing, process-oriented narrative medicine faculty development program on participants, and the authors explicitly stated that their intention was to look at evolving changes in interpersonal relationships and institutional practices, not to assess the individual interventions themselves. The study concluded that the participants in the faculty development program later helped shape the norms and practices in Columbia’s new curriculum. Both studies used solely qualitative methods in their analyses of the impact of the ongoing faculty seminars but were nevertheless confident that those who participated had a decisive and measurable hand in shaping the university’s medical school curriculum to include more narrative medicine practices.
Quality of evidence
A minority of publications included in this study (N = 13) did not attempt to assess the outcomes of their intervention, choosing instead to report on their development of pedagogic tools for the narrative medicine classroom. Examples include descriptions of workshop themes and designs (DasGupta Citation2003) or student and faculty feedback guides (Wald Citation2010; Citation2011; Charon, Hermann, et al. Citation2016). As these articles included informal testimonial evidence or the authors’ personal opinions, they could only be awarded a BEME strength of evidence score of 1.
We scored the majority of the remaining articles (N = 16) with a 2, meaning that the results were ambiguous, usually because of the small sample size or the fact that only one assessment tool was used. We scored five studies as a 3 on the BEME scale, meaning that conclusions in these studies could likely be linked to the results; only one study scored a 4, meaning the results were clear and likely to be true. According to our appraisal, none of the studies included in this systematic review provided unequivocal results.
Discussion
This systematic review attempted to answer the following three sub-questions: first, is there evidence of a structured model for narrative-based medicine in education? Second, is there evidence that narrative-based classroom interventions result in measurable outcomes? Finally, what is the quality and nature of the reported outcomes?
Consistency in pedagogic approach
Our review found clear evidence of a consistent and replicable methodology and pedagogic approach for narrative-based health education interventions. The seminars or courses described in the articles almost always followed the same three-step model of read-reflect-respond; in fact, the last step (response/discussion) was present in all of the articles we included in this study. The reflective exercises, in particular, can be directly linked to an important professional skill: clinical reasoning. As Maurer (Citation2006) describes, reflective exercises can promote and refine students’ clinical reasoning skills by training them to process a wide range of information, including their own experiences and sources of bias.
Variance in measurable outcomes
By using the BEME Global Scale strength of evidence and Kirkpatrick-based outcomes to code the type of learning being assessed and the quality of the results, we were able to take a broader view of narrative medicine as a pedagogic strategy. The preponderance of studies included in this review reported on Kirkpatrick’s first two outcome levels (participation, modification of attitudes or perceptions, and modification of knowledge and skills), probably because these two levels are easier to assess with tests and surveys. Still, these studies indicate two things: first, these students have learned skills in accordance with the goals and purpose of narrative medicine as outlined by course designers; second, these students are conscious of the goals and purpose of the course they have taken.
While the studies in this review reported on both elective and required courses, it is worth noting that students who actively chose to take a narrative medicine course may have been more positively predisposed to the course aims and content. Another point to keep in mind is that the number of participants in the included studies was low; this is arguably due to the fact that narrative medicine activities are best suited to small group settings. Nevertheless, this makes it more difficult to argue for the broader integration of narrative medicine in medical school programs.
Variance in strength of evidence
While the strength of the evidence was not always ideal, the studies that attempted to assess the outcomes of a narrative medicine intervention were able to measure almost exclusively positive outcomes. Those whose results were insignificant or even negative provided detailed explanations for the seemingly unexpected outcomes. For example, Winkel et al. (Citation2016), and Liu et al. (Citation2016) cited intervening factors like heavy workloads, stress, fatigue, and a resulting disillusionment with the profession as potential explanations for the small, even negative, modifications in attitudes or perceptions. Due to the stressful and intensive nature of many American medical school and residency programs, we found these explanations reasonable.
Strengths and weaknesses of this review
While the results reported in the articles included in our study are promising, a key source of bias needs to be addressed: the location of the studies. Of the 36 reported narrative medicine courses or seminars, 89% (N = 32) were conducted in the United States and 36% (N = 13) of these originated from Columbia University. At first sight, this may raise concerns about the transferability of the pedagogic tools beyond Columbia or the US. However, of the six studies that we scored a 3 or 4 on the BEME strength of evidence scale, just three originated from Columbia. The other three studies reported on interventions at other universities in the US and Canada. Furthermore, one can see an increase in non-Columbia publications over time, presumably as more educators learned about its goals and means of implementation. Of the 11 studies included in this review that were published between 2003 and 2010, 55% (N = 6) were from Columbia; in contrast, of the 25 studies published from 2011 to 2018, just 28% (N = 7) were from Columbia. It remains to be seen whether or not a similar pattern will emerge with international publications reporting on narrative medicine educational interventions.
Wieżel et al. (Citation2017) and Barber and Moreno-Leguizamon’s (Citation2017) conclude in their systematic reviews that they could find no clear narrative medicine methodology in the context of medical school interventions; our study indicates the opposite. This variation can be the result of two factors, both of which constitute strengths in our study. First, our method of assessment, the BEME Global Rating Scale, facilitated a more nuanced and transparent analysis of the reported outcomes. Second, our systematic review yielded a larger and different set of studies, with only three overlapping articles out of Barber’s nine included articles and just 8 overlapping articles out of Wieżel’s 27 included articles. Of the six articles that we gave the highest BEME strength of evidence scores, only three of were included in Wieżel’s study (Arntfield et al. Citation2013; Bhavaraju and Miller Citation2014; Chretien Citation2015) and one in Barber’s (Chretien Citation2015).
We consider it reasonable to conclude that narrative-based medicine interventions have a positive, measurable, and replicable effect on medical students and could constitute a meaningful tool to stimulate medical students’ professional and personal development. The studies included in this review also indicate that such interventions can stimulate self-reflection and empathy and that they can help students think about their patients from a different perspective or angle, thus helping them revise their notions about the doctor-patient relationship. Yet without longitudinal studies to verify the long-term impact of narrative medicine classroom interventions, at this point, we cannot unequivocally conclude that narrative medicine interventions will result in more engaged, empathic, and ultimately effective medical professionals in the future.
Conclusions
The founders of Columbia’s narrative medicine program claim that “to enter a narrative and have one’s perspective of the world altered is at the heart” of the pedagogic practice (Charon et al. Citation2016, p. 147). In the case of narrative medicine, the benefits of the training should be threefold: to reveal patients’ perspectives, to facilitate self-reflection, and as a means of providing emotional support amongst colleagues (Holmgren et al. Citation2011, p. 261). In other words, the results should later be apparent in medical professionals’ awareness of themselves, in their ability to reflect meaningfully upon their emotions and actions, in their relationships with their colleagues, and in their interactions with their patients.
While the articles in this study have argued that narrative medicine can lead to positive results in the first two aforementioned categories—more nuanced patient perspectives and a greater capacity for self-reflection—it is still unclear whether the long-term impact of such interventions are felt by patients, or whether such interventions positively impact patient care. If one of the cornerstone goals of narrative medicine is indeed to approach a patient’s story with humility, openness, and empathy (Yu Citation2017), the transfer of these goals from the classroom setting to the clinical encounter deserves further study and valorization. In other words, more research into the gap between the ideal and real practice of narrative medicine is needed to determine if, how, and to what extent the skills of interpretation and reflection taught in the narrative medicine classroom are actually implemented by students after graduation when they engage with patients in their everyday practice.
As this review has indicated, narrative medicine as a pedagogic intervention has a consistent replicable set of tools and strategies. And, while there is no lack of theoretical publications extolling the goals and virtues of a narrative-based approach, more research is needed to determine whether or not there is an ideological consensus undergirding such publications. A scoping review could help clarify, for example, which values and qualities of a medical practitioner are considered essential or important from a narrative-based approach. Such a study could also determine how these values and qualities compare with the competencies implicitly or explicitly taught in other medical school and professional health care settings.
Glossary
Narrative-(based) medicine: The practice of medicine with these skills of recognizing, absorbing, interpreting by the stories of illness; as a new frame for health care, it aims to create an effective health-care system than recognizing and respecting the persons undergoing care.
Marini MG. 2015. Narrative medicine: bridging the gap between evidence-based care and medical humanities. eBook: Springer. p. 143.
Kirkpatrick evaluation framework: Developed more than 50 years ago, the Kirkpatrick framework for evaluation has been used as a basic model for the identification and targeting of training-specific interventions in business, government, the military, and industry. It has also been employed as an assessment tool in higher education.
Rouse DN. 2011. Employing Kirkpatrick's evaluation framework to determine the effectiveness of health information management courses and programs. Perspect Health Inf Manag. 8:1c.
Supplemental Material
Download PDF (101.8 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
M. M. Milota
Megan Milota, PhD, is a lecturer in Medical Humanities at the Julius Center UMC Utrecht and holds a doctorate in English Literature.
G. J. M. W. van Thiel
Ghislaine van Thiel, MSc, PhD, is associate professor of medical ethics at the UMC Utrecht. She is chair of the Medical Research Ethics Committee of the UMC Utrecht and is a member of the Dutch Health Council.
J. J. M. van Delden
Johannes J.M. van Delden, MD PhD, is professor of medical ethics at the UMC Utrecht and director of education at the Julius Center for health sciences. He is currently the chair of the International Bioethics Committee at UNESCO and was president of CIOMS from 2011 to 2016.
References
- Al-Imari L, Yang J, Pimlott N. 2016. Peer-support writing group in a community family medicine teaching unit: facilitating professional development. Can Fam Phys. 62:E724–E730.
- Arntfield S, Slesar K, Dickson J, Charon R. 2013. Narrative medicine as a means of training medical students toward residency competencies. Pat Educ Couns. 91:280–286.
- Balmer DF, Richards BF. 2012. Faculty development as transformation: lessons learned from a process-oriented program. Teach Learn Med. 24:242–247.
- Barber S, Moreno-Leguizamon CJ. 2017. Can narrative medicine education contribute to the delivery of compassionate care? A review of the literature. Med Humanities. 43:199–203.
- Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. 2013. Teaching empathy to medical students: an updated, systematic review. Acad Med. 88:1171–1177.
- Bhavaraju VL, Miller S. 2014. Faculty development in narrative medicine: using stories to teach, learn, and thrive. J Grad Med Ed. 6:355–356.
- Charon R. 2001. The patient-physician relationship. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 286:1897–1902.
- Charon R. 2006. Narrative medicine: honoring the stories of illness. New York (NY): Oxford University Press.
- Charon R. 2007. What to do with stories: the sciences of narrative medicine. Can Fam Physician. 53:1265–1267.
- Charon R. 2008. Narrative evidence based medicine. Art Med Lancet. 371:296–297.
- Charon R, DasGupta S. 2011. Narrative medicine, or a sense of story. Lit Med. 29:vii–xiii.
- Charon R, DasGupta S, Hermann N, Irvine C, Marcus E, Rivera Colón E, Spencer D, Spiegel M. 2016. The principles and practice of narrative medicine. New York (NY): Oxford University Press.
- Charon R, Hermann N, Devlin MJ. 2016. Close reading and creative writing in clinical education: teaching attention, representation, and affiliation. Acad Med. 91:345–350.
- Chin-Yee B, Messinger A, Young LT. 2018. Three visions of doctoring: a Gadamerian dialogue. Adv Health Sci Educ Theory Pract. https://doi.org/10.1007/s10459-018-9824-3.
- Chretien KC, Swenson R, Yoon B, Julian R, Keenan J, Croffoot J, Kheirbek R. 2015. Tell me your story: a pilot narrative medicine curriculum during the medicine clerkship. J Gen Intern Med. 30:1025–1028.
- Colthart I, Bagnall G, Evans A, Allbutt H, Haig A, Illing J, McKinstry B. 2008. The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME Guide no. 10. Med Teach. 30:124–145.
- Cowen VS, Kaufman D, Schoenherr L. 2016. A review of creative and expressive writing as a pedagogical tool in medical education. Med Educ. 50:311–319.
- Cunningham H, Taylor D, Desai UA, Quiah SC, Kaplan B, Fei L, Catallozzi M, Richards B, Balmer DF, Charon R. 2018. Looking back to move forward: first-year medical Students' meta-reflections on their narrative portfolio writings. Acad Med. 93:888–894.
- DasGupta S. 2003. Reading bodies, writing bodies: self-reflection and cultural criticism in a narrative medicine curriculum. Lit Med. 22:241–256.
- DasGupta S, Charon R. 2004. Personal illness narratives: using reflective writing to teach empathy. Acad Med. 79:351–356.
- DasGupta S, Meyer D, Calero-Breckheimer A, Costley AW, Guillen S. 2006. Teaching cultural competency through narrative medicine: intersections of classroom and community. Teach Learn Med. 18:14–17.
- Devlin MJ, Richards BF, Cunningham H, Desai U, Lewis O, Mutnick A, Nidiry MAJ, Saha P, Charon R. 2015. “Where does the circle end?”: representation as a critical aspect of reflection in teaching social and behavioral sciences in medicine. Acad Psychiatry. 39:669–677.
- Feigelson S, Muller D. 2005. “Writing about medicine”: an exercise in reflection at Mount Sinai ( with five samples of student writing. Mt Sinai J Med. 72:322–326.
- Garrison D, Lyness JM, Frank JB, Epstein RM. 2011. Qualitative analysis of medical student impressions of a narrative exercise in the third-year psychiatry clerkship. Acad Med. 86:85–89.
- Gordon M, Daniel M, Patricio M. 2018. What do we mean by ‘systematic’ in health education systematic reviews and why it matters! Med Teach. 1.
- Graham S. 2009. Narrative writing and self-discovery in residency. Fam Med. 41:395–397.
- Greenhalgh T, Hurwitz B. 1999. Narrative based medicine: why study narrative? BMJ. 318:48–50.
- Greenhalgh T. 1999. Narrative based medicine: narrative based medicine in an evidence based world. BMJ. 318:323–325.
- Grossman E, Grosseman S, Azevedo GD, Figueiró-Filho EA, McKinley D. 2015. Flipped classroom on humanities: medicine, narrative and art. Med Educ. 49:1142.
- Haidet P, Jarecke J, Adams NE, Stuckey HL, Green MJ, Shapiro D, Teal CR, Wolpaw DR. 2016. A guiding framework to maximise the power of the arts in medical education: a systematic review and metasynthesis. Med Educ. 50:320–331.
- Hammick M, Dornan T, Steinert Y. 2010. Conducting a best evidence systematic review. Part 1: from idea to data coding. BEME Guide No. 13. Med Teach. 32:3–15.
- Hellerstein DJ. 2015. “The city of the hospital”: on teaching medical students to write. J Med Humanit. 36:269–289.
- Holmgren L, Fuks A, Boudreau D, Sparks T, Kreiswirth M. 2011. Terminology and praxis: clarifying the scope of narrative in medicine. Lit Med. 29:246–273.
- Hurwitz B. 2000. Narrative and the practice of medicine. Lancet. 356:2086–2089.
- Issenberg S, Mcgaghie W, Petrusa E, Gordon D, Scalese r. 2005. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 27:10–28. DOI: 10.1080/01421590500046924
- Kirkpatrick DL. 1959. Techniques for evaluating training programs. J Am Soc Train Dir. 13:3–9.
- Kirkpatrick DL. 1976. Evaluation of training. In Craig RR, editors. Training and development handbook: a guide to human resource development. 92nd ed. New York: McGraw-Hill. p. 310–319.
- Kirkpatrick DL. 1996. Invited reaction: reaction to Holton article. Hum Res Dev Quart. 7:23–25.
- Kissler MJ, Saxton B, Nuila R, Balmer DF. 2016. Professional formation in the gross anatomy lab and narrative medicine: an exploration. Acad Med. 91:772–777.
- Kuper A. 2006. Literature and medicine: A problem of assessment. Acad Med. 81:S128–S137.
- Launer J. 1999. Narrative based medicine: a narrative approach to mental health in general practice. BMJ. 318:117–119.
- Lewis B. 2011. Narrative and psychiatry. Curr Opin Psychiatry. 24:489–494.
- Liben S, Chin K, Boudreau JD, Boillat M, Steinert Y. 2012. Assessing a faculty development workshop in narrative medicine. Med Teach. 34:e813–E819.
- Littlewood S, Ypinazar V, Margolis SA, Scherpbier A, Spencer J, Dornan T. 2005. Early practical experience and the social responsiveness of clinical education: Systematic review. BMJ. 331:387–391.
- Liu GZ, Jawitz OK, Zheng D, Gusberg RJ, Kim AW. 2016. Reflective writing for medical students on the surgical clerkship: oxymoron or antidote? J Surg Educ. 73:296–304.
- Maurer MS, Costley AW, Miller PA, McCabe S, Dubin S, Cheng H, Varela-Burstein E, Lam B, Irvine C, Page KP, et al. 2006. The Columbia Cooperative Aging Program: an interdisciplinary and interdepartmental approach to geriatric education for medical interns. J Am Geriatr Soc. 54:520–526.
- Marchalik D. 2017. The return to literature-making doctors matter in the new era of medicine. Acad Med. 92:1665–1667.
- McDonald P, Ashton K, Barratt R, Doyle S, Imeson D, Meir A, Risser G. 2015. Clinical realism: a new literary genre and a potential tool for encouraging empathy in medical students. BMC Med Ed. 15:112.
- Miller E, Balmer D, Hermann N, Graham G, Charon R. 2014. Sounding narrative medicine: studying students' professional identity development at Columbia University College of Physicians and Surgeons. Acad Med. 89:335–342.
- Pearson AS, McTigue MP, Tarpley JL. 2008. Narrative medicine in surgical education. J Surg Educ. 65:99–100.
- Praslova L. 2010. Adaptation of Kirkpatrick’s four level model of training criteria to assessment of learning outcomes and program evaluation in higher education. Educ Asse Eval Acc. 22:215–225.
- Ross DA, Alpert MD, Edens EL. 2014. A narrative-based approach to teaching diagnostic criteria. Acad Psychiatry. 38:706–708.
- Sands SA, Stanley P, Charon R. 2008. Pediatric narrative oncology: interprofessional training to promote empathy, build teams, and prevent burnout. J Support Onc. 6:307–312.
- Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M, Prideaux D. 2006. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 28:497–526.
- Sullivan GM. 2011. Deconstructing quality in education research. J Grad Med Ed. 3:121–124.
- Tochel C, Haig A, Hesketh A, Cadzow A, Beggs K, Colthart I, Peacock H. 2009. The effectiveness of portfolios for post-graduate assessment and education: BEME Guide No. 12. Med Teach. 31:299–318.
- Tsai SL, Ho MJ. 2012. Can narrative medicine training improve OSCE performance? Med Educ. 46:1112–1113.
- Vannatta S, Vannatta J. 2013. Functional realism: a defense of narrative medicine. J Med Philos. 38:32–49.
- Wald HS, Reis SP, Monroe AD, Borkan JM. 2010. ‘The Loss of My Elderly Patient:’ interactive reflective writing to support medical students’ rites of passage. Med Teach. 32:E178–E184.
- Wald HS. 2011. Guiding our learners in reflective writing: a practical approach. Lit Med. 29:355–375.
- Wear D, Aultman JM. 2005. The limits of narrative: Medical student resistance to confronting inequality and oppression in literature and beyond. Med Educ. 39:1056–1065.
- Weiss T, Swede MJ. 2016. Transforming preprofessional health education through relationship-centered care and narrative medicine. Teach Learn Med. DOI: 10.1080/10401334.2016.1159566
- Welch TJ, Harrison SL. 2016. Teaching medicine through the study of literature: implementing a fourth-year distance learning elective. Acad Med. 91:360–364.
- Wesley T, Hamer D, Karam G. 2018. Implementing a narrative medicine curriculum during the internship year: an internal medicine residency program experience. Perm J. 22.
- Wieżel I, Horodeńska M, Domańska-Glonek E, Torres K. 2017. Is there a need for narrative medicine in medical students’ education? A literature review. Medscieduc. 27:559–565.
- Winkel AF, Feldman N, Moss H, Jakalow H, Simon J, Blank S. 2016. Narrative medicine workshops for obstetrics and gynecology residents and association with burnout measures. Obst Gyn. 128:27S.
- Winkel AF, Hermann N, Graham MJ, Ratan RB. 2010. No time to think: making room for reflection in obstetrics and gynecology residency. J Grad Med Educ. 2:610–615.
- Wittenberg E, Ragan SL, Ferrell B, Virani R. 2017. Creating humanistic clinicians through palliative care education. J Pain Sympt Manag. 53:153–156.
- Yu M. 2017. When I say … narrative competence. Med Educ. 51:1203–1205.