Abstract
Purpose
Student study behaviours that prioritise the UKMLA content map over the local curriculum are a significant risk for UK medical education. To mitigate this, we describe a student-centred faculty process to improve local curriculum guidance based on an evaluation of student study behaviours, concerns and needs. Responses informed the build of an online curriculum map.
Methods
A mixed methods approach was adopted, including an online anonymous survey exploring student study behaviours and preferences for curricular guidance. This was followed by student-led focus groups to explore emergent themes further. Qualitative data underwent reflexive thematic analysis.
Results
121 students responded to the survey, of which 12 consented to participate in two student-led focus groups. Five key themes emerged, including motivation for learning, student use of the intended curriculum, student experience of the enacted curriculum, the hidden curriculum, and expectations of an online curriculum map.
Conclusions
A participatory framework enabled shared aims and responsive outcomes for curricular development in the run up to the UKMLA. Student responses led to clarification of guidance, reorganisation of learning resources and optimal design of an online curriculum map which linked all content in a visible, UKMLA aligned framework, accessible to all students and teachers.
Practice points
Use a participatory framework to foster student engagement when aligning the curriculum to national standards and frameworks.
Develop a shared language for curriculum and ensure that all curriculum guidance is linked in a single framework with high visibility and accessibility such as a cloud-based map.
Ensure national requirements are visible and fully integrated into the local framework.
Use the framework as a single point of truth to drive a shared agenda for teaching, learning and assessment.
Provide adequate resourcing for ongoing faculty development, with a particular emphasis on hard-to-reach clinical teachers.
Introduction
From 2024 to 2025, all UK undergraduate medical students will be required to sit a common, national exit exam, the Medical Licensing Assessment (UKMLA), during their final or penultimate year (GMC Citation2022). This will consist of single best answer questions, the Applied Knowledge Test (AKT) and a set of quality standards guiding their final Clinical and Professional Skills Assessment (CPSA). In addition to these, medical schools will continue to set local final assessments, usually focussing on workplace and professional behaviours.
The UK professional regulatory body, the General Medical Council (GMC), first published a content map for the AKT in September 2019 (GMC Citation2019a), and updated this in March 2021 (GMC Citation2021). This included a list of core conditions, core presentations and areas of professional knowledge for the AKT, organised by areas of clinical practice such as child health and surgery. Similarly, a list of capabilities, practical skills and procedures guide the CSPA and workplace assessments. The St George’s University of London’s (SGUL) clinical syllabus follows a similar structure, with a list of core conditions and core presentations describing professional knowledge, and clinical practice outcomes which describe the professional skills and values required in the workplace and clinical assessments.
Initially, UK medical schools had concerns about the impact of the UKMLA on student learning and standards (GMC Citation2017). Experience from the US has shown that national assessments can encourage a parallel curriculum (Burk-Rafel et al. Citation2017), whereby students use national guidance, which describes minimum standards, supported by commercial learning resources, in preference to the local more comprehensive curriculum guidance and resources. Whilst all but one medical school consulted by the GMC did not oppose the aims set out by the UKMLA (GMC Citation2017), concerns arose regarding the desirability and feasibility of the assessment particularly for testing clinical and professional skills and doing so objectively within the ambitious timeline issued. These initial misgivings have evolved into a collaborative partnership between the UK Medical Schools Council and the GMC, with engagement from experienced educators from many medical schools to ensure that a robust, reliable, and valid assessment is developed that is kept up to date.
Despite this collaborative stance, disengagement from local curricula remains a significant risk of the UKMLA for UK medical education. In this study, we describe our strategy to mitigate this, which included quantitative and qualitative evaluation of how students used and experienced our current syllabus and resources, real-time improvements in the utility of guidance based on student responses, working with faculty to integrate the UKMLA content map into the local curricular structure, and optimisation of its accessibility by building an online curriculum map.
Curriculum studies: lenses and choices
Curriculum studies explore the relationship between the intentions of curriculum designer, expressed as a curriculum statement, and what actually happens in the lived experiences of students and faculty (Stenhouse Citation1975). This has usefully been described as the intended curriculum (the documented curriculum), the enacted curriculum (what educators teach) and the experienced curriculum (what students learn) (Kelly Citation2009). Impacting on all three is the hidden curriculum, by which core assumptions about education, routines, power structures and organisational factors influence the enculturation and selective engagement of students in an educational environment (Mossop et al. Citation2013).
While individual educators may vary in their approach to curriculum, learning institutions often espouse a favoured approach to curriculum theory and practice and reflect this in choices such as learning methods, student communications and staff development programmes. These approaches have been summarised in the literature as “curriculum as a body of knowledge to be transmitted,” “curriculum as product” as illustrated by competence frameworks, “curriculum as process” whereby students and faculty build shared meanings together or “curriculum as praxis,” a development on the process model whereby critical thinking and informed, committed action on curriculum arises from the process model (Smith Citation1996).
Curriculum theory and practice at St George’s, University of London 1996-present
Early years curriculum design at SGUL has evolved from the transmission model pre-1996, with didactic subject knowledge-focussed lectures dominating instruction in the five-year undergraduate medical curriculum, to systems-based curriculum post 1996, when case-based learning, early clinical experience and student selected components were introduced. The process-oriented SPICES model (student-centred, problem-based, integrated, community-based, electives and systematic) was adopted wholeheartedly for the new Graduate Entry Programme in 2000 (Harden et al. Citation1984). This influenced the five-year programme in 2007 when the clinical years of the two programmes were merged. Despite the emphasis on the process model in the choice of learning methods and learning week approach, behavioural objectives were defined for all parts of the early years and clinical years.
After 2017, while keeping the behavioural objectives in the early years, SGUL developed a competence framework for the clinical years, ‘The SGUL clinical practice outcomes.’ This is associated with a core condition list (akin to the UKMLA content map). Despite the “product” feel to the documented clinical curriculum, the clinical practice outcomes were developed by consensus with clinical colleagues, with close attention to the natural tasks and activities that arise in the workplace and with text narrative alongside the outcomes. This narrative encouraged a situated learning approach by making explicit the thinking skills and values of the community of practice they were joining (Lave and Wenger Citation2007). In this way, a process curriculum was captured in a product framework. Curriculum efforts now take a praxis approach, with critical reflection based on the values of student and patient-centredness, inclusivity, diversity and professionalism leading to curriculum re-evaluation and reform.
Exploring and developing student-centred curriculum praxis at SGUL
Over a two-year period, we created a dialectical, collaborative approach to curriculum practice with staff and students. Our aims were threefold
To work in a staff-student collaborative team to research the student experience of the current documented and enacted curriculum
To respond to the student experience while developing UKMLA aligned curriculum guidance with clinical staff
To respond to student preferences while developing and launching an online curriculum map to improve the visibility and accessibility of the curriculum
Working with students
Curriculum discussions with clinical students at SGUL habitually led to an impasse between staff and students. Wholly enculturated in the behavioural approach, students requested more detailed learning outcomes orientated to assessment preparation (Wormald et al. Citation2009; Raupach et al. Citation2013), while clinical educators exhorted students to get involved in clinical life, learn how to learn, use the workplace as the curriculum and become capable. In this study, we wanted to move out of fixed positions and into a dialectical space where students and staff better understood each other’s perspectives and moved to a shared understanding of curriculum. To achieve this, we recruited student advisors from the clinical years with a strong interest in curriculum (NA,JO,CT) to work with us throughout the project. The study began with a student workshop where problems with the current guidance were discussed openly, realistically, and constructively. Over a two year period, student advisors were equal contributors to our research team and were consulted over the suitability of new curriculum guidance developed by clinical staff.
Working with staff
Despite a desire to promote generalist skills in the undergraduate curriculum (Cohen Citation1995; Howe Citation2012; Levi Citation2017), excepting specialties such as geriatric medicine, paediatrics and general practice, the clinical curriculum at St George’s had become dominated by a single-disease approach to teaching and learning. While the UKMLA content map also encourages the single disease model (McKechnie et al. Citation2022), for the first time it did define core conditions for the undergraduate phase of medicine. While the core content map sets out only minimum standards and we expected teams to go beyond it, for the first time we had external guidance to moderate demands of specialist groups requesting curriculum time for specialty syllabi. Expert groups with consultants, who are the most senior attending doctors in a clinical team in the UK, and at least one generalist was set up for all the UKMLA areas of practice. These groups reviewed the content map, engaged in deliberation on what scope should be included beyond the map, developed schemas to group content into meaningful categories (Blissett et al. Citation2015), and agreed on a rating scale to guide students on the level of detail expected for their first year of practice after qualification (Foundation or F1). While a rating is not provided by the content map, we determined this using a consensus of experts who combined extensive experience of F1 practice and consultant level expertise in each area of practice. Following student advisor review, the new guidance was launched in September 2022 in the usual module by module, sequentially released handbook format.
Developing an online curriculum map
A dialectical approach to curriculum requires a accessible and interrogatable curriculum with the curricular detail visible in an overall holistic framework. To achieve this, we developed a partnership with University College London (UCL). With several years’ experience of an online curriculum map (Chakrabarti et al. Citation2021; Wardle et al. Citation2023), the UCL development team worked with us to build and refine a map structured to the new curriculum guidance and incorporating student preferences. The map was tested by staff and student focus groups from all years in May 2023 and launched in September 2023, giving students and all staff real-time access at the point of teaching to the entire curriculum framework for the first time.
Methods
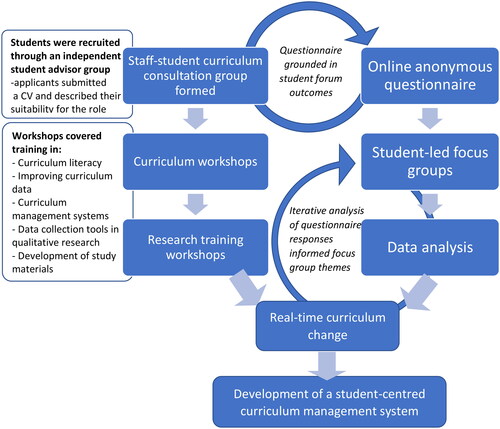
Given the complex, multilevel nature of curriculum research, we used a mixed-methods study design to explore our three aims (Fetters et al. Citation2013). Using an explanatory, sequential design, we initially used a mixed quantitative and qualitative online survey to establish a broad picture of the variety of student study behaviours, and their relative proportions. In the two focus groups that followed, qualitative methods were used to explore the reasons for the behaviours observed in the survey in more depth. In keeping with the desire to develop a student-centred curriculum practice, the design used a participatory framework whereby regular, collaborative staff-student curriculum advisor meetings provided the “engine” for the study ().
Figure 1. Flow diagram demonstrating the collaborative, student-led approach to the research design leading to real-time changes to the curriculum and the development of a curriculum management system.
Study setting and participants
The study was conducted at St George’s University, London at The Institute of Medical and Biomedical Education. Medical students in their 3rd or 4th year of training were eligible to participate. Recruitment for the survey was championed by a student advisor (NA) using oral, email and social media channels in a variety of contexts including lectures, student union events and social networks. Campaigns emphasised the participatory nature of the project and made visible the student contribution. Participants for focus groups were recruited from expressions of interest at the end of the survey.
Ethical approval
The study was approved by the Ethics Committee at St George’s University, London (approval ID:2022.0027).
Questionnaire
The questionnaire was developed after an initial student workshop and refined through reflection on how each question would address the intended, enacted, and experienced curriculum. It was then piloted on two students prior to dissemination for comprehension and refinement of wording. Participants were provided with information about the study during recruitment and at the beginning of the online questionnaire, which also established consent to take part. The questionnaire was available online between March and June 2022, and included a mix of Likert-scaled ratings and open text comments. It measured student motivation for using guidance, their perceptions of documented curriculum guidance, their use of the local curriculum as defined by learning resources (live and recorded), their use of notes from clinical learning as compared to textbooks and specialised revision websites, their experience of the relevance and quality of the local curriculum, and their expectations and reservations for a curriculum management system. The final section of the questionnaire invited students to take part in a focus group, aiming to explore their thoughts and views on the topic in more depth.
Focus groups
Consenting participants were invited to an online focus group (via MS Teams). Two focus groups were conducted in May (86 mins) and April 2022 (59 mins), using a discussion guide, to explore the hidden curriculum underpinning the survey results. The focus group interviews were each facilitated by a trained student curriculum advisor (JO, CT), mitigating any potential power relationships between students and staff that could obscure exploration of the power dynamics inherent in the hidden curriculum.
Data analysis
The focus group discussions were audio-recorded, transcribed verbatim and anonymised. The questionnaire data was analysed using SPSS, v15 for descriptive statistics (frequencies and percentages). The open text comments from the survey responses were coded and themed by a student advisor (JO) and reviewed by SB. The qualitative data from the surveys and the focus group transcripts were analysed by two student advisors (JO,CT), using a 6-phase reflexive thematic analysis (RTA) as described by Braun and Clarke (Citation2019). RTA recognises the researcher’s own biases and position in interpreting and co-constructing themes through reflective engagement with the data. The emergent themes from the focus groups were shared with SB and RA, agreed, and subsequently triangulated with the open text responses in the survey (SB). Themes were consistent across quantitative and qualitative survey data and focus groups. Subsequently, consistent with this finding, SB used a “integrating through narrative" approach to present quantitative and qualitative results together (Fetters et al. Citation2013). Results describing what functionality students would find useful in a curriculum map were used in the map development process, and are not presented in this paper.
Results
Participant demographics
The online survey was completed by 121 students (20% response rate) of which 12 students from their 3rd (n = 4, focus group 2) and 4th (n = 8, focus group 1) years consented to participate in the student-led focus groups.
Reflexive thematic analysis
The RTA led to the emergence of five key themes including motivation for learning, student use of the intended curriculum, student use and experience of the enacted curriculum, the hidden curriculum, and hopes and fears for a curriculum management system. These are described below with verbatim extracts from the online survey and focus group transcripts.
Theme 1: Motivation for learning
It was found that the primary motivation for learning among survey respondents was assessment related-the acquisition of knowledge necessary for passing assessments (93%) and maximising their competitive decile placement (76.9%). However, intrinsic interest (84.3%), good learning resources (74%), maximising participation in clinical teams (86.%) and a desire to prepare for the role of a F1 doctor (86.8%) were also all significant factors contributing to their motivation to learn. This mixture of extrinsic (assessment) and intrinsic (other) motivation was usefully illuminated by focus group participant together with the dissonance between the two motivations:
“It’s actually really helped me to look at it this way, you’re learning how to be two things. You’re learning how to be a medical student and you’re learning how to be a doctor…. and I feel like there is a massive gulf between those two things.” Focus group 1, participant 1
Theme 2: Student use of the intended curriculum
Amongst survey respondents, there was a high reported use of the core condition list (92.5%) compared with the clinical practice outcomes competence framework (41.3%) and learning objectives (41.3%) when preparing for the written assessment. Despite the core condition list giving no useful insight into the clinical competence assessment (CCA), the core condition list still informed more students (66.9%) than the competence framework (53.7%) and learning outcomes (38.9%). Qualitative comments from some students (6/9) revealed that their primary source of information for CCAs were clinical skills from the early years, with one student adding the invaluable role of bedside teaching.
“Clinical teaching fellow bedside teaching has been very helpful in putting this into perspective and being given clearer explanations of examinations.” Survey respondent 89
However, despite its high or moderate rate of use, survey respondents and focus group participants judged the intended curriculum to be unclear, complex, dispersed and hard to interrelate, with insufficient faculty explanation about how to use it. There was a high degree of agreement amongst focus group participants that the core condition list content and ratings were unclear.
“There’s so much nebulousness on the list, like gastrointestinal infections. Which ones do you want us to know about? And yes, this is seen up and down the whole list, I would like a bit more clarity on what each of those numbers (ratings) mean” Focus group 1, participant 8
There were mixed views about the competence framework, with students either finding them helpful or too wordy, and agreement that the different sources of information were not integrated.
"… for me, that’s one of the most important issues we have at the moment, that not only are important pieces of information stored separately, but they’re not integrated. It’s the integration or lack of integration, which is the key problem that I face, and I know many other people have faced as well.” Focus group 2, participant 3
While 53% of students found the core condition list easy to find on the virtual learning environment, only 21% felt this about the competence framework.
“Somewhere deep in Canvas (University resource sharing platform), there’s a booklet with 15 outcomes required for T year and stuff. But I think, if it’s more succinct, you can go show the doctor, okay, this is what is required of me, can you deliver this to us?” Focus group 2, participant 2
Theme 3: Student use and experience of the enacted curriculum
Students use a variety of learning resources when studying. Engagement with learning resources developed by lecturers and clinicians in the local curriculum is high (79.1%), and similar to personal notes made when seeing patients (78.5%) and textbooks (78.5%). However, engagement in third party resources (websites, revision courses) is more highly reported (98.5%). Probing more deeply, most students perceived the local learning resources to either be not comprehensive, or variable in their coverage or relevance to the curriculum (87%) and lack, or have variable clarity about what depth to learn (85%), a view confirmed in focus groups.
“If they (lectures) were just slightly more closely mapped to what we are actually expected to know… It’s sort of a little bit like, if 50% of them can be (fantastic), then why are the other 50% so offbeat and seemingly irrelevant to what we’re actually expected to know now, at this stage?” Focus group 1, participant 3
Most learning resources were either a mixture of organised and disorganised, or disorganised when students try to find them in the virtual learning environment (83.5%). Focus groups again identified difficulty finding learning resources as a major challenge.
“But you just can’t then re-find them very easily. Canvas is just such a maze, and Panopto (University’s online platform for sharing resources), for me, I can barely find anything.” Focus group 1, participant 6
The focus groups explored the awareness of clinical teachers of the intended curriculum and again found a disconnect.
“I’m sort of left with this core condition list to wave at people on placement, and say, I know you work for a different organisation, but can you teach me this, this, and this?” Focus group 1, participant 4
The lack of awareness of the intended curriculum also extended to faculty that set assessments, and there was a plea for all staff to be working from the intended curriculum.
“I’m not sure whether you guys felt this, but for me it was almost as if the questions and the teaching were done by two completely different people.” Focus group 2, participant 4
“…but I think everyone, those teaching, those examining and the students, all need to be working from the same hymn book type thing.” Focus group 2, participant 3
Theme 4: the hidden curriculum
Focus groups illuminated the workings of the hidden curriculum. The student “parent" system, where students are matched with mentors in the year above, emerged as a major source of advice and guidance on the curriculum from all students in focus group 2. Furthermore, a major theme in both focus groups was that, while the curriculum vision was one of workplace learning based on the competence framework, students received mixed and contradictory messages from junior and senior doctors on the value of learning in the workplace. Despite agreement that it was clinical experience that developed the capability to be a doctor, there was a continuum of advice given to students, with most junior doctors telling students to go home and study for assessments, younger consultants and registrars taking a balanced view, and older consultants feeling it was essential to spend almost all of their time on the wards.
“Probably the majority of doctors that I’ve met on the wards, have said something along the lines of, people who tend to make the best F1s, people who tend to go on to make the best doctors, have spent the most time on placement, have taken in more of that clinical experience.” Focus group 1, participant 3
“I feel like it tends to be the junior doctors who tell me, don’t be here, or, I never went to placement, and I’m fine. And then it tends to be the slightly more senior clinicians who will be like, no, you need, placement is vital, and you won’t learn anything if you’re not at placement. So, it contradicts quite a lot.” Focus group 1, participant 7
“One of the (younger) consultants on the colorectal team was like, okay, you’ve seen surgery for half a day, that’s fine, you know the ins and outs, I’ve questioned you on particular things, go and study for your exam.” Focus group 2, participant 2
Several participants described the reality of learning in the clinical workplace being more nuanced than the advice from junior doctors described but found it difficult to develop relationships with consultants because of working patterns and work pressures. This was sometimes perceived as being ignored.
“You are with the juniors, who are like, I didn’t get anything from my placement, so you won’t. And then you end up having an interesting experience. And then conversely, you might have someone who’s more senior, who’s like, placement’s the best thing ever. But then you’ll be sitting in the clinic with them, and they won’t acknowledge you.” Focus group 1, participant 7
“If you’re with them (consultants), you develop a relationship, they know what your drawbacks are that will help you improve. It might not be very feasible with the way the NHS is structured, consultants working at different periods in time.” Focus group 2, participant 2
This left students with a dilemma about the best course of action.
“Do I think about my exams, and what’s the best thing to do there? Or do I think about how to become a better clinician and doctor, and what’s going to be the best there? Because often they’re in competition with one another, and I’ve learned a lot of my experience on the job, whereas I do better in exams when I come home and sit in front of my laptop.” Focus group 1, participant 8
Theme 5: Hopes and fears for a curriculum management system
Survey respondents said they were likely or very likely (84%) to use a curriculum map, with most qualitative comments 23/35 being positive. A minority were circumspect or undecided 12/35. The desire for organisational simplicity and accessibility was a significant desire which was reported throughout the qualitative survey comments and focus groups.
“Just having everything collated together would be amazing – would save so much time and help us to stay motivated during our studies. So, by the end of the placement, I can actually look at the map and be like, I ticked all these things off whilst I was on placement. So, I think, for me, that’s where it would be useful.” Focus group 2, participant 4
Students reported a need to better understand the spiral curriculum and a hope for curriculum-assessment alignment across all lecturers, clinical teachers and assessors.
“…think, from the placements that I went on, most of the clinical teaching fellows, they themselves said they weren’t sure what we needed to know. And I think, if they had access to the curriculum, I think that would be really helpful in them guiding us on what we need to know.” Focus group 2, participant 4
“So, everyone needs to use whatever’s created to structure the teaching and structure the examinations, and the students in the middle can then use that to understand where the boundaries are about what they’re being tested on.” Focus group 2, participant 3
These hopes were tinged with realistic fears about engagement from staff, especially clinical teachers.
“I’m just not sure the clinicians themselves would necessarily use this, or they might feel like, well, actually, I’ve been practising for 20-years, and I know what medical students need to know.” Focus group 1, participant 7
“Unless they have access to it, and not only have access but are taught about it and encouraged to use it, and given time to teach us stuff, we’re stuck in the same merry-go-round, and maybe have a slightly better method of doing some self-directing learning, but as far as our placement learning goes, there won’t necessarily be that much of an improvement.” Focus group 1, participant 3
Discussion
Clinical education in the UK faces unprecedented pressures with fragmentation of clinical teams caused by the shift system, high clinical workloads, lack of recognition of teaching in job plans, and insufficient resources (GMC Citation2019b). Despite this, there is a need for the education culture to adapt to changes in work routines, acknowledge the way students learn, including embracing digital technologies, and provide the support students need to feel the workplace is a safe participatory space (Chan et al. Citation2019; Dornan et al. Citation2019). The results demonstrate the lived experience of the curriculum for clinical medical students at SGUL, explored to allow us to respond in real-time and increase engagement in the local curriculum in the run up to the UKMLA. Despite the excellent results from quality monitoring of clinical placements, we found the realities of the student experience of the clinical curriculum to be illuminating and unexpected, and this gave us clear direction for curriculum improvements and momentum for the map launch.
Contrary to the view that students are primarily motivated by assessments (Muijtjens et al. Citation1998; Wormald et al. Citation2009), the results demonstrate that almost the same number of students retain a strong vocational motivation, with sophisticated deliberation occurring in the student body about how to balance the two motivations, and mixed messages from clinical staff on the best course of action. Students perceive the intended curriculum to be complex, dispersed and lack clarity, and staff as having variable access to and awareness of the intended curriculum. The results demonstrated high extrinsic cognitive load as students struggle to access and integrate the intended curriculum and relate it to the enacted curriculum (Young et al. Citation2014). In contrast, third party resources such as revision websites and courses were almost universally used and perceived as being comprehensive, well-organised and targeted towards assessments. In response, clinical teachers reviewed all learning resources in the penultimate year and hyperlinked them to the core condition list on the virtual learning environment. Given the high use of third-party resources in our study, we might conclude that they have a part to play in medical education, but despite this, students will still engage in local curricula and benefit from its improvement.
In response to the findings, we launched the updated guidance in the online curriculum map in September 2023. All year groups were provided with live events, video and written guides. Conscious that students towards the end of training would have developed study habits using online handbooks rather than a cloud-based map, we provided both formats for penultimate and final years. Core conditions listed in the AKT blueprint are clearly marked in the map, but with a clear instruction to the students that conditions that appear not to be in the MLA may still feature in the AKT as a differential diagnosis of the AKT core presentation list, will be tested in SGUL assessments, and may well feature in the AKT blueprint revisions prior to their final year. Preliminary analytics show that 1051 of 1480 students have independently used the map (year 1 93%, year 2 68%, transition year 81%, penultimate year 56%, final year 52%) with 19000 actions in the note function to date. Small group tutors use the map with students on a weekly basis in years 1,2 and transition year.
Regarding addressing lack of awareness amongst staff, a comprehensive curriculum map launch strategy to reach academic and clinical teachers at all sites is underway with online events, face to face events, video guides and outreach visits. So far, 122 external clinical staff and 201 St George’s staff have accessed the online map. Importantly, these activities are being adequately resourced, with a part-time lecturer, data officer and curriculum manager. Given that core assumptions about education, routines, power structures and organisational factors inherent in the clinical workplace emerged as the determinants of the hidden curriculum (Mossop et al. Citation2013), a senior lecturer has been appointed to specifically address learning culture in the clinical workplace. This work began with face-to-face workshops run by staff and students about the struggles of modern medical students with respect to hardship, the skills needed for learning in a workplace under pressure and an ongoing improving engagement forum for clinical placement leads.
In conclusion, though a comprehensive study on use of the online map is yet to be done, early analytics, staff and student feedback indicate we have achieved our aims of launching a cloud-hosted online curriculum map, in which curriculum detail can be viewed in a holistic framework and its relationship to the UKMLA clarified, available to all staff and students and the point of teaching. For the majority of clinical teachers, it is the first-time any visibility of the curriculum has been possible. Together with initiatives to change the workplace learning culture amongst staff and students, we will continue our dialectical approach to clinical education development up to the UKMLA and beyond.
Acknowledgements
With thanks to Dr Annie O Leary and Dr Claire Spiller for their help aligning the St George’s curriculum with the UKMLA content map.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Shehla Baig
Dr Shehla Baig is a reader in medical education and an education associate for the General Medical Council. She is currently director of MBBS development, a member of the senior education team for MBBS at St George’s, University of London and a General Practitioner at Balham Park Surgery.
Roaa Al-bedaery
Dr. Roaa Al-bedaery, MSc, is a clinical teaching fellow, general practitioner, and lecturer at St. George’s University London with an academic interest in qualitative research, teaching evaluation and curriculum development.
Connor Togher
Connor Togher is a final year medical student at St. George’s, University of London. He has a strong interest in medical education and has worked as a clinical skills tutor, anatomy demonstrator and student curriculum advisor during his undergraduate studies.
Jonathan P.W. De Oliveira
Jonathan De Oliveira is an academic foundation doctor working at University Hospitals Bristol and Weston NHS Foundation Trust, with a strong interest in medical education. He holds a BA in History and received his MBBS from St George’s, University of London, where he was a student curriculum advisor and student lead on the academic stretch working group.
Naireen Asim
Naireen Asim is fourth-year medical student at St George’s University of London. She has a strong interest in medical education and worked on this research as a student curriculum advisor.
References
- Blissett S, Goldszmidt M, Sibbald M. 2015. Do research findings on schema-based instruction translate to the classroom? Perspect Med Educ. 4(6):334–338. doi: 10.1007/s40037-015-0225-5.
- Braun V, Clarke V. 2019. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 11(4):589–597. doi: 10.1080/2159676X.2019.1628806.
- Burk-Rafel J, Santen SA, Purkiss J. 2017. Study behaviors and USMLE Step 1 performance: implications of a student self-directed parallel curriculum. Acad Med. 92(11S):S67–S74. doi: 10.1097/ACM.0000000000001916.
- Chakrabarti R, Wardle K, Wright T, Bennie T, Gishen F. 2021. Approaching an undergraduate medical curriculum map: challenges and expectations. BMC Med Educ. 21(1):341. doi: 10.1186/s12909-021-02778-6.
- Chan M-K, Snell L, Philibert I. 2019. The education avenue of the clinical learning environment: a pragmatic approach. Med Teach. 41(4):391–397. doi: 10.1080/0142159X.2019.1566602.
- Cohen JJ. 1995. Generalism in medical education: the next steps. Acad Med. 70(1 Suppl):S7–S9. doi: 10.1097/00001888-199501000-00018.
- Dornan T, Conn R, Monaghan H, Kearney G, Gillespie H, Bennett D. 2019. Experience Based Learning (ExBL): clinical teaching for the twenty-first century. Med Teach. 41(10):1098–1105. doi: 10.1080/0142159X.2019.1630730.
- Fetters MD, Curry LA, Creswell JW. 2013. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 48(6 Pt 2):2134–2156. doi: 10.1111/1475-6773.12117.
- GMC. 2017. Report on the Medical Licensing Assessment consultation [Internet]. https://www.gmc-uk.org/-/media/documents/M05___Report_on_the_Medical_Licensing_Assessment_consultation.pdf_72007373.pdf.
- GMC. 2019a. UKMLA content map [Internet]. https://www.gmc-uk.org/-/media/documents/UKMLA-content-map-_pdf-85707770.pdf.
- GMC. 2019b. The state of medical education and practice in the UK [Internet]. [accessed 2023 Oct 25]. https://www.gmc-uk.org/-/media/documents/somep-2019–-full-report_pdf-81131156.pdf.
- GMC. 2021. Summary of changes to the UKMLA content map since the September 2019 publication [Internet]. https://www.gmc-uk.org/-/media/documents/summary-of-UKMLA-content-map-changes-march-2021_pdf-85706356.pdf.
- GMC. 2022. UK medical schools guide to the UKMLA [Internet]. n/medical-licensing-assessment/uk-medical-schools-guide-to-the-UKMLA.
- Harden RM, Sowden S, Dunn WR. 1984. Educational strategies in curriculum development: the SPICES model. Med Educ. 18(4):284–297. doi: 10.1111/j.1365-2923.1984.tb01024.x.
- Howe A. 2012. Medical generalism. Why expertise in whole person medicine matters. [Internet]. [accessed 2023 Oct 10]. https://www.rcgp.org.uk/getmedia/828af8c8-65a2-4627-9ef7-7bccd3335b6b/Medical-Generalism-Why_expertise_in_whole_person_medicine_matters.pdf.
- Kelly A. 2009. The curriculum: theory and practice. 6th ed. London: SAGE.
- Lave J, Wenger E. 2007. Situated learning: legitimate peripheral participation. New York: Cambridge University Press.
- Levi M. 2017. Generalism in modern subspecializing medicine. Eur J Intern Med. 39:36–38. doi: 10.1016/j.ejim.2017.01.002.
- McKechnie DGJ, Parmar N, Armstrong S, Pratt L, Pope L, Alberti H, Park S. 2022. General practice and the Medical Licensing Assessment. Br J Gen Pract. 72(723):497–498. https://bjgp.org/content/72/723/497. doi: 10.3399/bjgp22X720905.
- Mossop L, Dennick R, Hammond R, Robbé I. 2013. Analysing the hidden curriculum: use of a cultural web. Med Educ. 47(2):134–143. doi: 10.1111/medu.12072.
- Muijtjens AMM, Hoogenboom RJI, Verwijnen GM, Van Der Vleuten CPM. 1998. Relative or absolute standards in assessing medical knowledge using progress tests. Adv Health Sci Educ Theory Pract. 3(2):81–87. doi: 10.1023/A:1009728423412.
- Raupach T, Brown J, Anders S, Hasenfuss G, Harendza S. 2013. Summative assessments are more powerful drivers of student learning than resource intensive teaching formats. BMC Med. 11(1):61. doi: 10.1186/1741-7015-11-61.
- Smith M. 1996. Curriculum theory and practice’ The encyclopedia of pedagogy and informal education. [accessed 2023 Oct 25]. www.infed.org/biblio/b-curric.htm.
- Stenhouse L. 1975. Introduction to curriculum research and development. London: Heinemann Educational Publishers.
- Wardle K, Chakrabarti R, Wright T, Bennie T, Ntuiabane D, Gishen F. 2023. Evaluating a novel intervention in undergraduate medicine: an MBBS Curriculum Map. BMC Med Educ. 23(1):227. doi: 10.1186/s12909-023-04224-1.
- Wormald BW, Schoeman S, Somasunderam A, Penn M. 2009. Assessment drives learning: an unavoidable truth? Anat Sci Educ. 2(5):199–204. doi: 10.1002/ase.102.
- Young JQ, Van Merrienboer J, Durning S, Ten Cate O. 2014. Cognitive Load Theory: implications for medical education: AMEE Guide No. 86. Med Teach. 36(5):371–384. doi: 10.3109/0142159X.2014.889290.

