Abstract
Importance
The first-trimester anomaly scan (FTAS) has the potential to detect major congenital anomalies in an early stage of pregnancy. Due to this potential early detection, there is a trend to introduce FTAS in regular care. Data regarding the impact of FTAS on the patient’s perspective are limited.
Objective
To provide an overview of the literature assessing the impact of the FTAS on health-related quality of life (HRQoL) and healthcare costs.
Evidence acquisition
Literature search was performed in Embase, PubMed, Medline Ovid, Cochrane Library database, Web-of-Science, and Google Scholar were searched. All studies that reported the performance of a nuchal translucency measurement with a basic fetal assessment HRQoL or healthcare costs of FTAS were included. Studies solely describing screening of chromosomal anomalies were excluded. Three authors independently screened the studies and extracted the data. Results were combined using descriptive analysis. PROSPERO registration number: CRD42016045190.
Results
The search yielded 3242 articles and 16 were included. Thirteen articles (7045 pregnancies) examined the relationship between FTAS and HRQoL. Anxiety scores were raised temporarily before FTAS and returned to early pregnancy baseline following the absence of anomalies. Depression scores did not change significantly as a result of FTAS. Three articles studied healthcare costs. These studies, published before 2005, found a combination of FTAS and second-trimester anomaly scan (STAS) resulted in an increased amount of detected anomalies when compared to a STAS-only regimen. However, the combination would also be more costly.
Conclusions
Women experience anxiety in anticipation of the FTAS result and following a reassuring FTAS result, anxiety returns to the baseline level. FTAS seems to be a reassuring experience. The included studies on costs showed the addition of FTAS is likely to increase the number of detected anomalies against an increase in healthcare costs per pregnancy.
Review registration: PROSPERO CRD42016045190
Introduction
The field of fetal medicine will change following the implementation of the first-trimester anomaly scan (FTAS) due to the timely diagnosis of congenital anomalies or early reassurance of expectant parents. The detection rate varies per anomaly. Some congenital anomalies should always be detected on FTAS, while others cannot be detected. The FTAS is a systematic ultrasound examination of fetal structures between 11 + 0 and 13 + 6 weeks, which can reliably detect severe congenital anomalies (i.e. those that require major surgery or are considered fatal) early in pregnancy, but a second-trimester anomaly scan (STAS) will be required to maximize prenatal detection of anomalies [Citation1]. With a high sensitivity for major congenital anomalies, the focus of the implementation of the FTAS should shift toward the patient’s perspective of this new screening modality. The health-related quality of life (HRQoL) can be used to study the impact of such a screening modality on patient’s lives.
Several indicators of HRQoL can be influenced by the pregnant state or diagnosis of a congenital anomaly [Citation2]. These indicators are psychological, emotional, physical and social functioning, and health perception [Citation3]. Screening of congenital anomalies by FTAS can offer reassurance and relief, whereas the suspicion of a congenital anomaly may cause anxiety and stress.
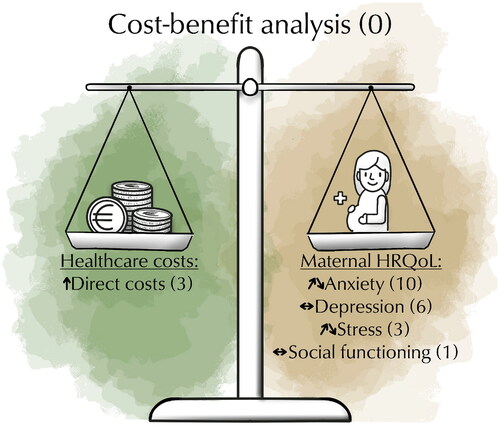
The HRQoL indicators, such as anxiety and depression scores, are important measures of the patient’s perspective on the implementation of the FTAS. Conversely, from a policymaker’s perspective, healthcare costs are important to make informed decisions concerning healthcare budgets. The knowledge on HRQoL indicators can be combined with healthcare costs estimates to perform a cost-benefit analysis (CBA), see also . In preparation for a CBA, an overview of these two important outcome measures, HRQoL and healthcare costs, is essential. However, an overview of both the HRQoL and costs associated with the implementation of the FTAS is missing. Therefore, the aim of this study is to provide a review on HRQoL and healthcare costs associated with the implementation of FTAS for the screening of congenital (non-chromosomal) anomalies.
Figure 1. Overview of parameters involved in cost-effectiveness. Figure shows the impact ↑ (increase)/↓ (decrease)/↔ (no change) of FTAS on the different components of a cost-effectiveness analysis, health-related quality of life (HRQoL) and healthcare costs. The number of studies on the cost-effectiveness analyses, indicators for HRQoL, or healthcare costs are shown in brackets (n).
Methods
The objective was to perform a systematic review of the literature studying HRQoL and healthcare costs associated with the implementation of FTAS for the screening of congenital (non-chromosomal) anomalies in pregnancy. The FTAS as an ultrasound examination is performed to identify structural fetal anomalies (including nuchal translucency measurement) during the first trimester of pregnancy (up to 13 + 6 weeks gestational age).
Prior to undertaking the systematic literature search, the study protocol for the review, describing the strategy of the selection of articles and data extraction, was registered within the PROSPERO Database (ID CRD42016045190). The review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for Scoping Reviews [Citation4]. Patients were not involved in the development of this review as no primary research was conducted. We performed a systematic electronic search with the help of a specialist librarian in the following databases: Embase, PubMed, Medline Ovid, the Cochrane Central Register of Controlled Trials (includes ClinicalTrials.gov), Web-of-Science, and Google Scholar, for articles published until January 29, 2024. The search syntax can be found in Supplemental Table 1.
Inclusion criteria for the articles in the review were:
Performance of a fetal ultrasound scan for a structural assessment or a nuchal translucency measurement with a basic fetal assessment during the first trimester of pregnancy (11+0–13+6 weeks of gestation).
And
The article had to report on indicators of HRQoL (anxiety, depression, stress, social dysfunction, health perception, and coping strategies), or healthcare costs (costs, cost-effectiveness).
HRQoL
During pregnancy, the following health aspects are likely to be impacted by FTAS and were thus considered to reflect maternal HRQoL: anxiety, depression, stress, social functioning, health perception and coping strategies. This review focused on the HRQoL in relation to FTAS and the results of the included articles were interpreted in terms of impact of FTAS on HRQoL.
Healthcare costs
The costs in this study were examined from a healthcare perspective. The healthcare perspective includes all direct costs of healthcare, related but also unrelated to the condition under consideration whereas the societal perspective even includes costs associated with loss of production and patient travel expenses [Citation5]. The costs were converted to euros with the year 2018 as a reference to ensure available healthcare costs of this year.
Exclusion criteria were the following study characteristics: animal studies, conference abstracts, letters, editorials, reviews and non-English articles. Moreover, studies focusing on screening of chromosomal anomalies, small for gestational age fetuses (SGA), miscarriages, hypertensive disorders of pregnancy and genetic tests were also excluded. Finally, studies that performed solely NT measurement for the calculation of risk of aneuploidy but did not perform any form of structural examination in the first trimester were excluded from this review.
The articles identified by the systematic search were screened based on title and abstract by three independent researchers (CP, LM, and KM). After screening of title and abstract, the remaining articles were read in full text, and additionally, references were checked for relevant articles. Key information was collected in a standardized data extraction form and included the following parameters: year of publication, study design, study population, study size, timing of fetal ultrasound examination, measurements and results of cost-effectiveness, maternal HRQoL and costs. Discrepancies between researchers (CP, LM and AM) regarding title/abstract screening, full text reading and data extraction were resolved by discussion, reaching consensus when at least two out of three researchers agreed.
Results
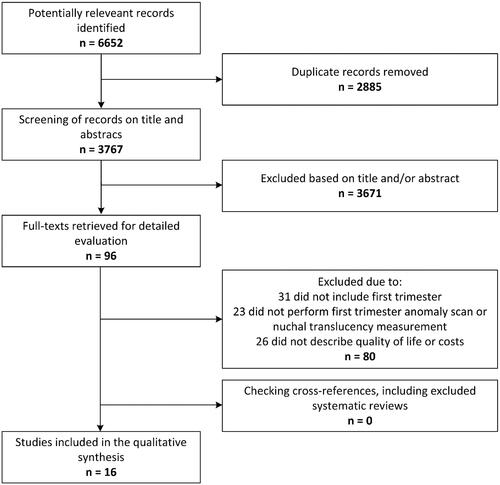
The flowchart () shows the number of identified, unique articles by the search (N = 3767). A total of 96 articles remained after screening of title and abstract. After full text screening, 16 articles were included in the review. Study populations of the included studies consisted of both low-risk and high-risk women for congenital anomalies. Furthermore, these definitions were not well described. Hence, heterogeneity of the study populations precluded pooling of data. Of these 16 articles, 13 reported on HRQoL indicators in a total of 7045 pregnancies.
HRQoL in these articles was expressed as psychological distress (including anxiety and depression), stress, social dysfunction, health perception, and coping strategies. summarizes the findings of the articles reporting on HRQoL. In addition, three articles investigated the costs of predefined healthcare strategies, summarized in . One article included a cohort study with 6634 pregnancies and two articles used hypothetical cohorts. None of the articles in the review discussed cost effectiveness of FTAS in terms of QALYs.
Table 1. Summary of studies on quality of life included in the review.
Table 2. Summary of costing studies included in the review.
HRQoL
Following the qualitative synthesis of the articles investigating HRQoL, we found the following results. Anxiety, as an indicator, was assessed in 10 studies [Citation6–15]. Seven of these studies used the State-Trait Anxiety Inventory (STAI) questionnaire to investigate anxiety in pregnant women in the first trimester [Citation6,Citation7, Citation9–13]. Of these seven studies, four reported on the level of anxiety directly before and after the FTAS [Citation6, Citation11–13]. The remaining three studies used the Hospital Anxiety and Depression Scale (HADS) [Citation8], the General Health Questionnaire (GHQ-22) [Citation15], and a self-designed questionnaire to measure anxiety levels [Citation14].
In five studies, it was found that anxiety levels increased prior to the FTAS. However, following a reassuring scan result (i.e. no anomalies suspected or a normal NT measurement), anxiety was reduced to the early pregnancy baseline level [Citation6,Citation7,Citation9,Citation11,Citation13]. In only one study (Weinans et al.), anxiety was higher after NT measurement compared to control group [Citation14]. A randomized clinical trial by Georgsson Öhman et al. involving 2026 women found no significant difference in anxiety level between those allocated to FTAS and those allocated to a regular second-trimester ultrasound [Citation10]. In the case of the detection of a congenital anomaly during the FTAS, anxiety rose significantly [Citation6]. In case of a suspected anomaly during the FTAS, anxiety would return to the early pregnancy baseline level once the congenital anomaly was disproven at a repeat scan. Only one study (Leithner et al.) found that anxiety was raised after prenatal testing compared to baseline [Citation12]. Brondino et al. and Kaasen et al. found that, in case of suspicion of a congenital anomaly, the levels of anxiety were highest during the decision-making period [Citation8,Citation15].
Depression was examined in six studies [Citation7,Citation8,Citation11,Citation12, Citation15,Citation16]. The two studies by Brondino et al. and Kaasen et al. included women who were referred to a tertiary hospital because of a suspected congenital anomaly at gestational ages ranging from 12 to 38 weeks [Citation8,Citation15]. In both studies, depression scores were higher in the presence of a fetal anomaly. In four other studies, also with a tertiary referral population, no significant difference in depressive symptoms was observed after prenatal testing, including NT measurement, compared to before testing [Citation7,Citation11,Citation12,Citation16]. These studies compared depression scores of women booked for NT measurement to women booked for invasive (genetic) testing. The two studies by Kowalcek et al. also measured stress before and after the NT measurement and found that stress was lower after the NT measurement [Citation11,Citation16]. Leithner et al. found that all women experience acute distress in anticipation of any potential outcome of the FTAS [Citation12].
The study by Kaasen et al. showed that social dysfunction in women with a confirmed congenital anomaly was significantly increased compared to women with no suspicion of anomalies [Citation15]. A survey study by McCoyd examined preparedness for prenatal testing in 659 low-risk women visiting the hospital for NT measurement [Citation17]. 57% of study participants had considered their options in the event of a fetal anomaly and 56% of participants did not expect to find a fetal anomaly. In another study including 991 women opting for NT measurement, 83% of pregnant women found the FTAS to be a reassuring experience [Citation18].
Healthcare costs
summarizes the three studies that examined the costs associated with implementation of FTAS. The studies of Whitlow et al. and Roberts et al. offered a FTAS followed by STAS, and the study by Ritchie et al. offered a first-trimester NT measurement followed by STAS [Citation19–21]. In the study by Whitlow et al. 6634 women, attending a university hospital for obstetric care, were offered the FTAS and STAS [Citation19]. In 1999, the cost of a FTAS was £33 per examination and the costs associated with the detection of anomalies by FTAS were £6.258 per anomaly. In the year 2018, this corresponds with approximately €63 per FTAS examination and €12.001 per anomaly after correction for inflation and conversion to euros (€). The studies by Roberts et al. and Ritchie et al. described a decision analytic model and CBA in a low-risk population for the screening of congenital anomalies by FTAS and/or STAS. In the CBA by Roberts et al. a combined strategy of FTAS and STAS would detect the highest number of congenital anomalies against higher costs when compared to STAS-only, i.e. an increase of £20-149 (1996) or €42-310 (2018) [Citation20]. The costs of FTAS in the study by Roberts et al. were estimated at £20 (1996) or €42 (2018) per pregnancy [Citation20]. The second decision analytic model by Ritchie et al. found that the combined strategy of FTAS and STAS would detect an additional eight anomalies per 10,000 pregnancies (59 vs 67 detected congenital anomalies per 10,000 pregnancies) compared to STAS only. This represents an increment in the detection rate of 13.6%. The combined strategy would increase the costs by £20 (2005) or €33 (2018) per pregnancy [Citation21]. These studies did not include the healthcare costs of children diagnosed with congenital anomalies.
Discussion
Main findings
This review shows that women experience a temporary increase in anxiety levels in anticipation of the FTAS result and these anxiety levels return to their initial state following a reassuring result of the FTAS. Depression tends not to change following FTAS. In case of a normal result of the FTAS, the additional ultrasound examination provided reassurance and relief to women. Adding FTAS to the routine screening program for congenital anomalies would increase both the number of detected congenital anomalies as well as the costs per pregnancy.
Strengths and limitations
The strength of this review is that most of the included articles had large sample sizes between 180 and 50,000 pregnant women. Second, of the included articles investigating the maternal quality of life in 11 (out of 13) validated questionnaires for HRQoL indicators were used, such as the State-Trait Anxiety Inventory (STAI), General Health Questionnaire (GHQ) and the Impact of Events Scale (IES). Unfortunately, most of these questionnaires are not specific for or validated for use in pregnancy. Only the Edinburgh Postnatal Depression Scale (EPDS) and STAI have been validated [Citation22,Citation23].
There are several limitations of this study. First, only articles describing cost-effectiveness based on costs and detected anomalies, rather than QALYs, of the FTAS could be included, and these were published before 2005. Lack of recent studies can be considered a limitation, questioning the applicability of the findings for current clinical practice, as both costs and sensitivity of the equipment have changed over time. For example, in their model, Roberts et al. consider a sensitivity of FTAS of 0% for the detection of cardiac defects [Citation20,Citation24]. Karim et al. who published a meta-analysis in 2022, have found a sensitivity of 55.8% for the detection of major cardiac anomalies in the first trimester. Additionally, only 16 articles are included in this review. It was possible to broaden the search by including articles investigating the second trimester or chromosomal anomalies, but this would have changed the scope of the review. Finally, the studies included in our review describe a heterogeneous population of low- and high-risk pregnancies for congenital anomalies, which hampers easy comparison and interpretation of our results. It is likely that women with a previous history of a child with a congenital anomaly experience more anxiety when compared to women without such history or awareness of these anomalies. A normal FTAS result in the high-risk group could therefore cause a greater reduction of (anticipated) anxiety.
Interpretation
Our results suggest that anxiety and stress levels return to baseline, initial levels after a transient increase associated with the FTAS, particularly in cases where a reassuring result is obtained. Like the STAS, in case of the detection of a congenital anomaly following FTAS, levels of anxiety, depression, and stress rise to a level comparable to the level of a major depressive period [Citation12,Citation25]. Our findings with anxiety are in line with a study that investigated anxiety in association with noninvasive prenatal testing (NIPT) for aneuploidy in the first trimester. At intake, before the test results were known, women felt more anxious compared to the moment they had received their test result [Citation26]. However, women with an abnormal NIPT result had higher anxiety levels after they had received the result. A detected anomaly will inevitably cause anxiety and stress, whereas a reassuring result of the FTAS will return anxiety to baseline levels. Finally, unlike a STAS-only regimen, women with a normal result of both FTAS and STAS will experience a longer period of relative reassurance.
The psychological stress of a pregnancy termination increases as pregnancy progresses, most likely due to feeling of fetal movements [Citation15,Citation27–30]. Decisions made following a diagnosis in the first trimester may, therefore, be less emotionally damaging than those made later in pregnancy. At the end of the first trimester, the risk of spontaneous miscarriage is low, the probability of a false positive result from FTAS is low, and the congenital anomalies detected by FTAS are likely to be serious [Citation1,Citation31]. Furthermore, if a miscarriage does occur, parents may be informed of a possible cause of the pregnancy loss, providing some measure of relief and information regarding their future reproductive perspectives. Therefore, early diagnosis of congenital anomalies may have multiple potential advantages.
The article by Ritchie et al. found that the combined screening strategy of FTAS followed by STAS will detect more congenital anomalies [Citation21]. An increased nuchal translucency or hygroma colli is associated with structural heart defects as well as chromosomal abnormalities. Awareness of such a risk factor of anomalies should prompt second-trimester echocardiography and increased vigilance in detecting anomalies. Furthermore, a transvaginal ultrasound in the increasingly obese pregnant population can improve visualization of the fetus and detection of congenital anomalies [Citation32]. Finally, by screening twice, it is more likely that a congenital anomaly will be identified.
The indicators for maternal HRQoL can be combined with healthcare costs to perform a CBA. Typically, the results of the CBA are expressed as quality-adjusted life years (QALY) [Citation33]. QALYs provide a uniform quantity of effect and duration of effect and are essential to compare different screening strategies. In a CBA, the (additional) costs due to the implementation of FTAS could be compared to the potential benefits, such as reduction in levels of anxiety. The included studies on the costs of FTAS and STAS estimated that the healthcare costs would increase with €33–310 per pregnancy. Further, decision-making using CBA requires choosing a cutoff value for the maximum acceptable cost per QALY, also described as the willingness to pay (WTP) [Citation34]. In particular, the WTP can be used to compare the value of FTAS to other health interventions. In a 1985 study, the WTP for diagnostic obstetric ultrasound was estimated at $1217, which would translate to €2400 in 2018 [Citation35]. This is starkly different from the WTP for the NIPT, which is calculated at €169 [Citation36]. With costs of FTAS lower than those of the NIPT and the potential to screen for multiple structural anomalies, early detection of anomalies by FTAS may easily outweigh the extra costs associated with the ultrasound examinations.
We show that knowledge on maternal HRQoL and healthcare costs of FTAS is limited. The implementation of FTAS into obstetrical clinical care should be preceded by extensive research on the impact of maternal quality of life. Subsequently, a cost-effectiveness analysis of this new screening modality should be attempted with maternal QALY as outcome. Future studies should focus on the impact of FTAS on anxiety and depression throughout pregnancy in a screening strategy including FTAS. Specifically, anxiety and depression are emotions affected by prenatal diagnosis of congenital anomalies and are important indicators of HRQoL. Understanding the impact of FTAS on levels of anxiety and depression throughout pregnancy is of value for optimization of the clinical decision-making process and psychological support especially for those women with abnormal FTAS results. Furthermore, it will enable healthcare providers and policymakers to better assess the cost-effectiveness of FTAS and to compare this new diagnostic modality to other health interventions.
Conclusion
In conclusion, women experience anxiety before a first-trimester ultrasound examination, with a relief in anxiety following a normal result. Furthermore, depression scores will return to early pregnancy levels following a normal result. Maternal HRQoL seems to be temporarily lowered in case an anomaly is detected. Implementation of FTAS may increase the number of detected anomalies with a concomitant increase in healthcare costs. Overall, while there is limited literature concerning the implementation of the first-trimester anomaly scan, further research may elucidate the impact on health-related quality of life.
Author contributions
CSP, MR, EAPS and AGMGJM conceived and planned the study. CSP, LM and AGMGJM performed data extraction and quality analysis. All authors commented and provided feedback on and approved the final version for publication.
Ethical approval
None.
Supplemental Material
Download MS Word (24.5 KB)Acknowledgments
The authors wish to thank Wichor Bramer and Eline Krabbendam from the Erasmus MC Medical Library for developing and updating the search strategies. Furthermore, the authors wish to thank Kajal Mohabier for her help with the screening of articles.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Karim JN, Roberts NW, Salomon LJ, et al. Systematic review of first-trimester ultrasound screening for detection of fetal structural anomalies and factors that affect screening performance. Ultrasound Obstet Gynecol. 2017;50(4):1–11. doi:10.1002/uog.17246
- Haraldstad K, Wahl A, Andenæs R, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. 2019;28(10):2641–2650. doi:10.1007/s11136-019-02214-9
- Gregory MRB, Prouhet PM, Russell CL, et al. Quality of life for parents of children with congenital heart defect: a systematic review. J Cardiovasc Nurs. 2018;33(4):363–371. doi:10.1097/JCN.0000000000000466
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi:10.7326/M18-0850
- Garrison LP, Jr., Pauly MV, Willke RJ, et al. An overview of value, perspective, and decision Context-A health economics approach: an ISPOR special task force report [2]. Value Health. 2018;21(2):124–130. doi:10.1016/j.jval.2017.12.006
- Bardi F, Bakker M, Kenkhuis MJA, et al. Psychological outcomes, knowledge and preferences of pregnant women on first-trimester screening for fetal structural abnormalities: a prospective cohort study. PLoS One. 2021;16(1):e0245938. doi:10.1371/journal.pone.0245938
- Beck V, Opdekamp S, Enzlin P, et al. Psychosocial aspects of invasive fetal therapy as compared to prenatal diagnosis and risk assessment. Prenat Diagn. 2013;33(4):334–340. doi:10.1002/pd.4073
- Brondino N, Colombini G, Morandotti N, et al. Psychological correlates of decision-making during prenatal diagnosis: a prospective study. J Psychosom Obstet Gynaecol. 2013;34(2):68–74. doi:10.3109/0167482X.2013.797404
- Chueh HY, Cheng PJ, Shaw SW, et al. Maternal anxiety about first trimester nuchal translucency screening and impact of positive screening results. Acta Obstet Gynecol Scand. 2007;86(12):1437–1441. doi:10.1080/00016340701622724
- Georgsson Ohman S, Saltvedt S, Grunewald C, et al. Does fetal screening affect women’s worries about the health of their baby? A randomized controlled trial of ultrasound screening for down’s syndrome versus routine ultrasound screening. Acta Obstet Gynecol Scand. 2004; 83(7):634–640. doi:10.1111/j.0001-6349.2004.00462.x
- Kowalcek I, Huber G, Bieniakiewitz I, et al. The influence of gestational age on depressive reactions, stress and anxiety of pregnant women and their partners in relation to prenatal diagnosis. J Psychosom Obstet Gynaecol. 2003;24(4):239–245. doi:10.3109/01674820309074688
- Leithner K, Maar A, Fischer-Kern M, et al. Affective state of women following a prenatal diagnosis: predictors of a negative psychological outcome. Ultrasound Obstet Gynecol. 2004;23(3):240–246. doi:10.1002/uog.978
- Simó S, Zúñiga L, Izquierdo MT, et al. Effects of ultrasound on anxiety and psychosocial adaptation to pregnancy. Arch Womens Ment Health. 2019;22(4):511–518. doi:10.1007/s00737-018-0918-y
- Weinans MJN, Kooij L, Müller MA, et al. A comparison of the impact of screen-positive results obtained from ultrasound and biochemical screening for down syndrome in the first trimester: a pilot study. Prenat Diagn. 2004;24(5):347–351. doi:10.1002/pd.872
- Kaasen A, Helbig A, Malt UF, et al. Acute maternal social dysfunction, health perception and psychological distress after ultrasonographic detection of a fetal structural anomaly. BJOG. 2010;117(9):1127–1138. doi:10.1111/j.1471-0528.2010.02622.x
- Kowalcek I, Mühlhoff A, Bachmann S, et al. Depressive reactions and stress related to prenatal medicine procedures. Ultrasound Obstet Gynecol. 2002;19(1):18–23. doi:10.1046/j.0960-7692.2001.00551.x
- McCoyd JL. Preparation for prenatal decision-making: a baseline of knowledge and reflection in women participating in prenatal screening. J Psychosom Obstet Gynaecol. 2013;34(1):3–8. doi:10.3109/0167482X.2012.757590
- Drysdale K, Ridley D, Walker K, et al. First-trimester pregnancy scanning as a screening tool for high-risk and abnormal pregnancies in a district, general hospital setting. J Obstet Gynaecol. 2002;22(2):159–165. doi:10.1080/01443610120113300
- Whitlow BJ, Chatzipapas IK, Lazanakis ML, et al. The value of sonography in early pregnancy for the detection of fetal abnormalities in an unselected population. Br J Obstet Gynaecol. 1999;106(9):929–936. doi:10.1111/j.1471-0528.1999.tb08432.x
- Roberts T, Mugford M, Piercy J. Choosing options for ultrasound screening in pregnancy and comparing cost effectiveness: a decision analysis approach. Br J Obstet Gynaecol. 1998;105(9):960–970. doi:10.1111/j.1471-0528.1998.tb10258.x
- Ritchie K, Bradbury I, Slattery J, et al. Economic modelling of antenatal screening and ultrasound scanning programmes for identification of fetal abnormalities. BJOG. 2005;112(7):866–874. doi:10.1111/j.1471-0528.2005.00560.x
- Murray D, Cox JL. Screening for depression during pregnancy with the edinburgh depression scale (EDDS). J Reprod Infant Psychol. 1990;8(2):99–107. 1990/04/01doi:10.1080/02646839008403615
- van der Bij AK, de Weerd S, Cikot RJ, et al. Validation of the dutch short form of the state scale of the Spielberger State-Trait Anxiety Inventory: considerations for usage in screening outcomes. Community Genet. 2003;6(2):84–87. doi:10.1159/000073003
- Karim JN, Bradburn E, Roberts N, study A., et al. First-trimester ultrasound detection of fetal heart anomalies: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2022;59(1):11–25. doi:10.1002/uog.23740
- Ekelin M, Crang Svalenius E, Larsson AK, et al. Parental expectations, experiences and reactions, sense of coherence and grade of anxiety related to routine ultrasound examination with normal findings during pregnancy. Prenat Diagn. 2009;29(10):952–959. doi:10.1002/pd.2324
- van Schendel RV, Page-Christiaens G, Beulen L, et al. Women’s experience with non-invasive prenatal testing and emotional well-being and satisfaction after test-results. J Genet Couns. 2017;26(6):1348–1356. doi:10.1007/s10897-017-0118-3
- Korenromp MJ, Christiaens GC, van den Bout J, et al. Long-term psychological consequences of pregnancy termination for fetal abnormality: a cross-sectional study. Prenat Diagn. 2005;25(3):253–260. doi:10.1002/pd.1127
- Korenromp MJ, Page-Christiaens GC, van den Bout J, et al. A prospective study on parental coping 4 months after termination of pregnancy for fetal anomalies. Prenat Diagn. 2007;27(8):709–716. doi:10.1002/pd.1763
- Alhusen JL. A literature update on maternal-fetal attachment. J Obstet Gynecol Neonatal Nurs. 2008;37(3):315–328. doi:10.1111/j.1552-6909.2008.00241.x
- Salisbury A, Law K, LaGasse L, et al. Maternal-fetal attachment. JAMA. 2003;289(13):1701. doi:10.1001/jama.289.13.1701
- Ammon Avalos L, Galindo C, Li DK. A systematic review to calculate background miscarriage rates using life table analysis. Birth Defects Res A Clin Mol Teratol. 2012; 94(6):417–423. doi:10.1002/bdra.23014
- Cullen MT, Green JJ, Reece EA, et al. A comparison of transvaginal and abdominal ultrasound in visualizing the first trimester conceptus. J Ultrasound Med. 1989; 8(10):565–569. doi:10.7863/jum.1989.8.10.565
- Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003;1(1):80. doi:10.1186/1477-7525-1-80
- Phelps CE. A new method to determine the optimal willingness to pay in cost-effectiveness analysis. Value Health. 2019;22(7):785–791. doi:10.1016/j.jval.2019.03.003
- Berwick DM, Weinstein MC. What do patients value? Willingness to pay for ultrasound in normal pregnancy. Med Care. 1985;23(7):881–893. doi:10.1097/00005650-198507000-00005
- Verweij EJ, Oepkes D, de Vries M, et al. Non-invasive prenatal screening for trisomy 21: what women want and are willing to pay. Patient Educ Couns. 2013; 93(3):641–645. doi:10.1016/j.pec.2013.08.006