Abstract
Purpose
To elucidate the impact of long COVID on menstruation and mental health, medical records of patients with long COVID were evaluated.
Methods
Symptoms of long COVID, QOL, mental health, and related endocrine data were compared between two groups with and without menstrual disturbances.
Results
Of 349 female patients who visited our clinic between February 2021 and March 2023, 223 patients with long COVID (aged 18–50 years) were included. Forty-four (19.7%) of the patients had menstrual symptoms associated with long COVID. The patients with menstrual symptoms were older than those without menstrual symptoms (42.5 vs. 38 years). The percentage of patients with menstrual symptoms was higher during the Omicron phase (24%) than during the Preceding (13%) and Delta (12%) phases. Cycle irregularity was the most frequent (in 63.6% of the patients), followed by severe pain (25%), heavy bleeding (20.5%), perimenopausal symptoms (18.2%), and premenstrual syndrome (15.9%). Fatigue and depression were the most frequent complications. Scores for fatigue and for QOL were significantly worse in long COVID patients with menstrual symptoms. Results of endocrine examinations showed significantly increased cortisol levels in patients with menstrual complaints.
Conclusion
Long COVID has an impact on menstrual conditions and on QOL related to menstrual conditions.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic started in 2019 and many viral variants with mutations have since emerged [Citation1,Citation2]. It has been shown that about one-third of patients may suffer from prolonged illness after surviving from the acute phase of COVID-19 [Citation3,Citation4]. Various symptoms of the prolonged illness have been evaluated by many institutions including the World Health Organization [Citation5]; however, the mechanisms of the prolonged symptoms have yet to be elucidated.
Long COVID is a complicated illness that develops after SARS-CoV-2 infection, independent of the severity of COVID-19. Long COVID is defined as symptoms that occur within 3 months after the initial infection and persist for at least 2 months [Citation5]. The major symptoms of long COVID include general fatigue, post-exertional malaise, headache, insomnia, dyspnea, cognitive dysfunction, low-grade fever, and muscle pain [Citation6,Citation7]. Proposed pathophysiological mechanisms of long COVID include pathogen persistence and viral reactivation, immune dysregulation and autoimmunity, neurological abnormalities, tissue damage due to hypoperfusion and/or microclots, autonomic and endocrine dysfunctions, and dysregulation of microbiomes [Citation6,Citation8,Citation9].
Recent studies on symptomatic trends of long COVID have shown that fatigue, headache, and insomnia became predominant in patients during the Omicron-variant phase [Citation10,Citation11]. We recently reported that the number of long COVID patients complaining of fatigue was gradually increasing during the Omicron phase regardless of the severity in the acute phase [Citation12], whereas the frequencies of dysosmia and dysgeusia were decreasing in the Omicron-variant phase. The reason why long COVID symptoms are different depending on the viral variants has not yet been determined. Moreover, the trends of long COVID symptoms in the Omicron period have made the clinical diagnosis of long COVID by differentiating from various other disorders more difficult.
Results of recent observational studies focusing on women’s health have shown that the COVID-19 pandemic has had various adverse effects on women’s menstrual periods including painful and heavy bleeding, missing periods, alteration of cycle duration, and deterioration of premenstrual symptoms [Citation13]. It has been reported that long COVID patients had higher rates of menstrual cycle changes than those in a control population [Citation14]. Regarding the prevalence of long COVID with menstrual disturbances, a multi-country survey on long COVID patients with menstrual cycles showed that about one-third of the patients had experienced various menstrual problems, such as irregular cycles and heavy periods [Citation7]. Although less prevalent, a longitudinal study also showed that 16% of women experienced menstrual cycle changes after COVID-19 [Citation15]. Given the high prevalence, clinical studies should be conducted on long COVID patients with menstrual disturbances.
We established a COVID-19 aftercare outpatient clinic (CAC) in the western area of Japan in February 2021 and we have been providing medical care for long COVID patients for more than 3 years [Citation12,Citation16,Citation17]. The aim of this study was to elucidate the characteristics of long COVID with menstrual symptoms. To characterize the clinical features of long COVID with menstrual disturbances in Japanese women, we evaluated (1) the interrelationships between the long COVID symptoms and menstrual abnormalities, (2) the impact of menstrual symptoms on QOL of long COVID patients, and (3) changes in endocrine factors in long COVD patients with menstrual symptoms.
Patients and methods
Study design and clinical evaluation of long COVID
This study was a retrospective observational study conducted at a single hospital. We obtained clinical information by reviewing the medical records of all long COVID patients who visited the CAC in the Department of General Medicine at Okayama University Hospital during the period from 15 February 2021 to 31 March 2023. Long COVID was defined as symptoms that persist for more than four weeks after the onset of COVID-19 [Citation18]. The severity of the acute phase of COVID-19 was categorized according to the criteria defined by the Ministry of Health, Labor and Welfare in Japan [Citation19]. Patients’ clinical symptoms are carefully examined by physicians in face-to-face medical interviews.
Menstrual symptoms associated with long COVID
Female long COVID patients aged between 18 and 50 years were considered for evaluating menstruation-related symptoms and general conditions related to long COVID. In the medical practice at the CAC, well-trained generalists have carefully evaluated each long COVID patient through face-to-face medical interviews and recorded the details of clinical information. Menstrual information for female long COVID patients was also obtained by reviews of medical records by the researchers. Menstrual symptoms included deterioration of painful and heavy menstrual bleeding, missing periods or small amount of bleeding, changes of cycle durations, and worsening premenstrual syndrome and perimenopausal symptoms during the phase of long COVID after individual infection.
Definitions of viral variant periods of COVID-19
According to our previous report [Citation12] based on the epidemiological classification of COVID-19 in Okayama Prefecture in Japan, we divided the COVID-19 onset periods into the Preceding phase, which is the period from the ancestral variant to the Alpha variant, before 18 July 2021; the Delta-variant phase, which is the period from 19 July 2021 to 31 December 2021, when the Delta-variant was dominant after the Alpha variant phase; and the Omicron-variant phase, which is the period after 1 January 2022, when the Omicron variant was dominant in Okayama Prefecture.
Assessment of quality of life and mental health
The Japanese version of the fatigue assessment scale (FAS) and the Japanese version of Euro QOL 5-dimensions 5-levels (EQ-5D-5L) were used to assess health-related quality of life (QOL). Patients were requested to complete the questionnaires including FAS [Citation20] and EQ-5D-5L scoring for the evaluation of fatigue status and QOL level [Citation21], respectively. A score of “0” indicates the worst QOL and a score of “1” indicates the best QOL in the evaluation of EQ-5D-5L. A score of <0.8 points was defined as an impairment of QOL in this study [Citation22]. The patients were also asked to fill out a questionnaire for self-rating depression scale (SDS) to assess mental health including depressive status [Citation23] as we previously reported [Citation11].
Endocrine examination
Hormone testing was decided by each physician to assess occult endocrine disorders. Blood samples were carefully collected in a relaxing position when the patients visited the clinic around late morning to early afternoon time. The auto-analyzer system Cobas 8000 (F. Hoffmann-La Roche AG, Basel, Switzerland) was used for measuring hormone levels at the central laboratory of our hospital. As we reported previously [Citation24], assays for serum free thyroxine (FT4) and thyrotropin (TSH) were performed by using Elecsys FT4 III and TSH kits, respectively. Plasma adrenocorticotropin (ACTH) and serum cortisol levels were determined by an electro-chemiluminescence immunoassay (ECLIA) using Elecsys ACTH and Elecsys Cortisol II kits (F. Hoffmann-La Roche AG), and assays for serum growth hormone (GH) and insulin-like growth factor (IGF)-I were completed by Elecsys GH and IGF-I kits (F. Hoffmann-La Roche AG), in which IGF-I levels were then calculated to the values of standard deviation (SD) [Citation25]. Assays for serum estradiol (E2) and follicle-stimulating hormone (FSH) were carried out by using Elecsys E2 IV and FSH II kits (F. Hoffmann-La Roche AG).
Statistical analysis
Stata SE, version 17, statistical software (StataCorp., College Station, TX, USA) was used for all analyses. The Mann–Whitney U test and Pearson’s chi-squared test were used for associations between non-normally distributed variables and between categorical variables, respectively. We also used the Student’s t-test for variables with a normal distribution. The threshold for significance was defined as *p < 0.05 and **p < 0.01.
Ethical approval
This study was approved by the Ethics Committee of Okayama University Hospital (No. 2105-030) and adhered to the Declaration of Helsinki. Information on the present study was posted on our hospital’s wall and on our website, and patients who wanted to opt out were given the opportunity to do so. Since the data in the present study were anonymized, informed consent from the patients was not required.
Results
During the study period, 651 patients visited the CAC. We excluded nine patients including five patients who visited the CAC <1 month after the onset of COVID-19 and four patients who had an unconfirmed infection or had no clear complaints (). The remaining 642 patients included 293 males (45.6%) and 349 females (54.4%). Of the 349 female patients, 39 patients were under 18 years of age and 87 patients were over 50 years of age. After excluding male patients and female patients under 18 years and over 50 years of age, 223 eligible female patients of reproductive age were evaluated by focusing on complaints regarding menstrual symptoms ().
Figure 1. Study subjects of female long COVID patients. Males and females under 18 years of age and over 50 years of age were excluded from the 642 patients with long COVID, and the remaining 223 females with long COVID were analyzed in the present study. Of the 223 female patients, 44 patients had complaints of menstrual symptoms and 179 patients did not have any complaints regarding their menstrual conditions.
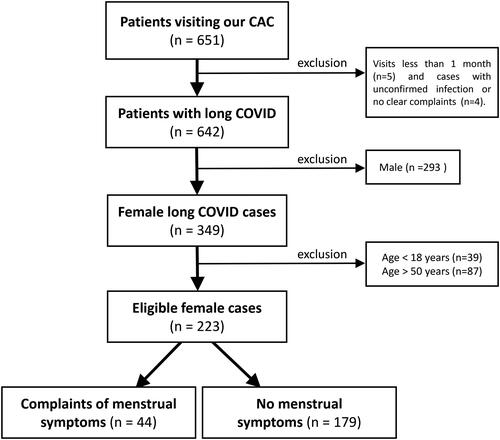
Figure 2. Distribution of ages of female long COVID patients. The black columns indicate the number of eligible female patients (44 patients) who complained of menstrual symptoms, and the gray columns indicate the number of all eligible females (223 cases).
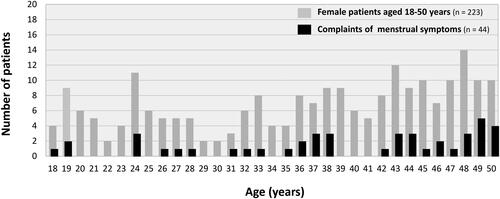
As shown in , among the 223 female patients with long COVID, 44 patients (19.7%) complained of menstrual symptoms, while the other 179 patients (80.3%) did not complain of any symptoms related to menstruation. The median ages of the patients were 42.5 [IQR: 34–48] years in the group with menstrual symptoms and 38 [IQR: 26–45] years in the group without menstrual symptoms. The patients with menstrual symptoms were significantly older than those without menstrual symptoms (*p = 0.036). The age distribution of female long COVID patients is shown in . The percentage of long COVID patients with menstrual symptoms was large in the 40’s population.
Table 1. Backgrounds of female long COVID patients aged from 18 to 50 years.
Regarding the phases of SARS-CoV-2 infection, the percentage of long COVID patients with menstrual abnormalities who were infected in the Omicron-variant phase (34 cases; 77.3%) was larger than the percentages of such patients infected in the Preceding phase (four cases; 9.1%) and Delta-variant phase (six cases; 13.6%), though the difference was not significant (p = 0.085) (). The timings of visits to the CAC were divided into three periods based on days after the onset of infection. Although the percentage of patients who visited the CAC more than 90 days after the initial infection was large regardless of menstrual symptoms, the differences between the three groups were not statistically significant.
The percentages of patients with a smoking habit and alcohol drinking habit and the levels of body mass index (BMI) were not significantly different between the two groups with and without menstrual symptoms (). The severity of the acute phase of COVID-19 was predominantly mild infection in both groups (95.5 and 90.5%, respectively). The vaccination status was also similar in the two groups (52.3 and 56.4%, respectively) and the patients who had been vaccinated had received 2–5 doses of vaccine.
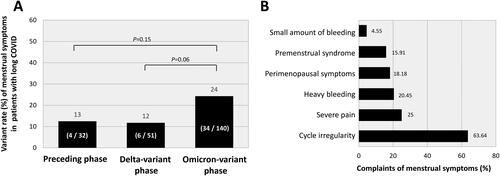
As shown in , the percentage of patients with menstrual symptoms was considerably higher during the Omicron-variant phase (34 cases; 24%) than during the Preceding phase (4 cases; 13%: p = 0.15) and the Delta-variant phase (6 cases; 12%: p = 0.06). The menstrual symptoms varied (). Cycle irregularity was the most frequent symptom (63.6%), followed by severe pain (25%), heavy bleeding (20.5%), perimenopausal symptoms (18.2%), premenstrual syndrome (15.9%) and smaller amount of bleeding (4.6%).
Figure 3. Characteristics of female long COVID patients with menstrual symptoms. (A) Variant-dependent changes in patients with menstrual symptoms. The variant rate was calculated by dividing the number of women who complained of menstrual symptoms (4, 6, and 34 cases in each phase) by the total number of women infected with each virus strain (32, 51, and 140 cases in each phase). Virus strains were presumed based on the epidemiological aspects of COVID-19 in Okayama Prefecture, Japan, categorized into three periods: the Preceding phase, before July 18, 2021; the Delta variant phase, spanning from 19 July 2021 to 31 December 2021; and the Omicron variant phase, after 1 January 2022. (B) Detailed symptoms of menstrual abnormalities in long COVID females. The percentages of the major six symptoms in 44 female patients with menstrual symptoms are shown in the columns.
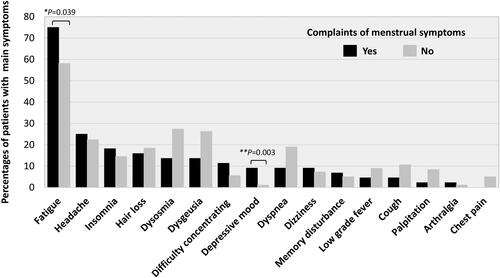
The frequencies of major sequelae in long COVID females were compared in the groups with and without menstrual symptoms (). Among the various symptoms including fatigue, headache, insomnia, hair loss, dysosmia, dysgeusia, difficulty of concentration, depressive mood, dyspnea, dizziness, memory disturbance, low-grade fever, cough, palpitation, arthralgia, chest pain, fatigue (75 vs. 58.1%: *p = 0.039), and depressive mood (9.1 vs. 1.1%: **p = 0.003) were significantly more frequent in the group with menstrual complaints ().
Figure 4. Comparison of the frequencies of major sequelae in long COVID females with and those without menstrual symptoms. The black columns indicate the frequencies of long COVID-related symptoms in patients who had menstrual complaints, and the gray columns indicate the frequencies of symptoms in patients without menstrual symptoms. The data were analyzed by the chi-squared test: **p < 0.01 and *p < 0.05 were considered statistically significant.
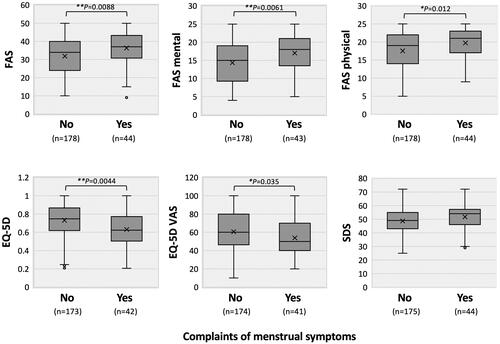
A comparison of the self-rating scales for fatigue, quality of life, and depression is shown in . The scale scores for fatigue level (FAS) and QOL (EQ), but not the score for depression (SDS), were significantly worse in the long COVID patients with menstrual symptoms. The scores for FAS, FAS mental, and FAS physical were significantly higher in the group with menstrual symptoms (37 [30.5–43.5] vs. 34 [24–40]: **p = 0.0088; 18 [13–21] vs. 15 [9–19]: **p = 0.0061; and 21 [17–23] vs. 19 [14–22]: *p = 0.012, respectively). EQ-5D and EQ-5D VAS scores were also significantly higher in the group with menstrual symptoms (0.62 [0.50–0.77] vs. 0.75 [0.62–0.87]: **p = 0.0044; and 50 [40–70] vs. 60 [45–80]: *p = 0.035, respectively) ().
Figure 5. Comparison of self-administered scales for fatigue, quality of life, and depression. FAS: fatigue assessment scale; EQ-5D: Euro QOL 5-dimensions 5-level scores; VAS: visual analog scale; SDS: self-rating depression scale. In each panel, the upper horizontal line of the box represents the 75th percentile, and the lower horizontal line of the box represents the 25th percentile. The horizontal bar within the box is the median, the upper horizontal bar outside the box is the maximum value within 1.5 times the interquartile range, and the lower horizontal bar outside the box is the minimum value within 1.5 times the interquartile range. The data were analyzed by the Mann–Whitney U test: **p < 0.01 and *p < 0.05, statistically significant between the indicated factors (“n” indicates the number of patients).
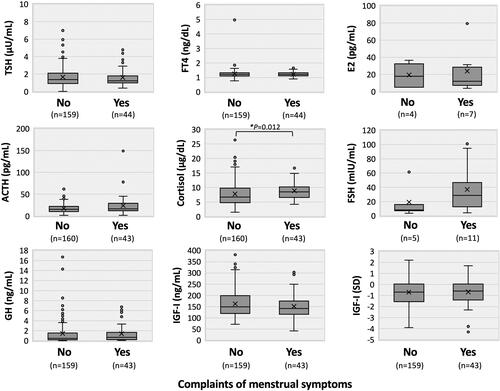
Hormonal trends in female long COVID patients with menstrual symptoms are shown in . Laboratory data showed that serum cortisol levels were significantly higher in patients with menstrual complaints than in patients without menstrual complaints (median: 8.5 [IQR: 6.5–10.4] vs. 6.7 [4.75–9.8] µg/dL: *p = 0.012), whereas plasma ACTH levels were not significantly different between the two groups (median: 16.5 [IQR: 11.8–32.4] vs. 15.4 [10.3–21.95] pg/mL: p = 0.14). Other endocrine data including thyroid functions (FT4 and TSH), other anterior pituitary functions (GH and IGF-I), and ovarian functions (E2 and FSH) did not show significant differences between the two groups, although patients with menstrual symptoms had higher serum FSH levels (median FSH: 28.7 [IQR: 11.2–52.3] vs. 8.3 [7–15.9] mIU/mL: p = 0.32) and lower serum E2 levels (median E2: 12 [IQR: 5–31.4] vs. 17.95 [5–33.75] pg/mL: p = 1.00) ().
Figure 6. Hormonal trends in female long COVID patients with menstrual symptoms. Circulating levels of thyrotropin (TSH), free thyroxine (FT4), adrenocorticotropin (ACTH), cortisol, growth hormone (GH), insulin-like growth factor (IGF)-I, estradiol (E2), and follicle-stimulating hormone (FSH) are shown in each panel. The context of each panel is shown in the legend of . The data were analyzed by the Mann–Whitney U test: *p < 0.05, statistically significant between the indicated factors (“n” indicates the number of patients).
Discussion
In the present study, we found that about one-fifth of long COVID female patients had various complaints regarding menstrual conditions. The patients with menstrual complaints included large percentages of patients who (1) were middle-aged, (2) were infected in the Omicron phase, (3) had cycle irregularity, severe pain, and heavy bleeding, (4) had fatigue and depressive mood with lowered QOL, and (5) had increased serum cortisol levels. The results of our observational study provide evidence that long COVID has a significant impact on menstrual conditions in Japanese women, leading to deterioration of QOL and mental health.
Results of recent studies have shown that COVID-19 affects the female reproductive system [Citation26,Citation27]. It has been speculated that SARS-CoV-2 infects female reproductive tissues including the ovaries and endometrium through cellular angiotensin-converting enzyme (ACE) 2 receptors [Citation26]. ACE2 is known to be expressed in the respiratory tract as well as in reproductive tissues including the ovary, uterus, and vagina [Citation28]. It has been shown that the expression of ACE2 receptors differs depending on the phases of the menstrual cycle [Citation29], being abundant in the secretory phase with interfering local homeostasis of angiotensin II [Citation30]. Since the expression of ACE2 receptors in the ovaries is involved in follicular development [Citation31,Citation32], SARS-CoV-2 infection seems likely to affect female reproductive functions [Citation27] and, at least in part, impair ovarian hormone production and endometrial responses in the periods [Citation33].
In the present study, various hormonal data, except serum cortisol levels, showed no notable differences between the long COVID groups with and without menstrual symptoms. Since the numbers of patients in the two groups were quite small, significant differences between serum levels of E2 and FSH in the two groups were not found; however, both groups showed higher levels of serum FSH than the reference values. Similarly, in women with COVID-19, it was reported that serum levels of FSH were increased and that serum levels of anti-Mullerian hormone (AMH) were decreased, whereas E2 levels were not different in women with and those without COVID-19 [Citation27]. We previously reported that fatigue including ME/CFS in adults with long COVID may be associated with endocrine dysfunctions represented by thyroid, adrenal, and pituitary hormonal effects and primary or secondary hypogonadism [Citation24,Citation34–38]. More detailed pathological and laboratory investigations are needed to elucidate the underlying mechanisms of long COVID with menstrual symptoms.
In the present study, it was revealed that premenstrual symptoms accounted for 16% of all of the complaints regarding menstrual symptoms. The scale scores for fatigue levels indicated by FAS and for QOL levels indicated by EQ were considerably worse in the long COVID patients with menstrual symptoms. A previous study showed a higher prevalence of premenstrual syndrome in women with high levels of psychosocial stress [Citation39]. Hence, premenstrual syndrome has a significant influence on women’s health and is linked to impairment of activities of daily life and mental disorders [Citation40].
Various types of stress related to the COVID-19 pandemic have exerted inhibitory effects on the regulation of the hypothalamic-pituitary-gonadal (HPG) axis. Stress and stress hormones inhibit the release of hypothalamic gonadotropin-releasing hormone (GnRH), and glucocorticoids inhibit luteinizing hormone (LH) secretion, leading to the suppression of ovarian steroidogenesis [Citation41]. The present study showed that serum cortisol levels were significantly higher in long COVID patients with menstrual complaints than in those without menstrual complaints, indicating the existence of stressful conditions due to menstrual abnormalities, in addition to the basal long COVID symptoms, leading to impairment of E2 production via the HPG axis.
Furthermore, 18% of the menstrual symptoms were classified into perimenopausal symptoms in the present study. It has been shown that premenopausal women with long COVID commonly feel deterioration of their premenstrual symptoms and that long COVID symptoms are associated with menstrual cycle changes in the week before and/or during menses [Citation7]. It has also been reported that premenopausal women have an elevated risk for long COVID [Citation42], suggesting that gonadal steroids may play a role in the prevention of long COVID [Citation43]. Since there is a considerable overlap between symptoms due to perimenopause to menopause and symptoms of long COVID, such as fatigue, sleep disturbance, brain fog, and palpitations, care should be taken to differentiate perimenopausal conditions from long COVID symptoms for appropriate application of hormonal therapy [Citation43]. Further longitudinal research is needed to determine the crucial factors for connecting long COVID status and female reproductive functions.
In the present study, it was found that the COVID-19 vaccination status had no effects on menstrual symptoms in patients with long COVID. A retrospective study in which the impact of COVID-19 and the impact of vaccination on menstrual health were compared suggested that a history of COVID-19, rather than vaccination, was linked to an increased risk of changes in menstrual conditions [Citation44]. On the other hand, an online survey of women of reproductive age [Citation45] showed that 10% of the women reported a change in the regularity of menstruation and that another 10% of the women reported a change in cycle duration after vaccination [Citation45,Citation46]. Involvement of the vaccination status in menstrual changes should also be carefully determined by considering individual causal relationships between long COVID and reproductive changes.
The results of our observational study suggested that long COVID has an impact on reproductive health in Japanese women. However, our study also has several limitations. First, the number of patients was relatively small since all of the data were obtained from a single university hospital. Second, there was no appropriate control group with known pre-infection status and there was no consideration of factors that may affect the menstrual cycle. Third, the virus variants were simply defined by the periods of infection and therefore may not be strictly accurate. Fourth, it is not known whether the menstrual disturbances are transient or not since there has been no longitudinal survey on the duration and since long COVID cases with climacteric periods were also included in this study.
Conclusion
We revealed the clinical characteristics of female long COVID patients with menstrual complaints. It was found that ∼20% of female long COVID patients have various menstrual symptoms. Since menstrual symptoms can affect physical conditions as well as mental conditions, maintenance of a normal menstrual condition is an important issue for all female long COVID patients.
Informed consent statement
Informed consent from the patients was not necessary due to the anonymization of data. Information regarding the present study was provided on our hospital wall and on the website of our hospital, and patients who wished to opt out were offered that opportunity.
Institutional review board statement
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Okayama University Hospital (No. 2105-030).
Author contributions
Y.S., Y.M., and F.O. conceived and designed the study; Y.S., Y.M., K.M., T.H., Y.O., Y.N., K.T., N.S., and K.U. performed data collection; Y.S., Y.M., K.M., N.S., H.H. (Honda), and F.O. analyzed the data; Y.S., K.T., and F.O. wrote the paper; and Y.S., Y.M., K.M., K.Y., H.H. (Hagiya), and F.O. revised the paper. All authors have read and agreed to the publication of the final version of the manuscript.
Acknowledgments
We are sincerely grateful to the clinical and office staff at the Department of General Medicine who contributed to the present work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Detailed data will be available if requested by the corresponding author.
Additional information
Funding
References
- Shrestha LB, Foster C, Rawlinson W, et al. Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: implications for immune escape and transmission. Rev Med Virol. 2022;32(5):1. doi:10.1002/rmv.2381
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–10. doi:10.1016/S0140-6736(20)30183-5
- Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi:10.1038/s41591-021-01283-z
- Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869–875. doi:10.1016/j.dsx.2021.04.007
- Soriano JB, Murthy S, Marshall JC, et al. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–e107. doi:10.1016/S1473-3099(21)00703-9
- Davis HE, McCorkell L, Vogel JM, et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133–146. doi:10.1038/s41579-022-00846-2
- Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi:10.1016/j.eclinm.2021.101019
- Klein J, Wood J, Jaycox J, et al. Distinguishing features of long COVID identified through immune profiling. Nature. 2023;623(7985):139–148. doi:10.1038/s41586-023-06651-y
- Monje M, Iwasaki A. The neurobiology of long COVID. Neuron. 2022;110(21):3484–3496. doi:10.1016/j.neuron.2022.10.006
- Sunada N, Nakano Y, Otsuka Y, et al. Characteristics of sleep disturbance in patients with long COVID: a retrospective observational study in Japan. J Clin Med. 2022;11(24):7332.
- Fujita K, Otsuka Y, Sunada N, et al. Manifestation of headache affecting quality of life in long COVID patients. J Clin Med. 2023;12(10):3533.
- Nakano Y, Otsuka Y, Honda H, et al. Transitional changes in fatigue-related symptoms due to long COVID: a single-Center retrospective observational study in Japan. Medicina. 2022;58(10):1393.doi:10.3390/medicina58101393
- Maher M, Owens L. SARS-CoV-2 infection and female reproductive health: a narrative review. Best Pract Res Clin Endocrinol Metab. 2023;37(4):101760. doi:10.1016/j.beem.2023.101760
- Medina-Perucha L, Lopez-Jimenez T, Holst AS, et al. Self-reported menstrual alterations during the COVID-19 syndemic in Spain: a cross-sectional study. Int J Womens Health. 2022;14:529–544. doi:10.2147/IJWH.S354655
- Khan SM, Shilen A, Heslin KM, et al. SARS-CoV-2 infection and subsequent changes in the menstrual cycle among participants in the Arizona CoVHORT study. Am J Obstet Gynecol. 2022;226(2):270–273. doi:10.1016/j.ajog.2021.09.016
- Otsuka Y, Tokumasu K, Nakano Y, et al. Clinical characteristics of Japanese patients who visited a COVID-19 aftercare clinic for post-acute sequelae of COVID-19/long COVID. Cureus. 2021;13(10):e18568. doi:10.7759/cureus.18568
- Sakurada Y, Sunada N, Honda H, et al. Serial changes of long COVID symptoms and clinical utility of serum antibody titers for evaluation of long COVID. J Clin Med. 2022;11(5):1309.
- Siso-Almirall A, Brito-Zeron P, Conangla Ferrin L, et al. Long covid-19: proposed primary care clinical guidelines for diagnosis and disease management. Int J Environ Res Public Health. 2021;18(8):4350.
- Kato Y. Case management of COVID-19 (secondary version). JMA J. 2021;4(3):191–197. doi:10.31662/jmaj.2021-0036
- De Vries J, Michielsen H, Van Heck GL, et al. Measuring fatigue in sarcoidosis: the fatigue assessment scale (FAS). Br J Health Psychol. 2004;9(Pt 3):279–291. doi:10.1348/1359107041557048
- Shiroiwa T, Ikeda S, Noto S, et al. Comparison of value set based on DCE and/or TTO data: scoring for EQ-5D-5L health states in Japan. Value Health. 2016;19(5):648–654. doi:10.1016/j.jval.2016.03.1834
- Ikeda S, Shiroiwa T, Igarashi A, et al. Developing a Japanese version of the EQ-5D-5L value set. J Natl Inst Public Health. 2015;64(1):47–55.
- Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12(1):63–70. doi:10.1001/archpsyc.1965.01720310065008
- Sunada N, Honda H, Nakano Y, et al. Hormonal trends in patients suffering from long COVID symptoms. Endocr J. 2022;69(10):1173–1181. doi:10.1507/endocrj.EJ22-0093
- Isojima T, Shimatsu A, Yokoya S, et al. Standardized centile curves and reference intervals of serum insulin-like growth factor-I (IGF-I) levels in a normal Japanese population using the LMS method. Endocr J. 2012;59(9):771–780. doi:10.1507/endocrj.ej12-0110
- Li R, Yin T, Fang F, et al. Potential risks of SARS-CoV-2 infection on reproductive health. Reprod Biomed Online. 2020;41(1):89–95. doi:10.1016/j.rbmo.2020.04.018
- Ding T, Wang T, Zhang J, et al. Analysis of ovarian injury associated with COVID-19 disease in reproductive-aged women in Wuhan, China: an observational study. Front Med. 2021;8:635255. doi:10.3389/fmed.2021.635255
- Jing Y, Run-Qian L, Hao-Ran W, et al. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol Hum Reprod. 2020;26(6):367–373. doi:10.1093/molehr/gaaa030
- Pan PP, Zhan QT, Le F, et al. Angiotensin-converting enzymes play a dominant role in fertility. Int J Mol Sci. 2013;14(10):21071–21086. doi:10.3390/ijms141021071
- Vaz-Silva J, Carneiro MM, Ferreira MC, et al. The vasoactive peptide angiotensin-(1-7), its receptor mas and the angiotensin-converting enzyme type 2 are expressed in the human endometrium. Reprod Sci. 2009;16(3):247–256. doi:10.1177/1933719108327593
- Barreta MH, Gasperin BG, Ferreira R, et al. The components of the angiotensin-(1-7) system are differentially expressed during follicular wave in cattle. J Renin Angiotensin Aldosterone Syst. 2015;16(2):275–283. doi:10.1177/1470320313491996
- Pereira VM, Reis FM, Santos RA, et al. Gonadotropin stimulation increases the expression of angiotensin-(1–7) and MAS receptor in the rat ovary. Reprod Sci. 2009;16(12):1165–1174. doi:10.1177/1933719109343309
- Sharp GC, Fraser A, Sawyer G, et al. The COVID-19 pandemic and the menstrual cycle: research gaps and opportunities. Int J Epidemiol. 2022;51(3):691–700. doi:10.1093/ije/dyab239
- Soejima Y, Otsuka Y, Tokumasu K, et al. Late-Onset hypogonadism in a male patient with long COVID diagnosed by exclusion of ME/CFS. Medicina. 2022;58(4):536. doi:10.3390/medicina58040536
- Yamamoto Y, Otsuka Y, Sunada N, et al. Detection of male hypogonadism in patients with post COVID-19 condition. J Clin Med. 2022;11(7):1955.
- Otsuka Y, Otsuka F. Possibility of endocrine dysfunction in post coronavirus disease 2019 (COVID-19) condition. Endocr J. 2022;69(11):1357–1357. doi:10.1507/endocrj.EJ22-0459
- Yamamoto Y, Otsuka Y, Tokumasu K, et al. Utility of serum ferritin for predicting myalgic encephalomyelitis/chronic fatigue syndrome in patients with long COVID. J Clin Med. 2023;12(14):4737.
- Sunada N, Otsuka Y, Honda H, et al. Phase-dependent trends of male hypogonadism in long COVID patients. Endocr J. 2023;70(7):755–756. doi:10.1507/endocrj.EJ23-0266
- Warner P, Bancroft J. Factors related to self-reporting of the pre-menstrual syndrome. Br J Psychiatry. 1990;157(2):249–260. doi:10.1192/bjp.157.2.249
- Yonkers KA, O’Brien PM, Eriksson E. Premenstrual syndrome. Lancet. 2008;371(9619):1200–1210. doi:10.1016/S0140-6736(08)60527-9
- Toufexis D, Rivarola MA, Lara H, et al. Stress and the reproductive axis. J Neuroendocrinol. 2014;26(9):573–586. doi:10.1111/jne.12179
- Sigfrid L, Drake TM, Pauley E, et al. Long covid in adults discharged from UK hospitals after covid-19: a prospective, multicentre cohort study using the ISARIC WHO clinical characterisation protocol. Lancet Reg Health Eur. 2021;8:100186. doi:10.1016/j.lanepe.2021.100186
- Stewart S, Newson L, Briggs TA, et al. Long COVID risk – a signal to address sex hormones and women’s health. Lancet Reg Health Eur. 2021;11:100242. doi:10.1016/j.lanepe.2021.100242
- Alvergne A, Kountourides G, Argentieri MA, et al. A retrospective case-control study on menstrual cycle changes following COVID-19 vaccination and disease. iScience. 2023;26(4):106401. doi:10.1016/j.isci.2023.106401
- Qazi TB, Dkhar SA, Quansar R, et al. Impact of COVID-19 vaccination on menstrual cycle in women of reproductive age. Int J Gynaecol Obstet. 2023;162(3):1086–1090. doi:10.1002/ijgo.14822
- Pourmasumi S, Kounis NG, Naderi M, et al. Effects of COVID-19 infection and vaccination on the female reproductive system: a narrative review. Balkan Med J. 2023;40(3):153–164. doi:10.4274/balkanmedj.galenos.2023.2023-3-4

