ABSTRACT
The novel coronavirus-2019 (COVID-19) pandemic has become a major health problem worldwide. The impact of COVID-19 has also been associated with psychological and social problems. The main objective of the present study was to examine the associations between fear of COVID-19 and mental wellbeing, through a serial mediation analysis that included loneliness and smartphone addiction. Utilising convenience sampling from 73 of 81 cities in Turkey via the web-based survey the present study comprised 773 participants (556 females and 217 males; aged between 18 and 66 years) were collected. Self-report data were collected including psychometric measures assessing fear of COVID-19, loneliness, smartphone addiction, and mental wellbeing. Fear of COVID-19 was found to have both a direct and indirect effect on mental wellbeing. In addition, results supported a serial mediation model where fear of COVID-19 was found to influence mental wellbeing via loneliness and smartphone addiction in a sequential manner. The findings suggest that higher fear of COVID-19 is associated with lower mental wellbeing by negatively affecting individuals’ emotion and behaviour.
1. Introduction
One of the theories explaining how individuals are motivated to act in situations that threaten health is the Protection Motivation Theory (PMT). According to this theory, the more threatening the individual perceives a life event and the more they see themselves competent in coping with it, the more they tend towards adaptive behaviours about protecting their health (Rogers and Prentice-Dunn Citation1997). Today, the situation that threatens health globally and increases stress is undoubtedly the novel coronavirus-2019 (COVID-19) pandemic. In this regard, one of the important questions is how individuals’ behaviour changed during the COVID-19 pandemic.
The COVID-19 pandemic emerged from China in December 2019 and has since spread across most countries worldwide. According to the World Health Organization, since the COVID-19 pandemic emerged, (and as of 20 August 2020), worldwide 21.3 million individuals have been infected and approximately 762,000 individuals have died (World Health Organization Citation2020a). Considering that these figures have been reached in a period of 7–8 months, COVID-19 can be said to have spread rapidly in terms of contagiousness and has a relatively high mortality rate (Lipsitch, Swerdlow, and Finelli Citation2020). This rapid spread has forced all countries with cases of COVID-19 to enforce strict measures to inhibit the spread of the disease. These precautions essentially aim to prevent individuals from coming together through means including spatial distancing, self-quarantining, and self-isolating (Abel and McQueen Citation2020; Ahorsu et al. Citation2020). As a result of these precautions, individuals have begun to go to their workplace less frequently (if at all) and stay at home more often. Consequently, this situation has forced individuals to gain new working habits and may have increased their work stress. Additionally, individuals have developed fears related to thinking about the loss of their own lives, the deaths of relatives, not engaging in habits and activities they would normally have been doing, and insufficient health services if they become sick during the COVID-19 pandemic (Angus Reid Institute Citation2020; Ornell et al. Citation2020; Pakpour and Griffiths Citation2020). Consequently, COVID-19 severely threatens and restricts many areas of human life, especially those areas concerning health and healthcare.
In Turkey (where the present study was carried out), the first COVID-19 case was reported on 11 March 2020 and measures were rapidly put into effect to control the spread of the virus. From 11 March to 3 May, 124,000 individuals have been reported as being infected with COVID-19 in Turkey, and nearly 3400 patients lost their lives (Republic of Turkey Ministry of Health Citation2020a). From the day the pandemic was initially observed until the initial writing of the present paper (beginning of May 2020), Turkey’s government enforced many measures to mitigate the spread of COVID-19, such as closing schools, enforcing spatial distancing, the use of medical face masks, prohibiting individuals younger than 20 years and older than 65 years from going outside, banning travel for dense provinces, enforcing weekend curfews in provinces with high populations, encouraging self-isolation, and quarantining individuals returning from abroad. As of 1 June 2020, curfews and travel restrictions had been lifted. In addition, places such as hotels, cafes, restaurants and places of worship were allowed to re-open on the condition that social distancing, the wearing of masks, and cleaning rules were followed. On 21 February 2021 (when the present paper was revised) 2,631,876 individuals had been reported as being infected with COVID-19 in Turkey, and 27,983 individuals had lost their lives due to COVID-19 (Republic of Turkey Ministry of Health Citation2020b).
1.1. Fear of COVID-19
One of the first emotional responses to the COVID-19 pandemic was fear. Consequently, individuals have developed both rational and irrational fears of catching the disease, dying, losing a relative, and harming others by transmitting the disease onto them (Montemurro Citation2020; Ornell et al. Citation2020). Fear is a functional emotion which ensures that an individual survives (Butter Citation2012; Öhman Citation2008). However, when experienced at excessive levels, fear may result in maladjusted behaviour (Lum and Tambyah Citation2020; van Meurs et al. Citation2014). For instance, a 50-year-old man in India with suspected COVID-19 quarantined himself to protect his family and threw stones at family members and friends who tried to approach him. He then committed suicide as a result of fear and panic (Goyal et al. Citation2020). Similarly, a 36-year-old man in Bangladesh committed suicide as a result of being identified as having COVID-19 and being excluded by individuals around him due to having a high fever, cold symptoms, and weight loss (Mamun and Griffiths Citation2020). In the former case, the individual chose loneliness and completely isolated himself from other individuals; in the second case, the individual was abandoned by society. In both cases, autopsies showed they did not even have COVID-19. The isolation precautions put in place by national governments during the COVID-19 pandemic has led to individuals spending time a lot of time alone because of self-quarantining and refraining from face-to-face social interactions. The fear of COVID-19 and the precautions taken against the pandemic have caused individuals to feel greater levels of loneliness (Armitage and Nellums Citation2020; Xiang et al. Citation2020a).
1.2. Loneliness and fear of COVID-19
Loneliness is a health-related emotional response that has arisen due to the policies put in place to inhibit the threat of COVID-19 (Okruszek et al. Citation2020). Loneliness is an emotion that must be dealt with because high levels may trigger psychological disorders such as depression and anxiety (Mishra et al. Citation2018; Panicker and Sachdev Citation2014) and can negatively affect an individual’s wellbeing (Ben-Zur and Michael Citation2016). Since health epidemics may cause many psychological disorders including depression, anxiety, stress and sleep disorders (Holmes et al. Citation2020; Liu et al. Citation2021; Mucci, Mucci, and Diolaiuti Citation2020; Plomecka et al. Citation2020), dealing with loneliness during the COVID-19 pandemic may help to protect mental health. During the epidemic, individuals either started living alone or stayed at home with family members. In addition, healthcare professionals (and other key workers) avoided face-to-face contact with their families in order to prevent the spread of COVID-19, and lived in separate rooms in the same house. Consequently, self-isolation, social distancing, and ‘stay-at-home’ orders were introduced and caused loneliness for many individuals (Banerjee and Rai Citation2020; Luchetti et al. Citation2020). In addition, it appears that individuals being able to share concerns about COVID-19 with family and friends reduces negative psychological symptoms (Plomecka et al. Citation2020). However, quarantine measures used to minimise the spread of COVID-19 reduce social interaction. Therefore, a decrease in social interactions (which is a protective factor for maintaining good mental health), is a factor that could lead to loneliness. Based on these aforementioned findings, it is likely that higher fear of COVID-19 may cause higher levels of loneliness.
1.3. Smartphone addiction and fear of COVID-19
Just as fear may be associated with COVID-19-related loneliness, individuals who already experience loneliness may experience other maladjusted behaviours related to decreasing perceived loneliness such as problematic smartphone use (Aktaş and Yılmaz Citation2017; Bian and Leung Citation2015; Enez Darcin et al. Citation2016). Although smartphone use has many positive benefits (particularly at a time where there has been reduced face-to-face contact), problematic smartphone use is particularly associated with excessive and problematic social media use (Kuss and Griffiths Citation2017). Smartphones are not only mobile telephones but also have the features of most computers. Therefore, smartphones that provide access to the internet can be useful tools for accessing information concerning the COVID-19 pandemic and communicating with others while in quarantine (van Deursen Citation2020). On the other hand, when smartphones used excessively they can also contribute to maladjusted behaviours including procrastination and skipping daily work as well as to negative physical consequences such as insomnia and neck/back pain (Fu, Chen, and Zheng Citation2020; Kwon et al. Citation2013a, Citation2013b). Consequently, although smartphones make lives easier when used functionally (Fino and Mazzetti Citation2019; Gavali et al. Citation2017), when used excessively, smartphone use may disrupt both physical and mental health among a small minority of individuals (Lapointe, Boudreau-Pinsonneault, and Vaghefi Citation2013; Oh and Kim Citation2020). Consequently, smartphones can become effective tools in coping with COVID-19 as well as being harmful to some individuals.
Smartphone addiction (the most extreme form of problematic smartphone use) is characterised by an increased desire of the phone, feelings of deprivation and restlessness when unable to reach the smartphone, an inability to stop using the smartphone and delaying daily work as a result of smartphone usage (Bian and Leung Citation2015; Kara, Baytemir, and Inceman-Kara Citation2019; Kim, Milne, and Bahl Citation2018). Although not formally recognised by any psychiatric organisations, smartphone addiction has positive correlations with psychopathological outcomes such as depression, anxiety and stress (Gökçearslan, Uluyol, and Şahin Citation2018; Matar Boumosleh and Jaalouk Citation2017) and has a negative correlation with positive wellbeing (Horwood and Anglim Citation2019; Kumcagiz and Gündüz Citation2016; Samaha and Hawi Citation2016). Consequently, smartphone addiction (like any addiction) negatively affects the quality of life of individuals. Based on these aforementioned findings, it is likely that higher fear of COVID-may cause higher levels of smartphone addiction.
1.4. Smartphone addiction and loneliness
Individuals who feel loneliness frequently use smartphones as tools to counteract the loneliness (Jiang, Li, and Shypenka Citation2018). Previous studies of loneliness and smartphone use have reported a positive correlation between loneliness and smartphone addiction (Jiang, Li, and Shypenka Citation2018; Shen and Wang Citation2019), and loneliness has been reported to be an important antecedent of problematic smartphone use and smartphone addiction (Mahapatra Citation2019). As individuals spend more time at home during the COVID-19 pandemic, smartphone use may increase as a way to pass the time, and increased smartphone use to the neglect of everything else in an individual’s life is a significant component of addiction (Elhai et al. Citation2017; Griffiths Citation2005). Therefore, both loneliness and the fear of COVID-19 may increase smartphone use, which may, in turn, lead to problematic smartphone use and possible addiction. In other words, individuals may their smartphones more to cope with the fear of COVID-19 and loneliness and therefore there may be higher levels of smartphone addiction. Based on these aforementioned findings, it is likely that higher loneliness may cause higher levels of smartphone addiction.
1.5. Wellbeing and fear of COVID-19
Previous epidemics have shown that living in regions exposed to an epidemic negatively affected the wellbeing of individuals (Kwon et al. Citation2017; Lau et al. Citation2008). One might infer from this that the COVID-19 pandemic will negatively affect the wellbeing of individuals. Mental wellbeing proposes a holistic wellbeing which unites various concepts of wellbeing (Keyes Citation2002). Mental wellbeing is defined as individuals being aware of their own abilities, being able to deal with stressful situations in life, being able to work productively and efficiently, and being beneficial to society (Keyes Citation2012; WHO Citation2004). Therefore, fear and loneliness induced by the COVID-19 pandemic may prevent individuals from being aware of their strengths and may blunt individuals’ feelings of working efficiently or being beneficial to society due to diminished or halted workflow in many areas within the framework of precautions.
Additionally, the COVID-2019 pandemic may facilitate various addictions, including excessive smartphone use, as individuals attempt to cope with these types of emotional difficulties, which can lead to the development of maladaptive coping behaviours for stress. In fact, loneliness (Lim and Kua Citation2011) and smartphone addiction (Tangmunkongvorakul et al. Citation2019) both negatively predict wellbeing. Smartphone addiction can also contribute to similar behavioural addictions such as internet addiction (Cardak Citation2013; Yu and Shek Citation2018) and social media addiction (Kuss and Griffiths Citation2017; Satici Citation2019), both of which negatively predict wellbeing. Therefore, the emotional and behavioural problems originating during the COVID-19 pandemic are likely to negatively affect some individuals’ mental wellbeing very negatively. As a result of the aforementioned theoretical and empirical research concerning the variables in the present study and the direction of the relationships between variables, it is hypothesised that there will be an association between fear of COVID-19 and mental wellbeing and that this relationship will be serially mediated by both loneliness and smartphone addiction.
2. The present study
The COVID-19 pandemic has deeply affected societies and their inhabitants physically, economically, socially, and psychologically. Determining present and potential issues caused by the pandemic is vital to determine the problems which have resulted from the pandemic and to predict potential problems which the pandemic might cause. In response to the COVID-19 pandemic, initial precautions were taken to prevent the spread of the virus and to treat infected individuals (Watkins Citation2020; Wu and McGoogan Citation2020). Other notable precautions relate to the economy (Baldwin and di Mauro Citation2020). In the field of mental health, psychosocial support services are now being offered to reduce the negative psychological effects of the pandemic (Duan and Zhu Citation2020; World Health Organization Citation2020b).
The present study investigated the associations between the fear of COVID-19 with the mental wellbeing of individuals. One of the effective routes for reducing negative psychological outcomes of epidemics is to support the strong psychological aspects of individuals and to develop wellbeing (Dewey et al. Citation2020). Understanding the association between COVID-19 and mental wellbeing will contribute to better intervention programmes intended to develop mental wellbeing.
According to PMT, information about health risk affects the individual's perception of vulnerability and efficacy against risky situations (Chamroonsawasdi et al. Citation2017; Rogers and Prentice-Dunn Citation1997). Within the framework of vulnerability and efficacy perceptions, the individual makes a threat and coping appraisal regarding the risky situations they face, and as a result, they are motivated to various behaviours to protect their health (Rogers Citation1983). Knowledge concerning COVID-19 can create fear in individuals. Fear of COVID-19 can cause individuals to consider risky situations as a threat and a difficult situation to cope with. This can strengthen the motivation to take action and increase self-isolation behaviour, which is often recommended for protection against COVID-19. Therefore, individuals may feel more alone as the time spent in self-isolation increases. Moreover, measures taken to protect health (i.e. self-isolation) may cause emotional problems for some individuals.
At the same time, individuals can use smartphones as a coping tool to protect their health in order to maintain their social relations in an isolated environment and to reach up-to-date information about COVID-19. However, increasing frequency of smartphone use may cause smartphone addiction (Gökçearslan, Uluyol, and Şahin Citation2018). Therefore, the behaviours that individuals prefer with the motivation to protect their health can turn into behaviours that can negatively affect their mental health. In addition, according to PMT, negative information about the risk factor can lead to unhealthy behaviours by increasing risk cognition (Moran, Webber, and Stanley Citation2018). Due to the fact that there is much misinformation concerning the COVID-19 pandemic is found on the internet and in social media, the increase in the use of smartphones that provide access to the internet and social media may result in increased exposure to misinformation about COVID-19. In this respect, it can be argued that lack of correct information about COVID-19 may increase fear and cause maladaptive feelings and behaviours such as loneliness and smartphone addiction. Consequently, the wellbeing of individuals may be negatively affected. More specifically, the present study examines the psychological effects of the COVID-19 pandemic by addressing the direct and indirect relationship of mental wellbeing with the fear of COVID-19, especially in relation to the mediating roles of loneliness and smartphone addiction. This is arguably another significant and novel aspect of the study.
Finally, the study investigates the relationship between COVID-19 fear with mental wellbeing in terms of the mediating roles of loneliness and smartphone addiction. Within the framework, the study will provide a significant contribution to the relevant literature concerning some of the psychological effects arising as a consequence of the COVID-19 pandemic. Consequently, the following hypotheses were proposed in the present study:
H1: Loneliness mediates the relationship between fear of COVID-19 and mental wellbeing.
H2: Smartphone addiction mediates the relationship between fear of COVID-19 and mental wellbeing.
H3: The association between fear of COVID-19 and mental wellbeing was serially mediated by both loneliness and smartphone addiction.
3. Methods
3.1. Participants and procedure
A total of 773 participants (556 females [72%] and 217 males [28%]) were recruited via web-based survey from 73 of 81 cities in Turkey. Convenience sampling was utilised in the present study, and was cross-sectional in nature. G*Power (Faul et al. Citation2009) was used to determine the required sample size. G*power is a free programme that enables researchers to determine the practical sample size. According to G*power, a sample of 218 participants is sufficient for three predictive variables with .95 real power. In addition, the N:q rule (Kline Citation2010), which is a useful rule of thumb for the relationship between sample size and model complexity, was also used. Considering Kline's expectation of 20:1 as N:q ratio, the sample size in the present study was more than sufficient.
Google Forms was used to collect online survey data. The survey link was disseminated through the social media accounts of the Turkish authors. Those who received the form were asked to share the survey link with others as well complete it themselves. Consequently, the participants from different cities of Turkey were recruited. No incentives were given to individuals to participate. All participants provided informed consent prior to taking part in the study. First, personal information was requested. This included information about COVID-19 and smartphone usage. This was followed by the psychometric measures. The online survey was planned in a way that allowed the participants to withdraw at any time. Only surveys where all questions were answered could be submitted. Therefore, there were no missing data in the study. The range age of the participants was 18–66 years (M=24.36 years, SD=7.13). A total of 521 participants were students (67%), 94 were employees in the public sector (12%), 61 were employees in the private sector (8%), and 97 were currently unemployed (13%). More detailed information about the participants is given in .
Table 1. Sample characteristics.
3.2. Measures
3.2.1. The Fear of COVID-19 Scale (FCVS19; Ahorsu et al. Citation2020)
The FCVS19 is a seven-item scale (e.g. ‘I am afraid of losing my life because of coronavirus-19’) that assesses self-rated fear of COVID-19. Items are rated on a five-point scale from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate greater fear of cororonavirus-19. The present study used the Turkish FCVS19 (Satici et al. Citation2020). The Turkish FCVS19 has very good construct validity and very good reliability. In this study, the FCVS19 also demonstrated very good reliability (α=.86 and ω=.86).
3.2.2. The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS; Tennant et al. Citation2007)
The WEMWBS is a 14-item scale (e.g. ‘I’ve been dealing with problems well’) that assesses self-rated mental wellbeing. Items were rated on a five-point scale from 1 (none of the time) to 5 (all of the time). Higher scores indicate greater mental wellbeing. The present study used the Turkish WEMWBS (Keldal Citation2015). The Turkish WEMWBS has very good construct validity, and excellent reliability (Cronbach’s α=.92). In this study, the WEMWBS also demonstrated excellent reliability (α=.90 and ω=.89).
3.2.3. The UCLA Loneliness Scale (ULS8; Hays and DiMatteo Citation1987)
The ULS8 is an eight-item scale (e.g. ‘I feel left out’) that assesses loneliness. Items are rated on a four-point scale from 1 (never) to 4 (always). Higher scores indicate greater loneliness. The present study used the Turkish ULS8 (Doğan, Çötok, and Tekin Citation2011). The Turkish ULS8 has very good construct validity and acceptable reliability. In this study, the ULS8 also demonstrated very good reliability (α=.80 and ω=.79).
3.2.4. The Smartphone Addiction Scale-Short Version (SAS, Kwon et al. Citation2013)
The SAS is a 10-item scale (e.g. ‘Using my smartphone longer than I had intended’) that assesses the risk of smartphone addiction. Items are rated on a six-point scale from 1 (strongly disagree) to 6 (strongly agree). Higher scores indicate greater risk of smartphone addiction. The present study used the Turkish SAS (Noyan et al. Citation2015). The Turkish SAS has good construct validity and excellent reliability. In this study, the SAS demonstrated very good reliability (α=.89 and ω=.89).
3.3. Statistical analysis
The analyses were carried out in sequential steps. First, the means, standard deviations, skewness, kurtosis, and bivariate correlations among the study variables were investigated. Second, a serial mediation model (PROCESS macro, model 6; Hayes Citation2018) with loneliness (first-order mediator) and smartphone addiction (second-order mediator) was conducted to test the proposed model. As this model includes two mediators, there were three specific indirect effects: (i) fear of COVID-19 → loneliness → mental wellbeing; (ii) fear of COVID-19 → smartphone addiction → mental wellbeing; and (iii) fear of COVID-19 → loneliness → smartphone addiction → mental wellbeing. To test the significance of indirect effects, 5000 bootstrap samples were used to create 95% confidence intervals (CI), which are significant if the 95% CI does not include zero. In all analyses, adjustments for potential confounding variables, such as gender and age were included.
Serial mediation analysis can be carried out with both structural equation modelling (SEM) and PROCESS macro. Hayes, Montoya, and Rockwood (Citation2017), in their study comparing SEM with PROCESS, found that there was great similarity between SEM and PROCESS in mediation model results. The ease of use of the PROCES macro is a great advantage which is why there is increasing utilisation due to its simplicity, ease of use, and similar results to SEM. Therefore, PROCESS was utilised in the present study.
3.4. Ethics
All study procedures were conducted in accordance with the ethical guidelines of the research team’s institutional review board and the Declaration of Helsinki. The data were collected online and only volunteers were asked to participate. Informed consent was obtained from the participants. Participants were informed that they could withdraw from the study at any time.
4. Results
4.1. Descriptive statistics
Means (with standard deviations in parentheses), skewness, and kurtosis of all study variables and bivariate Pearson correlation coefficients are presented in . Fear of COVID-19 was significantly and positively correlated with loneliness and smartphone addiction, and negatively correlated with mental wellbeing (see ). The results also showed that mental wellbeing was significantly and negatively correlated with loneliness and smartphone addiction.
Table 2. Descriptive statistics and correlations among study variables (N = 773).
4.2. Statistical assumption tests
Prior to analysis, assumptions of multivariate statistics were also checked. Normality of the variables was supported because the absolute values of skewness and kurtosis were not greater ±2 (George and Mallery Citation2003). All reliability coefficients above .70 indicates an acceptable internal consistency (Nunnally and Bernstein Citation1994). None of the Mahalanobis values were greater than 15, which indicated that there was no problem value. Multicollinearity was controlled via variance inflated factor (VIF), tolerance, and Durbin-Watson (DW) value. The results indicated that all VIFs were lower than 10 and tolerance values were above .10. Therefore, the findings indicated that there was no multiple linearity problem (Field Citation2016). DW value was 1.87, showing no significant correlations between the residuals. Finally, the model was examined Common Method Bias using Harman’s single factor score, which indicates that one factor explains less than the cut-off score of 50% (Mat Roni Citation2014), therefore there was no CMB problem.
4.3. Serial multiple mediational analyses
Serial multiple mediation analysis was performed after the assumptions were met. A completely standardised effect was used and reported as an effect size measure. The results (see ) showed that fear of COVID-19 significantly predicted loneliness (B=0.236, p<.001) and smartphone addiction (B=0.237, p<.001). Loneliness was also found to have a positive effect on smartphone addiction (B=0.187, p<.001). Both loneliness and smartphone addiction had a significant impact on mental wellbeing: B=−.438, p<.001 for loneliness; B=−0.087, p<.01 for smartphone addiction. Moreover, the total effect of fear of COVID-19 on mental wellbeing was significant, B=−0.231, p<.001. The (direct) effect of fear of COVID-19 on mental wellbeing continued to emerge even after controlling the impacts of loneliness and smartphone addiction, B=−0.087, p<.001.
Figure 1. The result of serial multiple mediational model, *p<.01, **p<.001. Values shown are standardised effects.
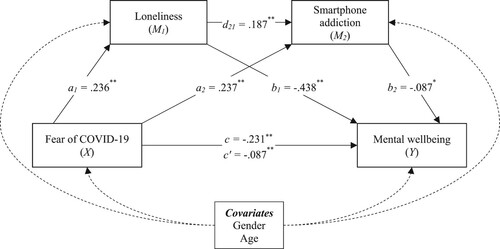
Both loneliness and smartphone addiction were found to mediate the relationship between fear of COVID-19 and mental wellbeing, B=−.104, SE=.02, 95% CI = [−.141, −.067] for loneliness; B=−.021, SE=.01, 95% CI = [−.039, −.005] for smartphone addiction. It was also found that fear of COVID-19 facilitated mental wellbeing via loneliness and then smartphone addiction (i.e. serial mediating effect), B=−.004, SE=.002, 95% CI = [−.008, −.001] (see ).
Table 3. Indirect Effect of Fear of COVID-19 on Mental Well-being via Serial Mediation.
In order to determine whether which serial mediator model was the best in the present study, reverse models were also analysed. Other variables (fear of COVID-19 = X; loneliness = M1; smartphone addiction = M2) in our model explained 27% of the dependent variable (mental well-being). In the first alternative model, fear of COVID-19 was defined as the dependent variable, mental well-being as the independent variable, and smartphone addiction (M1) and loneliness (M2) as the mediators. In this model, 23% of the dependent variable was explained. In the second alternative model, smartphone addiction was defined as the dependent variable, loneliness as the independent variable, and mental well-being (M1) and fear of COVID-19 (M2) as the mediators. In the second alternative model, 17% of the dependent variable was explained. Therefore, considering the rate of explanation of the dependent variable, the serial mediation model in the study was the best preferred model.
5. Discussion
In the present study, the mediating roles of loneliness and smartphone addiction in the relationship between fear of COVID-19 and mental wellbeing were investigated. Within this framework, the key findings were: (1) loneliness mediated the relationship between fear of COVID-19 and mental wellbeing, (2) smartphone addiction mediated the relationship between fear of COVID-19 and mental wellbeing, and (3) the association between fear of COVID-19 and mental wellbeing was serially mediated by both loneliness and smartphone addiction. Consequently, the study’s hypotheses were confirmed.
The findings confirmed the first hypothesis of the present study (H1). More specifically, an increased fear of COVID-19 was associated with increased loneliness, and this appeared to predict low mental wellbeing. A fear of COVID-19 caused individuals to experience feelings of loneliness more frequently as has been reported elsewhere (Armitage and Nellums Citation2020; Okruszek et al. Citation2020; Xiang et al. Citation2020a). It has been posited that a fear of COVID-19 can negatively affect wellbeing (Gavin et al. Citation2020), and research has shown that loneliness negatively affects wellbeing (Ben-Zur and Michael Citation2016; Lim and Kua Citation2011). Therefore, these findings are consistent with theoretical opinions (e.g. Armitage and Nellums Citation2020; Okruszek et al. Citation2020) concerning the outcomes of a fear of COVID-19 and previous research (e.g. Ben-Zur and Michael Citation2016; Gavin et al. Citation2020) and provide an integrated view of the associations between the investigated variables.
Fear of COVID-19 directs individuals to take precautions to protect their physical health. One of these precautions is for the individual to isolate from other individuals, which may result in increased feelings of loneliness. Loneliness experienced as a result of reduced social interaction negatively affects the mental wellbeing of individuals. The research here also supports the conclusion that an increased fear of COVID-19 is associated with increased risk of smartphone addiction among individuals. Furthermore, increased smartphone addiction predicts low mental wellbeing. These findings confirmed the present study’s second hypothesis (H2). Previous research has shown that fear of missing out and fear of evaluation increased smartphone addiction (Wolniewicz et al. Citation2018) and negatively predicted wellbeing (Roberts and David Citation2020). Additional findings show that smartphone addiction negatively predicts wellbeing (Horwood and Anglim Citation2019; Samaha and Hawi Citation2016). Therefore, the findings of the present study supports those of previous studies.
One reason for fear of COVID-19 increasing smartphone addiction and negatively affecting wellbeing is that individuals must remain at home more often because of the pandemic. With more time spent at home during the pandemic, individuals have increased amounts of free time, so smartphone use may increase due to the increased opportunities for free-time activities such as scrolling through social media, streaming and watching films/series, and listening to music (Chukwuere, Mbukanma, and Enwereji Citation2017). One of the important markers of smartphone addiction is the increased frequency of smartphone use (Elhai et al. Citation2017; Jiang, Li, and Shypenka Citation2018) which may lead to addiction in a minority of individuals. Excessive smartphone use is an ineffective coping strategy (Flynn, Thériault, and Williams Citation2020; Zhai et al. Citation2020) which may lower the wellbeing of individuals.
Finally, the third hypothesis of the present study was confirmed (H3). In this framework, fear of COVID-19 was associated with increased loneliness, loneliness was associated with increased smartphone addiction, and both loneliness and smartphone addiction predicted diminished mental wellbeing. No previous research has examined an association between a fear of COVID-19 and loneliness, smartphone addiction, and wellbeing. However, review studies which describe the COVID-19 pandemic have indicated that a fear of COVID-19 may cause individuals to experience increased loneliness (Okruszek et al. Citation2020) and increased smartphone use (Banskota, Healy, and Goldberg Citation2020) which negatively affected wellbeing (Ornell et al. Citation2020). Additionally, it is known that epidemics also negatively affect wellbeing (Kwon et al. Citation2017; Lau et al. Citation2008). As a result, the findings here support the conceptual view related to fear of COVID-19. In addition, as discussed above, it is consistent with research showing associations between loneliness, smartphone addiction, and mental wellbeing (e.g. Horwood and Anglim Citation2019; Lim and Kua Citation2011).
Mental wellbeing involves individuals being aware of their own abilities, coping with stressful situations in life, working productively and efficiently, and benefitting society (Keyes Citation2002, Citation2012). Fear pushes individuals to make sudden decisions and may result in excessive emotional and behavioural responses (Goyal et al. Citation2020; Mamun and Griffiths Citation2020; Öhman Citation2008). Therefore, a fear of COVID-19 may undermine an individual’s benefit to themselves and society through the ineffective use of their skills, the use of ineffective coping strategies for stress, and ineffective working. In other words, fear of COVID-19 negatively affects individuals emotionally, via loneliness, and behaviourally, via smartphone addiction, and disrupts their functioning. This dysfunction likely results in decreased mental wellbeing.
While the perception of COVID-19 as a threat increases stress levels, the fact that individuals feel themselves competent to struggle with covid-19 decreases stress levels. (Liu et al. Citation2021). Considering that stress is also negatively related to mental well-being (Linden and Stuart Citation2020), it can be said that low threat perception and high coping efficiency perception improves mental well-being. In addition, smartphones can be used as an effective tool for obtaining information and communicating with others during the epidemic (van Deursen Citation2020). In this respect, preventing smartphone addiction will increase the likelihood of using smartphones as an effective tool to cope with the epidemic, and will help facilitate good individual mental well-being.
5.1. Implications
The present study showed that a fear of COVID-19 negatively affected wellbeing by apparently causing dysfunctional feelings and behaviour in individuals. Therefore, during the COVID-19 pandemic, coping with dysfunctional feelings, developing functional coping behaviours, and supporting present functional behaviours will increase the mental wellbeing of individuals and benefit mental health. Consequently, mental health services provided during the COVID-19 pandemic should be organised to assist in improving an awareness of feelings of fear and loneliness and to encourage experiencing these feelings at optimum levels. In other words, one of the cornerstones of psychosocial support services may be developing skills related to emotional awareness, improving the ability to control feelings and coping with stress and anxiety. Additionally, preparing activities which individuals can perform with their families at home may protect against both loneliness and maladjusted behaviours such as excessive smartphone use, especially activities based on creating a product (painting, toys, food and drink, etc.) which may encourage individuals’ creativity. These types of activities can ease fear and loneliness in addition to supporting qualities related to mental wellbeing, such as discovering abilities and being productive and efficient. Therefore, as suggested by the PMT, individuals who develop effective coping strategies in relation to the COVID-19 pandemic (and which threatened their health), may feel more competent to cope with the COVID-19 pandemic. As a result, these individuals can protect their physical and mental health.
Although wellbeing levels fall as the risk of smartphone addiction increases, the effective and adaptive use of smartphones may be important for meeting the social needs of individuals during the COVID-19 pandemic. In fact, smartphones, which provide easy access to the internet, make it easier for individuals to obtain information about COVID-19 and to take precautions, and is an effective aid for communication in isolation conditions (van Deursen Citation2020). When smartphones are used effectively, they promote the development of social relationships and wellbeing (Bae Citation2019; Fitz et al. Citation2019; Mentor Citation2018). Therefore, to prevent the transformation of smartphone use into smartphone addiction during the COVID-19 pandemic, activities may be planned which promote effective and adaptive smartphone use skills to reduce the negative effects of the COVID-19 pandemic for individuals. Additionally, studies should address how to provide mental health services from a distance due to the health threat of meeting face-to-face during the pandemic (Torous and Keshavan Citation2020; Torous et al. Citation2020). It should be remembered that smartphone use that does not increase the risk of smartphone addiction may be effective in promoting mental health.
Additionally, according to PMT, negative information concerning risk factors can lead to unhealthy behaviours by increasing risk cognition (Moran, Webber, and Stanley Citation2018). Smartphones provide easy access to the internet and social media, which are frequently used as information sources. However, there are high amounts of misinformation on the internet and social media. Therefore, mental health professionals and educators need to provide individuals with skills in how they access more accurate and helpful information on the internet and social media. Consequently, individuals can develop healthier behaviours in dealing with the COVID-19 pandemic. Indeed, it has been demonstrated that smartphones can contribute to improving mental health among older adults who are among the high risk groups in contracting the virus (Kim, Park, and Kang Citation2020).
5.2. Limitations
There are some limitations to the research. First, the research data were collected via self-report scales, therefore the possibility of common methods biases should be considered (e.g. memory recall, social desirability). Second, participants were from different provinces in Turkey in different development periods, and the majority of the sample comprised young adults. These limitations should be considered when generalising the research results to the whole population. Finally, the study employed a cross-sectional design which makes it difficult to determine cause-and-effect relationships. Consequently, experimental and longitudinal studies are recommended for future research to investigate the associations between these variables.
6. Conclusion
Due to both the health threat of COVID-19 and the resultant precautions for minimising this threat, the mental health of individuals is threatened. The present study demonstrated that a fear of COVID-19 may cause loneliness; loneliness can lead to risk of smartphone addiction and these may result in reduced mental wellbeing. The findings here show the importance of protecting and developing the mental health of individuals to better cope with a fear of COVID-19 and to diminish subsequent emotional and behavioural disorders the disease may cause.
Disclosure of Interests
Download MS Word (12.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Abel, T., and D. McQueen. 2020. “The COVID-19 Pandemic Calls for Spatial Distancing and Social Closeness: Not for Social Distancing!.” International Journal of Public Health. doi:10.1007/s00038-020-01366-7.
- Ahorsu, D. K., C. Y. Lin, V. Imani, M. Saffari, M. D. Griffiths, and A. H. Pakpour. 2020. “The Fear of COVID-19 Scale: Development and Initial Validation.” International Journal of Mental Health and Addiction. Advance online publiction. doi:10.1007/s11469-020-00270-8.
- Aktaş, H., and N. Yılmaz. 2017. “Smartphone Addiction in Terms of the Elements of Loneliness and Shyness of University Youth.” International Journal of Social Sciences and Education Research 3 (1): 85–100. doi:10.24289/ijsser.283590.
- Angus Reid Institute. 2020. Half of Canadians Taking Extra Precautions as Coronavirus Continues to Spread around the Globe. Accessed May 4, 2020. http://angusreid.org/wp-content/uploads/2020/02/2020.02.04_Coronavirus.pdf.
- Armitage, R., and L. B. Nellums. 2020. “COVID-19 and the Consequences of Isolating the Elderly.” The Lancet Public Health. Advanced online publication. doi:10.1016/S2468-2667(20)30061-X.
- Bae, S. M. 2019. “The Relationship between Smartphone Use for Communication, Social Capital, and Subjective Well-Being in Korean Adolescents: Verification Using Multiple Latent Growth Modeling.” Children and Youth Services Review 96: 93–99. doi:10.1016/j.childyouth.2018.11.032.
- Baldwin, R., and B. W. di Mauro. 2020. Economics in the Time of COVID-19. London: CEPR Press.
- Banerjee, D., and M. Rai. 2020. “Social Isolation in Covid-19: The Impact of Loneliness.” International Journal of Social Psychiatry 66 (6): 525–527. doi:10.1177/0020764020922269.
- Banskota, S., M. Healy, and E. M. Goldberg. 2020. “15 Smartphone Apps for Older Adults to use While in Isolation During the COVID-19 Pandemic.” Western Journal of Emergency Medicine: AIntegrating Emergency Care with Population Health 21 (3): 514–525. http://doi.org/10.5811/westjem.2020.4.47372.
- Ben-Zur, H., and K. Michael. 2016. “Loneliness, Coping and Wellbeing Following Marital Loss and Separation: An Empirical Study.” In The Correlates of Loneliness, edited by A. Rockach, 184–214. Sharjah: Bentham Science Publishers. doi:10.2174/9781681080703116010011.
- Bian, M., and L. Leung. 2015. “Linking Loneliness, Shyness, Smartphone Addiction Symptoms, and Patterns of Smartphone use to Social Capital.” Social Science Computer Review 33 (1): 61–79. doi:10.1177/0894439314528779.
- Butter, S. 2012. “Cultural Constructions of Fear and Empathy: The Emotional Structure of Relationships in George Eliot’s Daniel Deronda (1876) and Jonathan Nasaw’s Fear Itself (2003).” In Who’s Afraid of?, edited by M. Gymnich, 109–139. Göttingen: Bonn University Press.
- Cardak, M. 2013. “Psychological Well-Being and Internet Addiction among University Students.” Turkish Online Journal of Educational Technology 12 (3): 134–141.
- Chamroonsawasdi, K., S. Chottanapund, P. Tunyasitthisundhorn, N. Phokaewsuksa, T. Ruksujarit, and P. Phasuksathaporn. 2017. “Development and Validation of a Questionnaire to Assess Knowledge, Threat and Coping Appraisal, and Intention to Practice Healthy Behaviors Related to non-Communicable Diseases in the Thai Population.” Behavioral Sciences 7 (2): 20.
- Chukwuere, J. E., I. Mbukanma, and P. C. Enwereji. 2017. “The Financial and Academic Implications of Using Smartphones among Students: A Quantitative Study.” Journal of Economics and Economic Education Research 18 (1): 1–26.
- Dewey, C., S. Hingle, E. Goelz, and M. Linzer. 2020. “Supporting Clinicians during the COVID-19 Pandemic.” Annals of Internal Medicine. Advanced online publication. doi:10.7326/M20-1033.
- Doğan, T., N. A. Çötok, and E. G. Tekin. 2011. “Reliability and Validity of the Turkish Version of the UCLA Loneliness Scale (ULS-8) among University Students.” Procedia - Social and Behavioral Sciences 15: 2058–2062.
- Duan, L., and G. Zhu. 2020. “Psychological Interventions for People Affected by the COVID-19 Epidemic.” The Lancet Psychiatry 7 (4): 300–302. doi:10.1016/S2215-0366(20)30073-0.
- Elhai, J. D., J. C. Levine, R. D. Dvorak, and B. J. Hall. 2017. “Non-social Features of Smartphone use are Most Related to Depression, Anxiety and Problematic Smartphone Use.” Computers in Human Behavior 69: 75–82. doi:10.1016/j.chb.2016.12.023.
- Enez Darcin, A., S. Kose, C. O. Noyan, S. Nurmedov, O. Yılmaz, and N. Dilbaz. 2016. “Smartphone Addiction and Its Relationship with Social Anxiety and Loneliness.” Behaviour & Information Technology 35 (7): 520–525. doi:10.1080/0144929X.2016.1158319.
- Faul, F., E. Erdfelder, A. Buchner, and A. G. Lang. 2009. “Statistical Power Analyses Using G* Power 3.1: Tests for Correlation and Regression Analyses.” Behavior Research Methods 41 (4): 1149–1160. doi:10.3758/BRM.41.4.1149.
- Field, A. 2016. Discovering Statistics Using IBM SPSS Statistics. Sage.
- Fino, E., and M. Mazzetti. 2019. “Monitoring Healthy and Disturbed Sleep through Smartphone Applications: A Review of Experimental Evidence.” Sleep and Breathing 23 (1): 13–24. doi:10.1007/s11325-018-1661-3.
- Fitz, N., K. Kushlev, R. Jagannathan, T. Lewis, D. Paliwal, and D. Ariely. 2019. “Batching Smartphone Notifications Can Improve Well-Being.” Computers in Human Behavior 101: 84–94. doi:10.1016/j.chb.2019.07.016.
- Flynn, E. A., ÉR Thériault, and S. R. Williams. 2020. “The use of Smartphones to Cope with Stress in University Students: Helpful or Harmful?” Journal of Technology in Behavioral Science. Advance online publiction. doi:10.1007/s41347-019-00125-7.
- Fu, S., X. Chen, and H. Zheng. 2020. “Exploring an Adverse Impact of Smartphone Overuse on Academic Performance via Health Issues: A Stimulus-Organism-Response Perspective.” Behaviour & Information Technology. Advance online publication. doi:10.1080/0144929X.2020.1716848.
- Gavali, M. Y., D. S. Khismatrao, Y. V. Gavali, and K. B. Patil. 2017. “Smartphone, the New Learning aid Amongst Medical Students.” Journal of Clinical and Diagnostic Research 11 (5): 5–8. doi:10.7860/JCDR/2017/20948.9826.
- Gavin, B., J. Hayden, D. Adamis, and F. McNicholas. 2020. “Caring for the Psychological Well-Being of Healthcare Professionals in the Covid-19 Pandemic Crisis.” Irish Medical Journal 113 (4): 51–53.
- George, D., and P. Mallery. 2003. SPSS for Windows Step by Step: A Simple Guide and Reference. Boston, MA: Allyn and Bacon.
- Gökçearslan, Ş, Ç Uluyol, and S. Şahin. 2018. “Smartphone Addiction, Cyberloafing, Stress and Social Support among University Students: A Path Analysis.” Children and Youth Services Review 91: 47–54. doi:10.1016/j.childyouth.2018.05.036.
- Goyal, K., P. Chauhan, K. Chhikara, P. Gupta, and M. P. Singh. 2020. “Fear of COVID 2019: First Suicidal Case in India!.” Asian Journal of Psychiatry 49: 101989. doi:10.1016/j.ajp.2020.101989.
- Griffiths, M. D. 2005. “A ‘Components’ Model of Addiction Within a Biopsychosocial Framework.” Journal of Substance Use 10: 191–197. doi:10.1080/14659890500114359.
- Hayes, A. F. 2018. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Publications.
- Hayes, A. F., A. K. Montoya, and N. J. Rockwood. 2017. “The Analysis of Mechanisms and Their Contingencies: PROCESS versus Structural Equation Modeling.” Australasian Marketing Journal 25 (1): 76–81. doi:10.1016/j.ausmj.2017.02.001.
- Hays, R. D., and M. R. DiMatteo. 1987. “A Short-Form Measure of Loneliness.” Journal of Personality Assessment 51 (1): 69–81. doi:10.1207/s15327752jpa5101_6.
- Holmes, E. A., R. C. O'Connor, V. H. Perry, I. Tracey, S. Wessely, L. Arseneault, C. Ballard, et al. 2020. “Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science.” The Lancet Psychiatry. Advanced online publication. doi:10.1016/S2215-0366(20)30168-1.
- Horwood, S., and J. Anglim. 2019. “Problematic Smartphone Usage and Subjective and Psychological Well-Being.” Computers in Human Behavior 97: 44–50. doi:10.1016/j.chb.2019.02.028.
- Jiang, Q., Y. Li, and V. Shypenka. 2018. “Loneliness, Individualism, and Smartphone Addiction among International Students in China.” Cyberpsychology, Behavior, and Social Networking 21 (11): 711–718. doi:10.1089/cyber.2018.0115.
- Kara, M., K. Baytemir, and F. Inceman-Kara. 2019. “Duration of Daily Smartphone Usage as an Antecedent of Nomophobia: Exploring Multiple Mediation of Loneliness and Anxiety.” Behaviour & Information Technology. Advanced online publication. doi:10.1080/0144929X.2019.1673485.
- Keldal, G. 2015. “Turkish Version of the Warwick-Edinburgh Mental Well-Being Scale: A Validity and Reliability Study.” Journal of Happiness & Well-Being 3 (1): 103–115.
- Keyes, C. L. 2002. “The Mental Health Continuum: From Languishing to Flourishing in Life.” Journal of Health and Social Behavior 43 (2): 207–222. doi:10.2307/3090197.
- Keyes, C. L. M. 2012. Mental Well-Being: International Contributions to the Study of Positive Mental Health. Atlanta: Springer.
- Kim, K., G. R. Milne, and S. Bahl. 2018. “Smart Phone Addiction and Mindfulness: An Intergenerational Comparison.” International Journal of Pharmaceutical and Healthcare Marketing 12 (1): 25–43. doi:10.1108/IJPHM-08-2016-0044.
- Kim, K., S. Y. Park, and H. C. Kang. 2020. “Smartphone Proficiency and Use, Loneliness, and Ego Integrity: An Examination of Older Adult Smartphone Users in South Korea.” Behaviour & Information Technology. Advance online publication. doi:10.1080/0144929X.2020.1713213.
- Kline, R. B. 2010. Principles and Practice of Structural Equation Modeling. 3rd ed. New York: Guildford Press.
- Kumcagiz, H., and Y. Gündüz. 2016. “Relationship between Psychological Well-Being and Smartphone Addiction of University Students.” International Journal of Higher Education 5 (4): 144–156. doi:10.5430/ijhe.v5n4p144.
- Kuss, D. J., and M. D. Griffiths. 2017. “Social Networking Sites and Addiction: Ten Lessons Learned.” International Journal of Environmental Research and Public Health 14: 311. doi:10.3390/ijerph14030311.
- Kwon, M., D. J. Kim, H. Cho, and S. Yang. 2013a. “The Smartphone Addiction Scale: Development and Validation of a Short Version for Adolescents.” PLoS ONE 8 (12): e83558. doi:10.1371/journal.pone.0083558.
- Kwon, H. M., T. H. Kim, M. R. Choi, B. J. Kim, H. W. Kim, O. S. Song, and H. J. Eun. 2017. “The Effects of MERS (Middle East Respiratory Syndrome) Event on the Psychosocial Wellbeing of Healthcare Workers and the Public with the Mediating Effect of Resilience.” Korean Journal of Psychosomatic Medicine 25 (2): 111–119. doi:10.22722/kjpm.2017.25.2.111.
- Kwon, M., J. Y. Lee, W. Y. Won, J. W. Park, J. A. Min, C. Hahn, X. Gu, J.-H. Choi, and D. J. Kim. 2013b. “Development and Validation of a Smartphone Addiction Scale (SAS).” PLoS ONE 8 (2): e56936. doi:10.1371/journal.pone.0056936.
- Lapointe, L., C. Boudreau-Pinsonneault, and I. Vaghefi. 2013. Is smartphone usage truly smart? A qualitative investigation of IT addictive behaviors. In: 46th Hawaii International Conference on System Sciences (pp. 1063-1072). IEEE. doi:10.1109/HICSS.2013.367.
- Lau, A. L., I. Chi, R. A. Cummins, T. M. Lee, K. L. Chou, and L. W. Chung. 2008. “The SARS (Severe Acute Respiratory Syndrome) Pandemic in Hong Kong: Effects on the Subjective Wellbeing of Elderly and Younger People.” Aging and Mental Health 12 (6): 746–760. doi:10.1080/13607860802380607.
- Lim, L. L., and E. H. Kua. 2011. “Living Alone, Loneliness, and Psychological Well-Being of Older Persons in Singapore.” Current Gerontology and Geriatrics Research 2011: 1–9. doi:10.1155/2011/673181.
- Linden, B., and H. Stuart. 2020. “Post-secondary Stress and Mental Well-Being: A Scoping Review of the Academic Literature.” Canadian Journal of Community Mental Health 39 (1): 1–32. doi:10.7870/cjcmh-2020-002.
- Lipsitch, M., D. L. Swerdlow, and L. Finelli. 2020. “Defining the Epidemiology of Covid-19 — Studies Needed.” New England Journal of Medicine 382: 1194–1196. doi:10.1056/NEJMp2002125.
- Liu, S., A. Lithopoulos, C. Q. Zhang, M. A. Garcia-Barrera, and R. E. Rhodes. 2021. “Personality and Perceived Stress During COVID-19 Pandemic: Testing the Mediating Role of Perceived Threat and Efficacy.” Personality and Individual Differences 168: 110351. doi:10.1016/j.paid.2020.110351.
- Luchetti, M., J. H. Lee, D. Aschwanden, A. Sesker, J. E. Strickhouser, A. Terracciano, and A. R. Sutin. 2020. “The Trajectory of Loneliness in Response to COVID-19.” American Psychologist. Advance online publication. doi:10.1037/amp0000690.
- Lum, L. H. W., and P. A. Tambyah. 2020. “Outbreak of COVID-19 – an Urgent Need for Good Science to Silence our Fears?” Singapore Medical Journal 61 (2): 55–57. doi:10.11622/smedj.2020018.
- Mahapatra, S. 2019. “Smartphone Addiction and Associated Consequences: Role of Loneliness and Self-Regulation.” Behaviour & Information Technology 38 (8): 833–844.
- Mamun, M. A., and M. D. Griffiths. 2020. “First COVID-19 Suicide Case in Bangladesh due to Fear of COVID-19 and Xenophobia: Possible Suicide Prevention Strategies.” Asian Journal of Psychiatry 51: 102073. doi:10.1016/j.ajp.2020.102073.
- Matar Boumosleh, J., and D. Jaalouk. 2017. “Depression, Anxiety, and Smartphone Addiction in University Students - A Cross Sectional Study.” PLoS ONE 12 (8): e0182239. doi:10.1371/journal.pone.0182239.
- Mat Roni, S. 2014. Introduction to SPSS. Edith Cowan University, SOAR Centre, Australia.
- Mentor, D. 2018. “Micro to Macro Social Connectedness Through Mobile Phone Engagement.” In Encyclopedia of Information Science and Technology, edited by M. Khosrow-Pour, 6184–6194. Hershey: IGI Global. doi:10.4018/978-1-5225-2255-3.ch537.
- Mishra, S. K., A. D. Kodwani, K. K. Kumar, and K. K. Jain. 2018. “Linking Loneliness to Depression: A Dynamic Perspective.” Benchmarking: An International Journal 25 (7): 2089–2104. doi:10.1108/BIJ-10-2016-0158.
- Montemurro, N. 2020. “The Emotional Impact of COVID-19: From Medical Staff to Common People.” Brain, Behavior, and Immunity. Advanced online publication. doi:10.1016/j.bbi.2020.03.032.
- Moran, K., J. Webber, and T. Stanley. 2018. “Protection Motivation Theory (PMT), Risk of Drowning, and Water Safety Perceptions of Adult Caregivers/Parents.” The Open Sports Sciences Journal 11 (1): 50–59.
- Mucci, F., N. Mucci, and F. Diolaiuti. 2020. “Lockdown and Isolation: Psychological Aspects of COVID-19 Pandemic in the General Population.” Clinical Neuropsychiatry 17 (2): 63–64.
- Noyan, C. O., A. Enez Darcin, S. Nurmedov, O. Yilmaz, and N. Dilbaz. 2015. “Validity and Reliability of the Turkish Version of the Smartphone Addiction Scale-Short Version among University Students.” Anadolu Psikiyatri Dergisi 16 (S1): 73–82. doi:10.5455/apd.176101.
- Nunnally, J. C., and I. H. Bernstein. 1994. Psychometric Theory. 3rd ed. New York: McGraw-Hill.
- Oh, Y. J., and H. D. Kim. 2020. “The Relationship between Perceived Smartphone Addiction and Physical and Mental Health in Female College Students.” Journal of the Korean Society of School Health 33 (1): 48–57. doi:10.15434/kssh.2020.33.1.48.
- Öhman, A. 2008. “Fear and Anxiety.” In Handbook of Emotions, edited by M. Lewis, J. M. Haviland-Jones, and L. F. Barrett, 709–729. New York: The Guilford Press.
- Okruszek, Ł, A. Aniszewska-Stańczuk, A. Piejka, M. Wiśniewska, and K. Żurek. 2020. “Safe but Lonely? Loneliness, Mental Health Symptoms and COVID-19.” PsyArXiv. Advance online publication. https://doi.org/10.31234/osf.io/9njps.
- Ornell, F., J. B. Schuch, A. O. Sordi, and F. H. P. Kessler. 2020. ““Pandemic Fear” and COVID-19: Mental Health Burden and Strategies.” Brazilian Journal of Psychiatry, (AHEAD). doi:10.1590/1516-4446-2020-0008.
- Pakpour, A. H., and M. D. Griffiths. 2020. “The Fear of Covid-19 and Its Role in Preventive Behaviors.” Journal of Concurrent Disorders 2 (1): 58–63.
- Panicker, J., and R. Sachdev. 2014. “Relations among Loneliness, Depression, Anxiety, Stress and Problematic Internet Use.” International Journal of Research in Applied, Natural and Social Sciences 2 (9): 1–10.
- Plomecka, M. B., S. Gobbi, R. Neckels, P. Radziński, B. Skórko, S. Lazerri, K. Almazidou, et al. 2020. “Mental Health Impact of COVID-19: A Global Study of Risk and Resilience Factors.” medRxiv. doi:10.1101/2020.05.05.20092023.
- Republic of Turkey Ministry of Health. 2020a. Day table of coronavirus in Turkey. Accessed May 4, 2020, from https://covid19.saglik.gov.tr/.
- Republic of Turkey Ministry of Health. 2020b. Day table of coronavirus in Turkey. Accessed October 21, 2020. https://covid19.saglik.gov.tr/.
- Roberts, J. A., and M. E. David. 2020. “The Social Media Party: Fear of Missing out (FoMO), Social Media Intensity, Connection, and Well-Being.” International Journal of Human–Computer Interaction 36 (4): 386–392. doi:10.1080/10447318.2019.1646517.
- Rogers, R. W. 1983. “Cognitive and Physiological Processes in Fear Appeals and Attitude Change: A Revised Theory of Protection Motivation.” In Social Psychophysiology, edited by J. Cacioppo, and R. Petty, 153–176. New York: Guilford Press.
- Rogers, R. W., and S. Prentice-Dunn. 1997. “Protection Motivation Theory.” In Handbook of Health Behavior Research 1: Personal and Social Determinants, edited by D. S. Gochman, 113–132. New York: Plenum Press.
- Samaha, M., and N. S. Hawi. 2016. “Relationships among Smartphone Addiction, Stress, Academic Performance, and Satisfaction with Life.” Computers in Human Behavior 57: 321–325. doi:10.1016/j.chb.2015.12.045.
- Satici, S. A. 2019. “Facebook Addiction and Subjective Well-Being: A Study of the Mediating Role of Shyness and Loneliness.” International Journal of Mental Health and Addiction 17 (1): 41–55. doi:10.1007/s11469-017-9862-8.
- Satici, B., E. Gocet-Tekin, M. E. Deniz, and S. A. Satici. 2020. “Adaptation of the Fear of COVID-19 Scale: Its Association with Psychological Distress and Life Satisfaction in Turkey.” International Journal of Mental Health Addiction. Advance online publication. doi:10.1007/s11469-020-00294-0.
- Shen, X., and J. L. Wang. 2019. “Loneliness and Excessive Smartphone use among Chinese College Students: Moderated Mediation Effect of Perceived Stressed and Motivation.” Computers in Human Behavior 95: 31–36. doi:10.1016/j.chb.2019.01.012.
- Tangmunkongvorakul, A., P. M. Musumari, K. Thongpibul, K. Srithanaviboonchai, T. Techasrivichien, S. P. Suguimoto, M. Ono-Kihara, and M. Kihara. 2019. “Association of Excessive Smartphone Use with Psychological Well-Being among University Students in Chiang Mai, Thailand.” PLoS ONE 14 (1): e0210294. doi:10.1371/journal.pone.0210294.
- Tennant, R., L. Hiller, R. Fishwick, S. Platt, S. Joseph, S. Weich, J. Parkinson, J. Secker, and S. Stewart-Brown. 2007. “The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Development and UK Validation.” Health and Quality of Life Outcomes 5 (1): 63. doi:10.1186/1477-7525-5-63.
- Torous, J., and M. Keshavan. 2020. “COVID-19, Mobile Health and Serious Mental Illness.” Schizophrenia Research. Advanced online publication. doi:10.1016/j.schres.2020.04.013.
- Torous, J., K. J. Myrick, N. Rauseo-Ricupero, and J. Firth. 2020. “Digital Mental Health and COVID-19: Using Technology Today to Accelerate the Curve on Access and Quality Tomorrow.” JMIR Mental Health 7 (3): e18848. doi:10.2196/18848.
- van Deursen, A. J. 2020. “Digital Inequality During a Pandemic: Quantitative Study of Differences in COVID-19–Related Internet Uses and Outcomes among the General Population.” Journal of Medical Internet Research 22 (8): e20073. doi:10.2196/20073.
- van Meurs, B., N. Wiggert, I. Wicker, and S. Lissek. 2014. “Maladaptive Behavioral Consequences of Conditioned Fear-Generalization: A Pronounced, yet Sparsely Studied, Feature of Anxiety Pathology.” Behaviour Research and Therapy 57: 29–37. doi:10.1016/j.brat.2014.03.009.
- Watkins, J. 2020. “Preventing a Covid-19 Pandemic.” BMJ 368: m810. doi:10.1136/bmj.m810.
- WHO (World Health Organisation). 2004. Promoting Mental Health; Concepts Emerging Evidence and Practice (Summary report). Geneva.
- WHO (World Health Organization). 2020a. Coronavirus Disease 2019 (COVID-19) Situation Report – 209. April 19. Accessed August 20, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200816-covid-19-sitrep-209.pdf?sfvrsn=5dde1ca2_2.
- WHO (World Health Organization). 2020b. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020 (No. WHO/2019-nCoV/MentalHealth/2020.1). https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf.
- Wolniewicz, C. A., M. F. Tiamiyu, J. W. Weeks, and J. D. Elhai. 2018. “Problematic Smartphone Use and Relations with Negative Affect, Fear of Missing out, and Fear of Negative and Positive Evaluation.” Psychiatry Research 262: 618–623. doi:10.1016/j.psychres.2017.09.058.
- Wu, Z., and J. M. McGoogan. 2020. “Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention.” JAMA 323 (13): 1239–1242. doi:10.1001/jama.2020.2648.
- Xiang, Y. T., Y. Yang, W. Li, L. Zhang, Q. Zhang, T. Cheung, and C. H. Ng. 2020a. “Timely Mental Health Care for the 2019 Novel Coronavirus Outbreak is Urgently Needed.” The Lancet Psychiatry 7 (3): 228–229. doi:10.1016/S2215-0366(20)30046-8.
- Yu, L., and D. T. L. Shek. 2018. “Testing Longitudinal Relationships between Internet Addiction and Well-Being in Hong Kong Adolescents: Cross-Lagged Analyses Based on Three Waves of Data.” Child Indicators Research 11 (5): 1545–1562. doi:10.1007/s12187-017-9494-3.
- Zhai, X., M. Ye, C. Wang, Q. Gu, T. Huang, K. Wang, Z. Chen, and X. Fan. 2020. “Associations among Physical Activity and Smartphone use with Perceived Stress and Sleep Quality of Chinese College Students.” Mental Health and Physical Activity 18: 100323. doi:10.1016/j.mhpa.2020.100323.

