ABSTRACT
Purpose
In oculoplastic surgery the eyelid tissue is frequently stretched in order to repair defects after tumor surgery. However, there is a paucity of research regarding how stretching affects eyelids. The purpose of this study was to gain insight into how traction force affects eyelid stretch as well as tissue perfusion, using a laser-based in vivo monitoring technique.
Method
Lower-lid pentagonal resections were performed in eight patients and a total of nine eyelids. The medial section of the eyelid was then stretched using a dynamometer up to a force of 2.3 Newtons (N), and eyelid stretching and blood perfusion were continuously measured using laser speckle contrast imaging.
Results
Tissue perfusion decreased exponentially when eyelid tissue was stretched, with an initial sharp decline followed by a more gradual reduction. Perfusion approached zero at a force of approximately 2.0 N. The length of the eyelid increased with increasing force up to 1.5 N, after which there was only a very slight increase in length.
Conclusions
Eyelid tissue seems to respond to traction in a non-linear fashion, where the initial force results in the greatest eyelid stretching and reduction in blood perfusion. The results provide information on the effects of a large force for direct closure of large eyelid defects. Considering how quickly perfusion approaches zero, the high success rate of eyelid reconstruction surgery is likely a testament to the extensive vascularization of the periocular region.
Introduction
The excision of periocular tumors results in a tissue deficiency that needs to be addressed. There are four main surgical options for repairing defects in the periocular region: direct closure, grafts, flaps, and laissez-faire.Citation1–3 Traditionally, the direct closure of lid defects has been restricted to wounds less than or equal to one-fourth of the lid, or up to one-third in elderly patients with increased lid laxity.Citation1 However, recent studies have shown that significantly larger defects on the lower eyelid can be closed directly with excellent postoperative results, even when extreme traction force is used, resulting in palpebral aperture distortion or partial wound dehiscence.Citation4,Citation5 Similarly, evidence from plastic surgery literature involving tissue expanders supports the same concept.Citation6 In standard practice, canthotomy is often carried out in order to mobilize extra tissue when direct closure of a lid defect is deemed to require too great a force. However, this reduces the traction and thereby decreases the potential of the globe to act as an expander, and the authors therefore recommended that canthotomy be avoided. In addition, it has been demonstrated that canthotomy combined with wedge resection may have a detrimental effect on blood perfusion.Citation7 Increased traction can be utilized in laissez-faire by employing guiding sutures to provide stretching and speed up healing.Citation8 A deeper understanding of the traction properties of eyelid tissue would help determine when direct closure might be a suitable option, and would be helpful in the design of grafts and flaps for eyelid reconstruction.
The periocular region is recognized for its excellent healing capabilities due to its rich vascular supply. It has been shown that avascular grafts and flaps that are stretched to a point where perfusion would be expected to be zero,Citation9 still have a high survival rate. Indeed, even flaps showing postoperative discoloration can often be quickly reperfused.Citation10 Nonetheless, understanding how the surgical approach affects perfusion is important in ensuring the optimal postoperative outcome.
Laser speckle contrast imaging (LSCI) is a non-invasive tool that has been used to study perfusion in plastic surgery. The area of interest is illuminated with laser light, and the backscattered light forms a random interference pattern called a speckle pattern. This pattern is affected by the movement of red blood cells, and microvascular perfusion can thus be monitored.Citation11–13 Previous studies have been performed using LSCI to evaluate blood perfusion during reconstruction with eyelid flaps, such as glabellar flaps, Hughes flaps, and advancement flaps, showing that stretching as well as rotation affect tissue perfusion.Citation9,Citation14–18 However, no study has yet been performed on the effects of high traction forces used in the closure of eyelid defects on perfusion.
The purpose of this study was to determine the effect of traction force on blood perfusion and stretching of the eyelid. The study was performed on eight patients undergoing pentagonal resection in conjunction with entropion repair, in which the eyelid was gradually stretched while the traction was measured using a dynamometer, and perfusion was measured using LSCI. The results provide valuable insight into the relation between traction force and perfusion in eyelid surgery, providing surgeons with valuable information on the direct closure of large eyelid defects.
Methods
Ethics
The experimental protocol for this study was approved by the Ethics Committee at the Swedish Ethical Review Authority, Sweden. The research adhered to the tenets of the Declaration of Helsinki as amended in 2013. All patients included in the study gave their full informed written consent.
Subjects
Lower-lid pentagonal resections were performed as part of entropion repair using the Quickert procedure.Citation15 Patients undergoing surgery at the Department of Ophthalmology, Skåne University Hospital, during the months of January through March 2023 were included in the study. Exclusion criteria were the inability to give informed consent, or to cooperate, due to mental or physical factors, during the procedure, which was performed under local anesthesia. One patient was excluded due to advanced dementia. Furthermore, data from one patient were excluded due to malfunctioning of the equipment, and the data from another patient were deemed unphysiological. In total, eleven patients were recruited and eight were included, whereof nine eyelids were studied. The characteristics of the patients are presented in .
Table 1. Patient characteristics.
Surgical procedure
An adjusted Quickert procedure was performed under local infiltration anesthesia with 20 mg/ml lidocaine (Xylocaine®, AstraZeneca, Södertälje, Sweden). A pentagonal resection was made approximately 5 mm from the lateral canthus. The excision was made of enough horizontal length in order to obtain adequate tightening of the eyelid, to remedy the excess laxity and the cause of entropion. Thereafter, the study protocol was undertaken (as described below). This was done before creating flaps to mimic tumor excision as closely as possible. After completion of the study protocol, the Quickert procedure was completed according to normal practice.
Study protocol
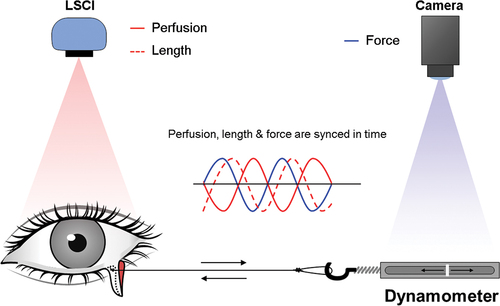
Following pentagonal resection, a mark was made at the medial canthus. A suture (4–0 Sofsilk, Covidien, Mansfield, MA, USA) was placed on the medial side of the eyelid defect and connected to a dynamometer (FK50, Vetek AB, Väddö, Sweden). Using a dynamometer, the eyelid was then pulled laterally to create a horizontal traction force, resulting in stretching of the eyelid, using a steadily increasing force up to a maximum of 2.3 Newtons (N). Eyelid perfusion and the length of stretching was measured using LSCI, while a regular camera simultaneously captured the applied force from the dynamometer. This enabled us to measure eyelid stretching and perfusion in relation to the applied traction force. The study setup is illustrated in .
Figure 1. Schematic illustration of the study protocol. A lower-lid pentagonal resection was made as part of an entropion repair procedure. A suture was placed on the medial side of the eyelid defect and connected to a dynamometer. The eyelid was then pulled laterally to create a horizontal traction force, resulting in stretching of the eyelid, using a steadily increasing force up to a maximum of 2.3 N. The procedure was filmed and eyelid perfusion was monitored with LSCI.
Laser speckle contrast imaging
Blood perfusion was measured using LSCI (PeriCam PSI NR with Zoom System, with Zoom HR, Perimed AB, Stockholm, Sweden). This system employs an infrared 785 nm laser beam that is spread over the surface of the skin by a diffuser. The reflected light creates a speckle pattern (dark and bright areas formed by random interference of the light backscattered from the illuminated area). Blood perfusion is calculated automatically by the system, by analyzing variations in the speckle pattern. The speckle pattern is recorded in real time, at a rate of up to 100 images per second, with a high resolution of up to 100 μm/pixel. It is well known that skin perfusion is affected by cardiovascular status and room temperature. The room temperature was therefore maintained at 20°C.
A limitation of LSCI in the measurement of perfusion is that it is hampered by movement artifacts, as tissue movement may be interpreted as perfusion. To assess the effect of mechanical stretching of the eyelid on the LSCI signal, experiments were performed on skin excised in conjunction with blepharoplasty, from four eyelids. These experiments were performed ex vivo, thus in the absence of blood perfusion.
Calculations and statistics
Eyelid stretch was calculated as a percentage of the eyelid length, from the medial canthus to the surgical defect. The blood perfusion is given in arbitrary units (perfusion units, PU). The results from each eyelid were normalized to the perfusion before stretching (defined as 100%) to account for variations in perfusion between the subjects. Perfusion measurements were started at an initial force exertion of 0.2 N, to ensure that the setup was stable. The changes in eyelid length and perfusion were analyzed using nonlinear regression with one-phase decay. Calculations and statistical analysis were performed using GraphPad Prism7.0a (GraphPad Software Inc., San Diego, CA, USA).
Results
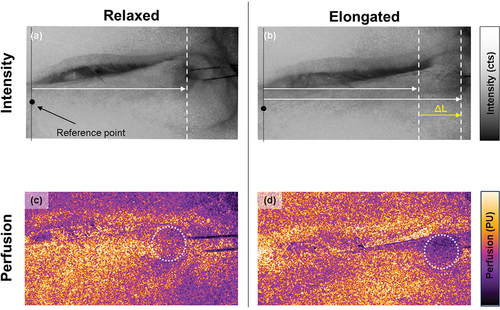
Applying a horizontal traction force to the eyelid resulted in stretching and a reduction in blood perfusion, as illustrated in the representative example in .
Figure 2. Representative example of intensity maps showing eyelid stretching (top) and perfusion maps (bottom) from a left lower eyelid with a pentagonal resection before and after the application of a horizontal force. Eyelid stretching (ΔL) was calculated as a percentage of the total eyelid length, from a reference point at the medial canthus. Perfusion was measured in a region of interest (dashed circle), close to the pentagonal resection, and expressed as a percent of the initial value in the relaxed eyelid. Note the decrease in perfusion (d) when the eyelid is elongated by the traction force.
Eyelid stretching due to the traction force was non-linear (). The length of the eyelid increased with increasing force up to 1.5 N, after which there was only a very slight increase in length. Despite the fact that the distance from the medial canthus to the surgical defect was similar in the patients, the maximum length to which the eyelid was extended varied considerably, suggesting a large interindividual variation in tissue laxity.
Figure 3. Eyelid stretching and blood perfusion in relation to traction force. Stretching was measured from a reference point at the medial canthus to the pentagonal resection. Blood perfusion is expressed as a percentage of the value before traction (100%). Nonlinear regression with one-phase decay was performed to describe the change in stretch and perfusion with increasing force.
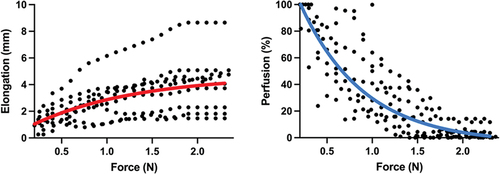
The perfusion also decreased in a non-linear fashion as the eyelids were subjected to increasing traction force (). Perfusion approached zero at a traction force of approximately 2.0 N.
To determine whether mechanical tissue movement had any significant effect on the perfusion measured with LSCI, skin excised during upper-lid blepharoplasty was investigated with LSCI ex vivo. The results showed a substantial increase in the signal over the entire tissue sample while stretching, which is entirely motion-induced as no perfusion is expected. This is the opposite of the response seen in vivo, indicating that signal artifacts from tissue movement on the LSCI signal had little impact on the results from the present study.
All eyelids healed well and the surgical outcome was excellent in all cases.
Discussion
Understanding the mechanobiology of tissue and its perfusion in response to manipulation may be valuable in wound closure after tumor excision. The results of the present study demonstrate that eyelids readily stretch in response to traction force. However, above a force of 1.5 N, stretching decreased significantly, suggesting that 1.5 N is close to the limit of horizontal force that can be applied to eyelid tissue. In addition, the exponential manner in which the tissue stretches is in line with previous findings that the stress-strain curve of the skin is governed by its structure, and the order in which extracellular matrix molecules are engaged, first elastin and then collagen.Citation19,Citation20
The stretching potential of eyelid tissue may be important for the design of eyelid flaps and grafts, as well as in determining whether direct closure is a viable option. However, there is considerable interindividual variability in eyelid laxity. Several factors may contribute to this variability, including age, sun exposure, smoking, genetics, and body mass index.Citation21 The median age was 72 years in the present study. Collagen degradation and elastosis are hallmarks of aging, and have been suggested as significant contributory factors in the development of entropion and ectropion.Citation22 The results would thus probably have been different in a younger age group. However, most patients undergoing reconstructive eyelid surgery are elderly, and the findings of this study are thus relevant in the clinical context.
Another aspect to take into account is that the size of the defect that can be closed is not only dependent on the laxity of the eyelid and canthal ligaments, but also the fact that normally the eyelid is curved to enclose the eye. When large defects are closed by primary intention, the eyelid is tightened, and the globe is luxated upwards. This provides additional opportunity to close large eyelid defects. Tissue expansion during healing restores the anatomy and original position of the globe. However, care must be taken to not overtightening the lid since it may result in lid retraction and risk exposure.
An important aspect, not addressed in this study, is the response of tissue to prolonged stretching. Indeed, stretching eyelid tissue with extreme forces, such that the eyelid aperture is deformed, meaning that the patient cannot open their eye postoperatively, will eventually result in an extension of the eyelid tissue and a reduction of traction.Citation4 The short- and long-term mechanobiological effects are the result of several factors, including changes and realignment in the architecture of the main extracellular matrix proteins and activation of intracellular signaling pathways, including mechanosensitive ion channels and integrin-molecules.Citation19 Studying these long-term effects of eyelid stretching may be an important target of future studies.
Previous studies have shown that the perfusion of eyelid flaps is dependent on the length of the flap, with perfusion decreasing gradually from the base to the tip, and that stretching and rotation can decrease flap perfusion.Citation9,Citation14–18,Citation23,Citation24 The present study reinforces these previous findings and demonstrates that traction force reduces tissue perfusion, with values at or approaching zero at a force of 2 N. A decrease in perfusion may be detrimental in terms of healing and postoperative results. However, the high survival rate of eyelid flaps and favorable outcomes following extensive stretching in direct closure suggest that there is rapid postoperative reperfusion. It can be speculated that stretching causes the narrowing of blood vessels without causing lasting damage, and that the vessels quickly reopen once the tissue adapts to stretching. Once attached, the traction forces should result in the recruitment of surrounding tissue and a redistribution of force, which might facilitate reperfusion. It would be of interest to study the immediate postoperative period to determine how rapidly the tissue is reperfused, and whether the degree of stretching affects reperfusion.
LSCI measures movement in the tissue, which is then interpreted as perfusion. Therefore, movement created by stretching of the eyelid may have affected the LSCI signal in the present study. However, the results of the ex vivo experiments, conducted on excised skin from upper lid blepharoplasty, in the absence of blood perfusion, suggest that this this effect was minimal. Indeed, mechanical movement increased the LSCI signal, which, if anything, would counteract the effect of decreased perfusion due to stretching. Movement caused by stretching the eyelid thus had no impact on the conclusions drawn in the present study.
In conclusion, this study demonstrates the effect of traction force on stretching and blood perfusion in eyelids. The results showed that eyelid stretching reached a plateau at a force of approximately 1.5 N, but there was considerable interindividual variability. It is therefore difficult to give a general recommendation on the degree of acceptable eyelid stretching, and this must be determined perioperatively on a case-by-case basis. We have also shown that the perfusion approaches zero when the tissue is stretched to a maximum at a force of about 2 N. Increased knowledge on the amount of traction that can be applied to an eyelid without detrimental effects on perfusion will hopefully pave the way for primary closure of large eyelid defects, as well as laissez-faire procedures using guiding sutures with high traction.
Acknowledgements
The authors express their gratitude to John Albinsson for his assistance during the measurements, and to the surgical staff involved at Skåne University Hospital.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Additional information
Funding
References
- Codner MA, McCord CD, Mejia JD, Lalonde D. Upper and lower eyelid reconstruction. Plast Reconst Surg. 2010;126(5):231e–245e. doi: 10.1097/PRS.0b013e3181eff70e.
- Morton J. Secondary intention healing in lower eyelid reconstruction–a valuable treatment option. J Plast Reconstr Aesthet Surg. 2010;63(11):1921–1925. doi: 10.1016/j.bjps.2010.03.005.
- Shafi F, Rathore D, Johnson A, Mehta P, Ahluwalia HS. Medial canthal defects following tumour excision: to reconstruct or not to reconstruct? Orbit. 2017;36(2):64–68. doi: 10.1080/01676830.2017.1279654.
- Thaller VT, Madge SN, Chan W, Vujic I, Jazayeri F. Direct eyelid defect closure: a prospective study of functional and aesthetic outcomes. Eye (Lond). 2019;33(9):1393–1401. doi: 10.1038/s41433-019-0414-2.
- Vahdani K, Thaller VT. Re: “The effect of canthotomy on blood perfusion during the repair of lower eyelid defects”. Ophthal Plast Reconstr Surg. 2020;36(4):422–423. doi: 10.1097/IOP.0000000000001684.
- Buchanan PJ, Kung TA, Cederna PS. Evidence-based medicine: wound closure. Plast Reconstr Surg. Dec, 2014;134(6):1391–1404. doi: 10.1097/PRS.0000000000000720.
- Berggren JV, Tenland K, Memarzadeh K, Sheikh R, Hult J, Lindstedt S, et al. The effect of canthotomy on blood perfusion during the repair of lower eyelid defects. Ophthalmic Plast Reconstr Surg. 2020;36(2):135–138. doi: 10.1097/IOP.0000000000001489.
- DaCosta J, Oworu O, Jones CA. Laissez-faire: how far can you go? Orbit. 2009;28(1):12–15. doi: 10.1080/01676830802417510.
- Tenland K, Berggren JV, Dybelius Ansson C, Hult J, Dahlstrand U, Lindstedt S, et al. Blood perfusion in rotational full-thickness lower eyelid flaps measured by laser speckle contrast imaging. Ophthalmic Plast Reconstr Surg. 2020;36(2):148–151. doi: 10.1097/IOP.0000000000001496.
- Tyers AGCJ. Colour Atlas of Ophthalmic Plastic Surgery E-Book. 4th ed. PA: Elsevier Inc; 2017.
- Zotterman J, Bergkvist M, Iredahl F, Tesselaar E, Farnebo S. Monitoring of partial and full venous outflow obstruction in a porcine flap model using laser speckle contrast imaging. J Plast Reconstr Aesthet Surg. 2016;69(7):936–943. doi: 10.1016/j.bjps.2016.02.015.
- Yamamoto Y, Ohura T, Nohira K, Sugihara T, Minakawa H, Igawa H, et al. Laserflowgraphy: a new visual blood flow meter utilizing a dynamic laser speckle effect. Plast Reconstr Surg. 1993;91(5):884–894. doi: 10.1097/00006534-199304001-00022.
- Allen J, Howell K. Microvascular imaging: techniques and opportunities for clinical physiological measurements. Physiol Meas. 2014;35(7):R91–R141. doi: 10.1088/0967-3334/35/7/R91.
- Nguyen CD, Sheikh R, Dahlstrand U, Lindstedt S, Malmsjo M. Investigation of blood perfusion by laser speckle contrast imaging in stretched and rotated skin flaps in a porcine model. J Plast Reconstr Aesthet Surg. 2018;71(4):611–613. doi: 10.1016/j.bjps.2017.08.030.
- Nguyen CD, Hult J, Sheikh R, Tenland K, Dahlstrand U, Lindstedt S, et al. Blood perfusion in human eyelid skin flaps examined by laser speckle contrast imaging-importance of flap length and the use of diathermy. Ophthalmic Plast Reconstr Surg. 2018;34(4):361–365. doi: 10.1097/IOP.0000000000001010.
- Berggren JV, Tenland K, Sheikh R, Hult J, Engelsberg K, Lindstedt S, et al. Laser speckle contrast imaging of the blood perfusion in glabellar flaps used to repair medial canthal defects. Ophthalmic Plast Reconstr Surg. 2022;38(3):274–279. doi: 10.1097/IOP.0000000000002082.
- Tenland K, Memarzadeh K, Berggren J, Nguyen CD, Dahlstrand U, Hult J, et al. Perfusion monitoring shows minimal blood flow from the flap pedicle to the tarsoconjunctival flap. Ophthalmic Plast Reconstr Surg. 2019;35(4):346–349. doi: 10.1097/IOP.0000000000001250.
- Sheikh R, Memarzadeh K, Torbrand C, Blohme J, Lindstedt S, Malmsjo M. Blood Perfusion in a full-thickness eyelid flap, investigated by laser doppler velocimetry, laser speckle contrast imaging, and thermography. Eplasty. 2018;18:e9.
- Silver FH, Siperko LM, Seehra GP. Mechanobiology of force transduction in dermal tissue. Skin Res Technol. 2003;9(1):3–23. doi: 10.1034/j.1600-0846.2003.00358.x.
- Pullen R, Konrad J, Merkel R, Hoffmann B. Skin under strain: from epithelial model tissues to adult epithelia. Cells. 2021;10(7):1834. doi: 10.3390/cells10071834.
- Jacobs LC, Liu F, Bleyen I, Gunn DA, Hofman A, Klaver CC, et al. Intrinsic and extrinsic risk factors for sagging eyelids. JAMA Dermatol. 2014;150(8):836–843. doi: 10.1001/jamadermatol.2014.27.
- Kocaoglu FA, Katircioglu YA, Tok OY, Pulat H, Ornek F. The histopathology of involutional ectropion and entropion. Can J Ophthalmol. 2009;44(6):677–679. doi: 10.3129/i09-152.
- Memarzadeh K, Sheikh R, Blohme J, Torbrand C, Malmsjo M. Perfusion and oxygenation of random advancement skin flaps depend more on the length and thickness of the flap than on the width to length ratio. Eplasty. 2016;16:e12.
- Berggren JV, Sheikh R, Hult J, Engelsberg K, Malmsjo M. Laser speckle contrast imaging of a rotational full-thickness lower eyelid flap shows satisfactory blood perfusion. Ophthalmic Plast Reconstr Surg. 2021;37(4):e139–e41. doi: 10.1097/IOP.0000000000001921.

