Abstract
Aim: To review definitions and elements of interventions in studies, which used the word “functional” to describe their intervention for children with cerebral palsy (CP), and to determine whether definitions and elements are similar to criteria of functional therapy described in the Dutch Guidelines.
Methods: Systematic review of intervention studies, which used the word “functional” to describe interventions for children with CP. We described criteria of functional therapy that were used to describe the intervention, and whether criteria were described similarly to the descriptions used in the Dutch Guidelines.
Results: Of the 27 included studies, criteria “based on the activities/participation level of the ICF-CY”, “goal-directed” and “context-specific” were referred to the most (40–59.3%). Descriptions of these criteria were less comparable to the suggested definition (43.8–69.2%). The remaining three criteria (“active involvement”, “task-specific”, and “focused on functionality instead of normality”) were referred to less frequently (18.5–33.3%). The descriptions reported for these criteria were, however, the most comparable with the suggested definitions (80–100%).
Conclusions: The included studies, in general have not used criteria of functional therapy. Future studies have to describe the elements of interventions in detail. Moreover, it is important to reach consensus on the definition and elements of functional therapy.
Introduction
There is an increasing number of studies of children with cerebral palsy (CP) that refer to their intervention as functional therapy. However, there is no standard description of what constitutes functional therapy. Ketelaar, Vermeer, Hart, van Petegem-van Beek, and Helders (Citation2001) described functional therapy as: “Functional physical therapy emphasizes the learning of motor abilities that are meaningful in the child’s environment and perceived as problematic by either the child or parents. Children practice these motor abilities in functional situations with the child having an active role in finding solutions for motor problems rather than having the physical therapist’s handling result in a solution. Functional goals, in terms of skills, are established with parents and children based on their priorities. Functional activities are assumed to be learned by repetitive practice of goal-related tasks in functional situations” (p. 1536) (Ketelaar et al., Ketelaar et al., Citation2001). Another study by Ahl, Johansson, Granat, and Carlberg, (Citation2005) described functional therapy in a similar manner: “Physical therapy in this context emphasizes the interaction between the individual, the task, and the environment as a basis for the child to learn; children actively seek effective solutions to problems that arise in situations they desire to master. The approach is called ‘functional’ as primarily functional skills (e.g. dressing and climbing stairs) are practiced to achieve functional goals. Defining specific goals can enhance motivation and, possibly, the child’s capacity to learn. In this context, the child can become an active problem solver instead of a passive recipient of treatment” (p. 613) (Ahl et al., Citation2005).
Over the last decade, there has been a substantial increase in therapy interventions addressing motor abilities of children with CP (Novak et al., Citation2013). Some of these studies refer to the intervention as functional therapy, but an elaborated description of the intervention is frequently missing (Sakzewski, Reedman, & Hoffmann, Citation2016). It can be questioned whether studies which refer to their intervention as functional therapy indeed examined interventions that align with the definition of functional therapy as described by Ketelaar et al. (Citation2001) and Ahl et al. (Citation2005). Vice versa, there may be other interventions that align with the definition of functional therapy, yet do not use this terminology to label their intervention.
Based on the lack of consensus on the definition and criteria for functional therapy, experts in the field of CP introduced six criteria to guide the implementation of functional therapy for children with CP. The group of experts consisted of members of the CP guideline steering group. Within this group of experts a total of five members were part of the consensus group, consisting of two experienced pediatric physical therapist, a pediatric occupational therapist, pediatric rehabilitation physician, and human movement scientist. The six criteria were selected during several expert meetings. First, all possible names and definitions of functional therapy were identified based on a comprehensive review of the literature and clinical experience, and discussed. The second step was to synthesize all names and definitions into a set of criteria defining functional therapy. After reaching consensus the criteria were then discussed with the other members of the steering group, which approved the following six criteria of functional therapy: (1) goal-directed, (2) based on the activities/participation level of the International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY), (3) task-specific, (4) active involvement of the child and parents to find solutions, learn motor skills and discover new possibilities, (5) focused on functionality rather than normality and (6) context specific (Revalidatieartsen, Citation2015). See for a more elaborated description of the criteria.
Table 1. Criteria of functional therapy of the Dutch guidelines (CitationRevalidatieartsen, 2015).
The aim of this systematic review was to review definitions and elements of interventions in studies, which used the word “functional” to describe their intervention for children with CP (aged ≤18 years), and to determine whether definitions and elements are similar to the criteria of functional therapy described in the Dutch Guidelines. The findings will provide evidence as to whether or not the construct functional therapy is generalizable across studies that specifically stated they used functional therapy and to provide recommendations for standardized criteria for clinical practice and research.
Methods
This systematic review was conducted in accordance with the PRISMA guidelines. A completed PRISMA checklist can be found in the Online Supplementary Appendix A.
Inclusion/Exclusion Criteria
This review included all intervention studies, which used the word “functional” to describe interventions for children with CP; only therapies that focused on oral function were excluded. Studies included randomized controlled trials (RCTs), clinical trials (CTs), two group comparison, non-randomized CTs, pre-post study design, CTs with only one data point and studies with a single subject design. Participants were children and/or adolescents with any type of CP. Studies which comprised both children with CP and children with other disorders were included if at least 50% of the study sample had a diagnosis of CP.
Literature Searches
Literature searches were performed using search strategies developed by one reviewer (MG). A total of five electronic databases were searched: EMBASE, MEDLINE, PubMed, CINAHL, and PEDro. The first search was performed on March 2016 with an update in January 2018. The search strategy was adapted according to the configuration and requirements of each database. The searches were developed using keywords (e.g. MeSH terms) and text words, combining population, and intervention related terms. The population related keyword was “cerebral palsy”. Intervention related search terms were “functional” in combination with “exercise”, “intervention”, “practice”, “program”, “therapy”, “training”, “treatment”, “rehabilitation”, or their plurals. Additional intervention related search terms were “task-oriented”, “task-specific”, and “goal-directed”. Literature searches were limited to articles published between 2000 and 2018, the English language and human subjects.
Identified references were downloaded in Endnote X7 software (Thomson Reuters, New York) for further assessment and handling, and duplicate records were removed.
Study Selection and Data Extraction
The first phase of the selection process was screening titles and abstracts on eligibility criteria to remove irrelevant reports. If there was any doubt regarding relevance, the report remained included at this stage. Subsequently, full texts were retrieved for all potentially relevant reports. Full-text reports were selected based on the inclusion and exclusion criteria. Multiple reports of the same study were identified and only the primary outcome paper of a study was included. Any available protocol papers of the included studies were retrieved for the data extraction.
The first phase of the selection process (i.e. screening of titles and abstracts) was performed by three reviewers (ER, MG, and MK), where each abstract was screened by two reviewers independently.
The second phase of the selection process (i.e. examination of the full-text reports) was performed independently by the same reviewers (ER, MG, and MK) in the same way as the first phase. In the case of discrepancies in any phase of the selection process, the third independent reviewer mediated to reach consensus.
After the selection process, data extraction was performed. Of the included studies, the following data were extracted: demographic information (age and type CP), methodology (study design, number of participants), whether the criteria of functional therapy (“goal-directed”, “based on activities/participation level of the ICF-CY”, “task-specific”, “active involvement”, “focused on functionality rather than normality”, and “context-specific”) were used to describe the intervention. We checked whether criteria were described similarly to the descriptions used in the Dutch Guidelines. In addition, we checked whether the criteria were mentioned in the method section. Mentioning the criteria in the method section is an indicator that it was part of the intervention.
Agreement
Agreement between the reviewers was determined by calculating Cohen’s Kappa (κ). Two independent reviewers checked if the authors used “functional” to describe their intervention. There was a high agreement (κ = 0.91) for “functional (therapy)” between the two reviewers. A third reviewer was consulted to reach consensus.
There were moderate to high levels of agreement between reviewers when determining whether criteria were mentioned in a study (goal-directed, κ = 0.92; based on activities/participation level of the ICF-CY κ = 0.70; task-specific κ = 0.78; active involvement κ = 0.74; focused on functionality rather than normality κ = 0.63; context specific κ = 0.78). When determining whether the definition of the criteria aligned with those used in this review, agreement between reviewers was moderate to good (goal-directed κ = 0.64; based on activities/participation level of the ICF-CY κ = 0.68; task-specific κ = 0.89; active involvement κ = 0.82; focused on functionality rather than normality κ = 1.00; context specific κ = 0.91). Consensus was reached for all criteria and definitions by consulting a third independent reviewer.
Results
Study Selection
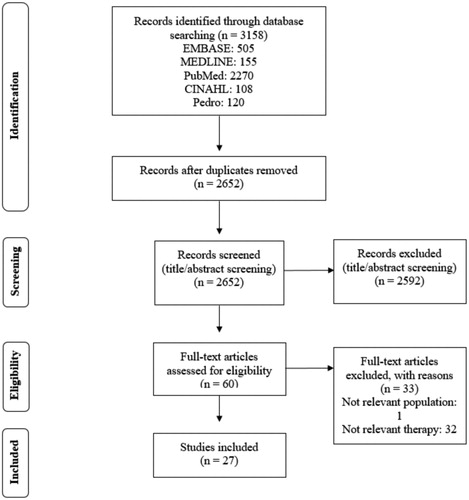
Literature searches of electronic databases retrieved 3158 titles/abstracts. After de-duplication, a total of 2652 titles/abstracts were screened, and 2592 articles were excluded because there was no therapeutic intervention. Full-text reports of 60 potentially relevant studies were selected for further examination. Of these, 33 studies were excluded after further examination for the following reasons: an adult population (1 article) or the authors did not use the word “functional” to describe their intervention (32 articles). A total of 27 studies met the criteria for inclusion in the review. A flow diagram of the identification and selection of studies for inclusion in this review is presented in .
Study Characteristics
All characteristics of the included studies are shown in . Several different types of intervention approaches were referred to by authors as functional therapy. For example home-based or modified constraint-induced movement therapy (CIMT) involving functional training of the involved hand (Chen et al., Citation2013; de Brito Brandao, Mancini, Vaz, Pereira de Melo, & Fonseca, Citation2010; Gordon et al., Citation2011; Chen et al., Citation2014; Citation2016; Xu, He, Mai, Yan, & Chen, Citation2015), goal-directed functional therapy (GDT) (Ahl et al., Citation2005; Lowing, Bexelius, & Brogren Carlberg, Citation2009; Lowing, Bexelius, & Carlberg, Citation2010; Storvold & Jahnsen, Citation2010), and functional (physical) training program (Akbari, Javad Zadeh, Shahraki, & Jahanshahi Javaran, Citation2009; Blundell, Shepherd, Dean, Adams, & Cahill, Citation2003; Ferre et al., Citation2017; Gorter, Holty, Rameckers, Elvers, & Oostendorp, Citation2009; Ketelaar et al., Citation2001; Kusumoto, Nitta, & Takaki, Citation2016; Lee, Ko, Shin, & Lee, Citation2015; Liao, Liu, Liu, & Lin, Citation2007; Moura et al., Citation2017; Peungsuwan, Parasin, Siritaratiwat, Prasertnu, & Yamauchi, Citation2017; Rameckers, Duysens, Speth, Vles, & Smits-Engelsman, Citation2010; Rameckers, Speth, Duysens, Vles, & Smits-Engelsman, Citation2009; Scholtes et al., Citation2010; van Vulpen, de Groot, Rameckers, Becher, & Dallmeijer, Citation2017).
Table 2. Characteristics of the included studies.
The age of participants included in the studies ranged from 1 to 18 years, the majority were school-aged children. According to the Surveillance of Cerebral Palsy in Europe (SCPE) terminology, eleven studies included only children with unilateral CP (Chen et al., Citation2013; de Brito Brandao et al., Citation2010; Ferre et al., Citation2017; Gordon et al., Citation2011; Chen et al., Citation2014; Citation2016; Moura et al., Citation2017; Rameckers et al., Citation2009; Citation2010; Sung et al., Citation2005; Xu et al., Citation2015). Eight studies included both unilateral and bilateral CP (Akbari et al., Citation2009; Ketelaar et al., Citation2001; Lowing et al., Citation2009; Citation2010; Peungsuwan et al., Citation2017; Scholtes et al., Citation2010; Storvold & Jahnsen, Citation2010; van Vulpen et al., Citation2017). Five studies included children with bilateral CP (Ahl et al., Citation2005; Blundell et al., Citation2003; Kusumoto et al., Citation2016; Liao et al., Citation2007; Lin et al., Citation2015). Three studies did not specify the subtype of CP (Gorter et al., Citation2009; Lammi & Law, Citation2003; Lee et al., Citation2015).
Criteria and Definition of Criteria
All 27 studies referred to functional therapy, mostly in the methods section (23 studies; 85.2%). Of these 27 studies only one study referred to all six criteria, whereas four studies referred to five criteria. Three studies referred to four criteria, four studies referred to three criteria, and another four studies to two criteria. Four studies referred to only one criterion and seven studies did not refer to any criterion. lists the criteria and definitions mentioned in the method section of each study. A more detailed overview of the criteria of functional therapy and definitions mentioned in the included studies, and in which section of the paper the criteria were mentioned can be found in and .
Figure 2. Criteria and definition mentioned in the method section of each study. When the definition was not in line with the proposed definition an * was placed in the box.
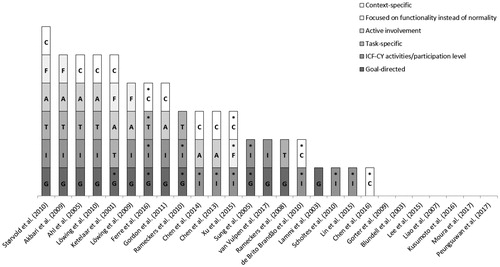
Table 3. Criteria of functional therapy mentioned in the included papers, and in which section of the paper.
Table 4. Comparison of the proposed definitions with the definitions of the criteria that were mentioned in the methods section of the included papers.
Of the six proposed criteria, “based on the activities/participation level of the ICF-CY” was referred to the most in 16 (59.3%) of the studies followed by the criterion “goal-directed” in 13 (48.1%) and “context-specific” in 11 (40.7%). The descriptions of these criteria, however, were only comparable to the suggested definition of the Dutch guidelines in 7 (43.8%), 9 (69.2%), and 7 (63.6%) of the studies respectively. The remaining three criteria were referred to less frequently. The criterion “active involvement” was described in 9 (33.3%) studies, “task-specific” in 8 (29.6%) and “focused on functionality instead of normality” in 5 (18.5%). The descriptions reported for these three criteria were, however, the most comparable with the suggested definitions of the Dutch guidelines (80–100%). The descriptions for all criteria were reported in the methods section of each study. No other definitions for the criteria were found in the studies.
Discussion
The aim of this systematic review was to review definitions and elements of interventions in studies which used the word “functional” to describe their intervention for children with CP, and to determine whether definitions and elements are similar to the criteria of functional therapy described in the Dutch Guidelines. A clear description of treatment methodology or taxonomy for rehabilitation is crucial to compare studies and to unravel the black box, called intervention (Craig et al., Citation2008; Dijkers, Hart, Tsaousides, Whyte, & Zanca, Citation2014). Our comprehensive literature search identified a range of different interventions targeting both upper and lower extremity function, all of which were described as functional therapy. Findings of this review demonstrate inconsistent descriptions and definitions of the multiple elements of functional therapy, with three or more of six criteria reported in less than 50% of the studies.
While all studies described their intervention as functional therapy, lack of a clear description of the essential elements made it difficult to match against our proposed six criteria. Firstly, it is shown that the total set of all six criteria to describe functional therapy was not or rarely used. Only one of the 27 studies referred to all six criteria in their article, whereas seven studies referred to none of the criteria. In most studies, there is a description of the intervention, but the intervention is not described in terms of the proposed criteria. Secondly, the referred criteria were used to a varying extent. The criteria “based on activities/participation level of the ICF-CY” and “goal-directed” were referred to most frequently while the criterion “focused on functionality rather than normality” was referred to only in five studies. The criteria “based on activities/participation level of the ICF-CY” and “goal-directed” are already well known and often used in reviews and papers to describe interventions for children with CP. The criterion “focused on functionality rather than normality” is a very specific element and therefore may not always be explicitly mentioned. The agreement between the reviewers for this criterion was moderate, so even if it is mentioned it can be interpreted differently. The criteria “task-specific”, “active involvement”, and “context-specific” are based on motor learning principles and therefore not explicitly mentioned separately (Shumway-Cook & Woollacott, Citation2007). Thirdly, when the criteria were mentioned, a definition was not always provided. Eight studies referring to one or more criteria did provide definitions for all mentioned criteria, whereas seven studies naming one or more of the criteria did not provide any definition. When criteria were defined, these definitions were in extent in line with the definitions of the Dutch guidelines used in this review, only the definitions of the criterion “based on activities/participation level of the ICF-CY” showed minimal agreement with the definition used in this review. The definition used in this review links the ICF model to activity-based intervention goals, which is often not the case in the definitions mentioned in the studies. Also, the agreement between the reviewers for this criterion was moderate, so despite the fact that this criterion is mentioned most frequently, the definition may be too broad. Overall, it is obvious that the criteria of functional therapy and their definitions are not yet well incorporated in research about functional therapy.
The lack of reporting on the elements and definitions of functional therapy does not necessarily mean that the studies did not use all these components. Hoffmann, Erueti, and Glasziou (Citation2013) investigated the completeness of descriptions of non-pharmacological interventions in randomized trials. The results showed that 39% of the interventions were adequately described, but after contact with the authors to get more information, it increased to 59% (Hoffmann et al., Citation2013). We may have been able to get additional information if we had approached the authors directly. Possibly a percentage of the excluded studies might have included functional interventions, without describing the therapy as functional, for example the studies of Cameron et al. (Citation2016), Kruijsen-Terpstra et al. (Citation2016)and Law et al. (Citation2011). Also, several excluded studies did indeed describe elements of functional therapy but were not included on the sole basis that they did not use “functional” to describe their interventions. However, this review was not intended to include all papers examining functional therapy but aimed to examine the use of terminology. We also saw that different terms have been used to describe a “functional” approach of the intervention, such as task-oriented, activity-focused, and goal-directed. It is essential to use the same terminology when describing interventions, so it is clear what has been done and to compare intervention approaches.
Rehabilitation approaches for children with CP are inherently complex, multi-faceted, and comprise a number of interconnected elements. A clear description of each of the elements of an intervention is required for standardization, usability and replication. Unclear descriptions will hamper evidence uptake into clinical practice (implementation), and interventions are unlikely to be delivered as intended with fidelity. Therefore, a clear description of the intervention is of great importance. A tool for intervention description and replication are the TIDieR guidelines (Hoffmann et al., Citation2014). When interventions are clearly described in clinical guidelines or in consensus statements, the protocols can be more readily embedded in clinical practice. The consensus statement in stroke research is an example, in which definitions and a shared vision for new standards in stroke recovery have been agreed upon internationally (Bernhardt et al., Citation2017). The Dutch Guideline for diagnosis and treatment of children with spastic CP might be a starting point to bring people together internationally to reach consensus on the definitions of these elements of functional therapy.
Our systematic review concluded that the set criteria and definitions of functional therapy were frequently not used in the included studies. It is of great importance that interventions are described in detail for both research and clinical practice. The criteria as described in the Dutch Guideline for diagnosis and treatment of children with spastic CP are a helpful tool to describe elements of functional interventions. The next step is to reach international consensus on the elements of functional therapy to promote standardization and widespread use.
Supplemental Material
Download PDF (28 KB)Acknowledgments
We would like to thank the members of the consensus group that worked on the chapter on functional therapy in the Dutch Guideline for diagnosis and treatment of children with spastic CP (L. van Wely, R. Wong Chung, and N. van den Dikkenberg) for their role and input in the process of defining the criteria for functional therapy.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ahl, L. E., Johansson, E., Granat, T., & Carlberg, E. B. (2005). Functional therapy for children with cerebral palsy: An ecological approach. Developmental Medicine & Child Neurology, 47(9), 613–619. doi:10.1111/j.1469-8749.2005.tb01213.x
- Akbari, A., Javad Zadeh, M., Shahraki, S., & Jahanshahi Javaran, P. (2009). The effects of functional therapy on motor development in children with cerebral palsy. Iran Journal of Child Neurology, 3(3), 23–32.
- Bernhardt, J., Hayward, K. S., Kwakkel, G., Ward, N. S., Wolf, S. L., Borschmann, K., … Cramer, S. C. (2017). Agreed definitions and a shared vision for new standards in stroke recovery research: The stroke recovery and rehabilitation roundtable taskforce. Neurorehabilitation and Neural Repair, 31(9), 793–799. doi:10.1177/1545968317732668
- Blundell, S. W., Shepherd, R. B., Dean, C. M., Adams, R. D., & Cahill, B. M. (2003). Functional strength training in cerebral palsy: A pilot study of a group circuit training class for children aged 4-8 years. Clinical Rehabilitation, 17(1), 48–57. doi:10.1191/0269215503cr584oa
- Cameron, D., Craig, T., Edwards, B., Missiuna, C., Schwellnus, H., & Polatajko, H. J. (2016). Cognitive orientation to daily occupational performance (CO-OP): A new approach for children with cerebral palsy. Physical & Occupational Therapy in Pediatrics, 37(2), 183–198. doi:10.1080/01942638.2016.1185500
- Chen, H. C., Chen, C. L., Kang, L. J., Wu, C. Y., Chen, F. C., & Hong, W. H. (2014). Improvement of upper extremity motor control and function after home-based constraint induced therapy in children with unilateral cerebral palsy: Immediate and long-term effects. Archives of Physical Medicine and Rehabilitation, 95(8), 1423–1432. doi:10.1016/j.apmr.2014.03.025
- Chen, H. C., Kang, L. J., Chen, C. L., Lin, K. C., Chen, F. C., & Wu, K. P. (2016). Younger children with cerebral palsy respond better than older ones to therapist-based constraint-induced therapy at home on functional outcomes and motor control. Physical & Occupational Therapy in Pediatrics, 36(2), 171–185. doi:10.3109/01942638.2015.1101042
- Chen, C. L., Kang, L. J., Hong, W. H., Chen, F. C., Chen, H. C., & Wu, C. Y. (2013). Effect of therapist-based constraint-induced therapy at home on motor control, motor performance and daily function in children with cerebral palsy: A randomized controlled study. Clinical Rehabilitation, 27(3), 236–245. doi:10.1177/0269215512455652
- Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., & Petticrew, M, & Medical Research Council, G. (2008). Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ, 337, a1655. doi:10.1136/bmj.a1655
- de Brito Brandao, M., Mancini, M. C., Vaz, D. V., Pereira de Melo, A. P., & Fonseca, S. T. (2010). Adapted version of constraint-induced movement therapy promotes functioning in children with cerebral palsy: A randomized controlled trial. Clinical Rehabilitation, 24(7), 639–647. doi:10.1177/0269215510367974
- Dijkers, M. P., Hart, T., Tsaousides, T., Whyte, J., & Zanca, J. M. (2014). Treatment taxonomy for rehabilitation: Past, present, and prospects. Archives of Physical Medicine and Rehabilitation, 95(1), S6–S16. doi:10.1016/j.apmr.2013.03.032
- Ferre, C. L., Brandao, M., Surana, B., Dew, A. P., Moreau, N. G., & Gordon, A. M. (2017). Caregiver-directed home-based intensive bimanual training in young children with unilateral spastic cerebral palsy: A randomized trial. Developmental Medicine & Child Neurology, 59(5), 497–504. doi:10.1111/dmcn.13330
- Gordon, A. M., Hung, Y.-C., Brandao, M., Ferre, C. L., Kuo, H.-C., Friel, K., … Charles, J. R. (2011). Bimanual training and constraint-induced movement therapy in children with hemiplegic cerebral palsy. Neurorehabilitation and Neural Repair, 25(8), 692–702. doi:10.1177/1545968311402508
- Gorter, H., Holty, L., Rameckers, E. E., Elvers, H. J., & Oostendorp, R. A. (2009). Changes in endurance and walking ability through functional physical training in children with cerebral palsy. Pediatric Physical Therapy, 21(1), 31–37. doi:10.1097/PEP.0b013e318196f563
- Hoffmann, T. C., Erueti, C., & Glasziou, P. P. (2013). Poor description of non-pharmacological interventions: Analysis of consecutive sample of randomised trials. BMJ, 347, f3755. doi:10.1136/bmj.f3755
- Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., … Michie, S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ, 348, g1687. doi:10.1136/bmj.g1687
- Ketelaar, M., Vermeer, A., Hart, H., van Petegem-van Beek, E., & Helders, P. J. (2001). Effects of a functional therapy program on motor abilities of children with cerebral palsy. Physical Therapy, 81(9), 1534–1545. doi:10.1093/ptj/81.9.1534
- Kruijsen-Terpstra, A. J. A., Ketelaar, M., Verschuren, O., Gorter, J. W., Vos, R. C., Verheijden, J., … Visser-Meily, A. (2016). Efficacy of three therapy approaches in preschool children with cerebral palsy: A randomized controlled trial. Developmental Medicine & Child Neurology, 58(7), 758–766. doi:10.1111/dmcn.12966 doi:10.1111/dmcn.12966
- Kusumoto, Y., Nitta, O., & Takaki, K. (2016). Impact of loaded sit-to-stand exercises at different speeds on the physiological cost of walking in children with spastic diplegia: A single-blind randomized clinical trial. Research in Developmental Disabilities, 57, 85–91. doi:10.1016/j.ridd.2016.06.006
- Lammi, B. M., & Law, M. (2003). The effects of family-centred functional therapy on the occupational performance of children with cerebral palsy. Canadian Journal of Occupational Therapy, 70(5), 285–297. doi:10.1177/000841740307000505
- Law, M., Baptiste, S., McColl, M., Opzoomer, A., Polatajko, H., & Pollock, N. (1990). The Canadian occupational performance measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy, 57(2), 82–87.
- Law, M. C., Darrah, J., Pollock, N., Wilson, B., Russell, D. J., Walter, S. D., … Galuppi, B. (2011). Focus on function: A cluster, randomized controlled trial comparing child- versus context-focused intervention for young children with cerebral palsy. Developmental Medicine & Child Neurology, 53(7), 621–629. doi:10.1111/j.1469-8749.2011.03962.x
- Lee, M., Ko, Y., Shin, M. M., & Lee, W. (2015). The effects of progressive functional training on lower limb muscle architecture and motor function in children with spastic cerebral palsy. Journal of Physical Therapy Science, 27(5), 1581–1584. doi:10.1589/jpts.27.1581
- Liao, H. F., Liu, Y. C., Liu, W. Y., & Lin, Y. T. (2007). Effectiveness of loaded sit-to-stand resistance exercise for children with mild spastic diplegia: A randomized clinical trial. Archives of Physical Medicine and Rehabilitation, 88(1), 25–31. doi:10.1016/j.apmr.2006.10.006
- Lin, Y. C., Huang, C. Y., Lin, I. L., Shieh, J. Y., Chung, Y. T., & Chen, K. L. (2015). Evaluating functional outcomes of botulinum toxin type a injection combined with occupational therapy in the upper limbs of children with cerebral palsy: A 9-month follow-up from the perspectives of both child and caregiver. PLoS One, 10(11), e0142769. doi:10.1371/journal.pone.0142769
- Lowing, K., Bexelius, A., & Brogren Carlberg, E. (2009). Activity focused and goal directed therapy for children with cerebral palsy–do goals make a difference? Disability and Rehabilitation, 31(22), 1808–1816. doi:10.1080/09638280902822278
- Lowing, K., Bexelius, A., & Carlberg, E. B. (2010). Goal-directed functional therapy: A longitudinal study on gross motor function in children with cerebral palsy. Disability and Rehabilitation, 32(11), 908–916. doi:10.3109/09638280903353422
- Moura, R. C. F., Santos, C., Collange Grecco, L., Albertini, G., Cimolin, V., Galli, M., & Oliveira, C. (2017). Effects of a single session of transcranial direct current stimulation on upper limb movements in children with cerebral palsy: A randomized, sham-controlled study. Developmental Neurorehabilitation, 20(6), 368–375. doi:10.1080/17518423.2017.1282050
- Novak, I., Mcintyre, S., Morgan, C., Campbell, L., Dark, L., Morton, N., … Goldsmith, S. (2013). A systematic review of interventions for children with cerebral palsy: State of the evidence. Developmental Medicine & Child Neurology, 55(10), 885–910. doi:10.1111/dmcn.12246
- Peungsuwan, P., Parasin, P., Siritaratiwat, W., Prasertnu, J., & Yamauchi, J. (2017). Effects of combined exercise training on functional performance in children with cerebral palsy: A randomized-controlled study. Pediatric Physical Therapy, 29(1), 39–46. doi:10.1097/PEP.0000000000000338
- Rameckers, E. A., Duysens, J., Speth, L. A., Vles, H. J., & Smits-Engelsman, B. C. (2010). Effect of addition of botulinum toxin-A to standardized therapy for dynamic manual skills measured with kinematic aiming tasks in children with spastic hemiplegia. Journal of Rehabilitation Medicine, 42(4), 332–338. doi:10.2340/16501977-0521
- Rameckers, E. A., Speth, L. A., Duysens, J., Vles, J. S., & Smits-Engelsman, B. C. (2009). Botulinum toxin-a in children with congenital spastic hemiplegia does not improve upper extremity motor-related function over rehabilitation alone: A randomized controlled trial. Neurorehabilitation and Neural Repair, 23(3), 218–225. doi:10.1177/1545968308326629
- Revalidatieartsen, N. V. V. (2015). Richtlijn Spastische cerebrale parese bij kinderen. Retrieved from https://richtlijnendatabase.nl/richtlijn/spastische_cerebrale_parese_bij_kinderen/spastische_cerebrale_parese_-_startpagina.html.
- Sakzewski, L., Reedman, S., & Hoffmann, T. (2016). Do we really know what they were testing? Incomplete reporting of interventions in randomised trials of upper limb therapies in unilateral cerebral palsy. Research in Developmental Disabilities, 59, 417–427. doi:10.1016/j.ridd.2016.09.018
- Scholtes, V. A., Becher, J. G., Comuth, A., Dekkers, H., Van Dijk, L., & Dallmeijer, A. J. (2010). Effectiveness of functional progressive resistance exercise strength training on muscle strength and mobility in children with cerebral palsy: A randomized controlled trial. Developmental Medicine & Child Neurology, 52(6), e107–113. doi:10.1111/j.1469-8749.2009.03604.x
- Shumway-Cook, A., & Woollacott, M. H. (2007). Motor control. Translating research into clinical practice. Philadelphia: Lippincott Williams & Wilkins.
- Storvold, G. V., & Jahnsen, R. (2010). Intensive motor skills training program combining group and individual sessions for children with cerebral palsy. Pediatric Physical Therapy, 22(2), 150–159. doi:10.1097/PEP.0b013e3181dbe379
- Sung, I. Y., Ryu, J. S., Pyun, S. B., Yoo, S. D., Song, W. H., & Park, M. J. (2005). Efficacy of forced-use therapy in hemiplegic cerebral palsy. Archives of Physical Medicine and Rehabilitation, 86(11), 2195–2198. doi:10.1016/j.apmr.2005.05.007
- Turner-Stokes, L. (2009). Goal attainment scaling (GAS) in rehabilitation: A practical guide. Clinical rehabilitation, 23(4), 362–370.
- van Vulpen, L. F., de Groot, S., Rameckers, E. A. A., Becher, J. G., & Dallmeijer, A. J. (2017). Effectiveness of functional power training on walking ability in young children with cerebral palsy: study protocol of a double-baseline trial. Pediatric Physical Therapy, 29(3), 275–282. doi:10.1097/PEP.0000000000000424
- World Health Organization. (2007). International classification of functioning, disability and health: Children and youth version. Geneva, Switzerland: WHO Press.
- Xu, K., He, L., Mai, J., Yan, X., & Chen, Y. (2015). Muscle recruitment and coordination following constraint-induced movement therapy with electrical stimulation on children with hemiplegic cerebral palsy: A randomized controlled trial. PLoS One, 10(10), e0138608. doi:10.1371/journal.pone.0138608