?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Aim
The aim of this study was to evaluate the construct validity of the Both Hands Assessment (BoHA) using activity of the upper limbs as detected by accelerometry in children with bilateral cerebral palsy (CP).
Methods
Observational study of children with CP (n = 44, n = 27 boys, aged 9.1 ± 1.6 years; Manual Ability Classification Scale I: n = 15, II: n = 22, III: n = 7) completing a BoHA assessment while wearing a triaxial accelerometer on each wrist. BoHA Each-Hand sub-scores, BoHA percentage difference between hands, BoHA Units, mean activity for each hand, mean activity asymmetry index and total mean activity were calculated. Linear regressions were used to analyze associations between measures.
Results
There were significant, positive associations between BoHA Units and total mean activity (B = 0.86, 95%CI: 0.32, 1.40), BoHA Percentage difference between hands and mean activity asymmetry index (B = 0.95, 95%CI: 0.75,1.15), and BoHA Each-Hand sub-score and mean activity for the non-dominant hand (B = 1.71, 95%CI: 1.16, 2.28), but not the dominant hand (B = 0.50, 95%CI: −0.45, 1.45).
Conclusions
This study provides further evidence for the construct validity of the BoHA as a measure of upper limb performance. Wearable wrist sensors such as accelerometers capture and quantify gross upper limb movement in children with CP but cannot measure fine finger movements captured by the BoHA.
Clinical trials registration
Australian New Zealand Clinical Trials Registry (ACTRN12616001488493 and ACTRN12618000164291)
Clinicians who work with children who have cerebral palsy (CP) require valid and reliable outcome measures of hand and upper limb function as an essential component of evidence-based clinical practice. Where appropriate, clinicians use information from standardized outcome measures, previous clinical experience and research evidence, together with knowledge about the child, and their circumstances and goals to inform clinical reasoning (Occupational Therapy Australia, Citation2019). Systematic reviews (Burgess et al., Citation2019; Gilmore et al., Citation2010) of upper limb activity measures for children with CP identified the Assisting Hand Assessment (AHA) (Krumlinde-Sundholm and Eliasson Citation2003) and the Both Hands Assessment (BoHA) (Elvrum et al., Citation2018) as tools which measure upper-limb activity performance for children with unilateral and bilateral CP respectively (World Health Organization, Citation2007). Unilateral CP is defined as having motor involvement on one side of the body, while bilateral CP indicates motor involvement on both sides of the body (Surveillance of Cerebral Palsy in Europe, Citation2000). Activity is defined as the carrying out of a task, and may be assessed using measures of performance (which pertain to what a child does in real life in their everyday environment) or measures of capacity (what a child can do in a standardized environment) (World Health Organization, Citation2007). Bimanual activity performance therefore involves the coordinated use of both hands together in activities involving everyday tasks, which shows the usual, self-initiated level of bimanual skill.
The BoHA is a relatively new measure that was developed through adaptation of the AHA. The BoHA measures and describes how effectively children with bilateral CP use their hands in spontaneous bimanual activity performance (Elvrum et al., Citation2018). It was designed for children aged between 18 months and 12 years of age, who are classified Manual Ability Classification System (MACS) levels I-III (Elvrum et al., Citation2018). Toys are used which elicit or provoke bimanual handling in a semi-structured play session, with the child sitting at a table. The play session is video-recorded and then later scored according to specific criteria (Elvrum et al., Citation2018). There are eleven unimanual items and five bimanual items on which hand function is scored. The unimanual items are scored for both the right hand and left hand separately and cover initiation of movements, speed, and quality of movements, reaching, grasp and release, and fine motor adjustments. The unimanual items are summed for each hand and produce a raw score referred to as the BoHA Each-Hand sub-score for both the left hand and right hand (sub-score ranges between 11 and 44). The five bimanual items examine how ‘both hands work together’ and encompass the pace and flow with which activities are performed and coordination of the hands together. All unimanual and bimanual items are scored according to a 4-level rating, where 4 indicates ‘effective’ and a rating of 1 indicates ‘does not do’. The right and left hand BoHA Each-Hand sub-scores are combined with the score for the bimanual items to provide a total raw sum score (range 27–108). The total raw sum is then converted to a BoHA Unit (0–100 scale). Higher BoHA Units reflect better bimanual performance. The BoHA contains two unidimensional scales which are used to convert the raw scores to BoHA Units. The BoHA-A is used for children who demonstrate asymmetrical hand use (≥20% difference between the hands in the unimanual items). The BoHA-S is used for children who present with symmetrical hand use (<20% difference between hands in unimanual items).
The BoHA has high inter-rater reliability (Klevberg et al., Citation2018), is able to discriminate between Manual Ability Classification (MACS) levels I to III (Burgess et al., Citation2021) and, correlates strongly with MACS levels (Elvrum et al., Citation2018). BoHA scores also exhibit moderate to strong correlation with measures of upper limb capacity as measured by the Melbourne Assessment-2 subscales of range of motion, accuracy, dexterity and fluency for both the dominant and non-dominant hand, the Box and Blocks Test for the dominant and non-dominant hand (Elvrum et al., Citation2022), and measures of self-care performance using the Pediatric Evaluation of Disability Inventory (Elvrum et al., Citation2022). Children with bilateral CP with asymmetrical hand use tend to perform worse on the BoHA than children with symmetrical hand use, and are usually classified MACS levels II and III (Burgess et al., Citation2021). It should be noted that a person without CP, with typical hand function would have symmetrical hand function measured using the BoHA (Burgess et al., Citation2021).
Further psychometric studies have been recommended to confirm the validity of the BoHA (Burgess et al., Citation2019). Construct validity is “the degree to which the scores of a measurement instrument are consistent with hypotheses, for instance, with regard to internal relationships, relationships with scores of other instruments or differences between relevant groups” (de Vet et al., Citation2011, p. 169; Mokkink et al., Citation2010). The use of wrist-worn accelerometers is a valid method of detecting and quantifying objective arm movement in children with CP using movement detected in three orthogonal axes, which are often reported as ‘activity counts’ (Beani et al., Citation2019; Braito et al., Citation2018). The aim of this study was to evaluate the construct validity of the BoHA through hypothesis testing of the expected relationship between BoHA scores and activity of the upper limbs as measured by accelerometry. Specifically, we hypothesized that in children with bilateral CP:
There will be a moderate to strong positive correlation between a child’s overall BoHA Units and the total of mean accelerometer activity counts (sum of left and right hand).
There will be a moderate to strong positive correlation between the BoHA Each-Hand sub-score and accelerometer activity counts for the dominant hand.
There will be a moderate to strong positive correlation between the BoHA Each-Hand sub-score and the accelerometer activity counts for the non-dominant hand.
There will be a moderate to strong positive correlation between the BoHA Percentage difference between hands and asymmetry in upper limb movement as quantified by accelerometer data.
Methods
Design
This study used data from two studies, PREDICT-CP (Partnership Project: Comprehensive Surveillance to Predict Outcomes for School age Children with CP) (Boyd et al., Citation2017) and HABIT-ILE (Hand Arm Bimanual Intensive Training Including Lower Extremity Training) (Sakzewski et al., Citation2019). PREDICT-CP was a follow-up of a prospective longitudinal cohort study called CP Child (Boyd et al., Citation2013). Children born in Queensland, Australia between 2006 and 2009 were eligible to participate in CP Child, and they were assessed up to six times between 18 months and 5 years. All CP Child participants were invited back to participate in PREDICT-CP which was a single assessment between 8 and 12 years (Boyd et al., Citation2013).
HABIT-ILE was a multi-site waitlist randomized controlled trial with assessments at baseline, immediately post intervention, and at 26 weeks post-intervention (Sakzewski et al., Citation2019). To be eligible for inclusion, children had to be 6–16 years, have a diagnosis of bilateral CP and gross motor function classification (GMFCS) II-IV, be able to grasp light objects and lift their most impaired arm ≥15 cm above a table surface, and be able to understand instructions and complete testing. All assessments were completed at the Queensland Cerebral Palsy and Rehabilitation Research Center, Brisbane, Australia. Both studies had ethical approval and caregivers gave written consent for participation and publication (Children’s Health Queensland Hospital and Health Service Human Research Ethics Committee (HREC/14/QRCH/329 and HREC/17/QRCH/282) and the University of Queensland’s Human Research Ethics Committees (2014001487 and 2018000017/HREC/17/QRCH/2820) and The Cerebral Palsy Alliance Ethics Committee (2018_04_01/HREC/17/QRCH/282) and were registered in the Australian New Zealand Clinical Trials Registry (ACTRN12616001488493 and ACTRN12618000164291).
Participants
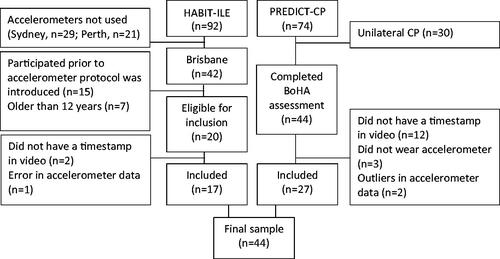
A total of n = 74 children participated in PREDICT-CP and n = 92 participated in HABIT-ILE (). From PREDICT-CP, only children with bilateral CP could be included in the current study, and from HABIT-ILE, only participants aged ≤12 years who attended the primary study site assessments after September 2019 could be included, as the BoHA is only validated for ≤12-year-olds, and accelerometers were only utilized at the primary study site from the specified date. In the current study, the baseline BoHA of the children participating in HABIT-ILE was used in all but one case, in which their 26-week post-intervention assessment was used. A total of 64 children (n = 20 from HABIT-ILE and n = 44 from PREDICT-CP were eligible to participate in the current study, however n = 14 participants lacked a timestamp in their video and n = 3 participants did not wear an accelerometer, and could not be included. Further, during data inspection, n = 3 participants were identified as outliers (>3SD difference from the mean) in the accelerometry data and were excluded from analysis. Two of these participants had a dystonic motor type causing very high activity counts and the third appeared to be an error with the accelerometer data download itself. In the BoHA data, n = 1 participant was identified as a mild outlier (>2SD difference from the mean). Their video was inspected, and their score was deemed to be correct. The inclusion of this participant in the analyses did not significantly change the estimates, hence they were included.
The final sample therefore included 44 children (27 from PREDICT-CP and 17 from HABIT-ILE), ranging in age from 6 to 12 years, with a mean age of 9 (SD 1.6) years (). The sample consisted of more boys (n = 27, 61%) and a primary motor type of spasticity (n = 36, 82%). Participants were classified as MACS levels I (n = 15), II (n = 22) and III (n = 7). Participants were more frequently right-hand dominant (n = 26) than left (n = 15), and three children demonstrated mixed hand dominance. There were eight children with ≥20% asymmetry on the BoHA asymmetry index.
Table 1. Sample characteristics.
Measures and Procedure
Classifications
All children had a confirmed diagnosis of bilateral CP (Rosenbaum et al., Citation2007; Surveillance of Cerebral Palsy in Europe, Citation2000). Children were classified using the Manual Abilities Classification System (MACS) and the Gross Motor Function Classification Scale (GMFCS). The MACS classifies a child’s ability to handle objects in daily life on a five-level ordinal scale, and has established construct validity and excellent inter-rater reliability (Eliasson et al., Citation2006). The GMFCS classified as child’s ability to carry out self-generated movements related to sitting and walking on a five-level ordinal scale and has established construct validity and good inter-rater reliability (Palisano et al., Citation2008; Rosenbaum et al., Citation2008). Hand dominance was determined using the Edinburgh Handedness Inventory (Oldfield, Citation1971) in PREDICT-CP and by parent/child report in HABIT-ILE. Motor type was classified as spastic, dyskinetic, ataxic or hypotonic according to the Surveillance of CP in Europe guidelines (Surveillance of Cerebral Palsy in Europe, Citation2000). Rating of the MACS and GMFCS were performed by experienced physiotherapists and occupational therapists in collaboration with the child’s primary caregiver. Motor type was often recorded in hospital records and was confirmed by the research therapists.
Both Hands Assessment (BoHA)The BoHA is an objective, criterion referenced, Rasch modeled assessment tool (Elvrum et al., Citation2018). The BoHAs were administered according to the BoHA test guidelines by one of three authors (AB, LS, and SR) who are all certified. A height-adjustable table and chair was used to provide appropriate seating for each child. The video camera was placed high, diagonally opposite the non-dominant hand to enable a clear view of the child’s hands. Assessment time varied between 9 and 28 min, depending on the child’s level of impairment. All BoHAs were scored by the first author (AB). When scoring, the assessor frequently paused and re-played the recording, each video varied in the time required for scoring, but commonly took around 30–60 min to score.
Accelerometry
The ActiGraph GT3X+ (ActiGraph Corporation, Pensacola, FL, USA) is a triaxial accelerometer (4.6 cm x3.3 cm x1.5 cm, 19 g). Children wore one accelerometer on each wrist during a videotaped BoHA assessment, and the acceleration along three orthogonal axes (x, y, z) was collected (30 Hz). Prior to each BoHA assessment, an external timepiece was synchronized with the laptop computer used to initialize the accelerometers and displayed in front of the camera to ensure synchronization between video files and accelerometer timestamps. Accelerometer data were downloaded using ActiLife v.6.13.4, raw acceleration data were converted to proprietary activity counts per second and vector magnitude was calculated (√[x2+y2+z2]). Mean activity during the BoHA assessment was calculated by dividing the sum of vector magnitude for each hand during BoHA assessment by the total time the participant took to complete the BoHA play session in seconds (Beani et al., Citation2019). Total mean activity was then calculated by adding the mean activity for the dominant and non-dominant hand. For those with mixed hand dominance (n = 4), the upper limb which they use to write was designated as the dominant hand. To quantify asymmetry in hand movement during the BoHA assessment, an asymmetry index for the accelerometry data was calculated using mean activity with the following formula (Beani et al., Citation2019):
Data Analysis
Data were analyzed using the statistical package Stata (StataCorp, v.17, College Station, TX, USA). Sample characteristics were reported as mean (standard deviation) and frequency (percentage). BoHA and accelerometer measures were reported by MACS level as means (standard deviation) and One-way ANOVAs and t-tests were used to describe differences in BoHA and accelerometer variables within and between MACS level. To test the hypotheses, linear regression was used to assess the association between 1) BoHA Units and total mean activity, 2) BoHA Each-Hand sub-score and mean activity for the dominant and non-dominant hand separately, and 3) BoHA Percentage difference between hands and the mean activity asymmetry index. Within each regression model, age, gender, and the interaction between MACS and BoHA variables tested for significance. Significance level for all tests was set to p < 0.05. Data were inspected to ensure assumptions for linear regression were met, and to identify any outliers. Standardized betas (β) were calculated to assess the strength of correlations between the accelerometer and BoHA measures for each hypothesis. The relative strength of correlations was defined as β = 0.00–0.10 (negligible correlation), β = 0.10–0.39 (weak correlation), β = 0.40–0.69 (moderate correlation), β = 0.70–0.89 (strong correlation), β = 0.90–1.00 (very strong correlation) (Schober et al., Citation2018).
Results
The mean BoHA Units, total mean activity, BoHA Each-Hand sub-scores and mean activity for the dominant and non-dominant hand, BoHA Percentage difference between hands and mean activity asymmetry index by MACS level for the study sample are presented in . There was a statistically significant difference in BoHA Units, Sum of mean activity, BoHA Percentage difference between hands and Mean activity asymmetry index between MACS levels I-III, and between the BoHA Each Hand sub-scores and Mean activity for the dominant and non-dominant hand within MACS levels II and III, but not MACS level I. Age, gender, and the interaction between BoHA variables and MACS level were not significant, and these were not included in any of the regression analyses reported below.
Table 2. Mean both hands (BoHA) assessment units and mean activity counts by manual ability classification scale (MACS) level, BoHA Each-Hand Sub-scores and mean activity counts for the dominant and non-dominant hand by MACS level and BoHA percentage difference between hand and mean activity asymmetry index by MACS level.
The association between BoHA Units and total mean activity is displayed in . There was a significant, moderate, positive correlation between the overall BoHA Units and the total mean activity (B = 0.86, 95%CI: 0.32, 1.40, p = 0.002; β = 0.45).
Figure 2. (a) Association between BoHA units and total mean activity. (b) Association between BoHA Each-Hand Sub-score and mean activity by limb. (c) Association between the mean activity and BoHA asymmetry indexes of X children with bilateral cerebral palsy.
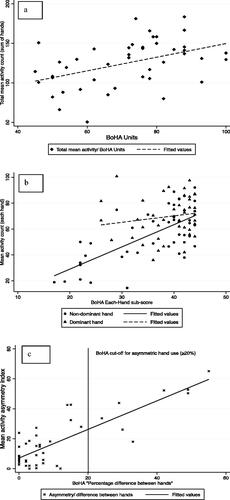
The association between BoHA Each-Hand sub-score and mean activity count for each hand is displayed in . For the dominant hand, there was a weak, non-significant correlation between the BoHA Each-Hand sub-score and the mean activity count (B = 0.50, 95%CI: −0.45, 1.45 p = 0.29; β = 0.16). For the non-dominant hand there was a significant, moderate positive correlation between the BoHA Each-Hand sub-score and the mean activity count (B = 1.71, 95%CI: 1.16, 2.28 p < 0.001; β = 0.69).
The association between the BoHA Percentage difference between hands and mean activity asymmetry index is displayed in . There was a significant, strong positive correlation between the BoHA Percentage difference between hands and the mean activity asymmetry index (B = 0.95, 95%CI: 0.75,1.15, p < 0.001; β = 0.83).
Discussion
The BoHA is the only observational-based assessment of upper limb activity performance for children with bilateral CP (Burgess et al., Citation2019). This study demonstrates further evidence of construct validity for the BoHA using hypotheses testing about the relationship of BoHA scores with accelerometer activity counts. In support of Hypothesis 1, 3 and 4, there was a moderately strong positive association between BoHA Units and total mean activity (H1), a moderately strong positive association between BoHA Each-Hand sub-score and mean activity count for the non-dominant hand (H3), and a strong, positive correlation between BoHA Percentage difference between hands and mean activity asymmetry index (H4).
Hypothesis 2 was not supported, as for the dominant hand there was a weak, non-significant association between BoHA Each-Hand sub-score and mean activity. This result is consistent with previous findings, as BoHA Units have been found to have a strong correlation with the Melbourne Assessment 2 and the Box and Blocks Test for the non-dominant hand, but moderate correlations with these measures for the dominant hand (Elvrum et al., Citation2022). It was suggested that this may have been due to less variability in Melbourne Assessment 2 scores and the fact that bimanual performance is dependent on the degree of limitation in the movement of the non-dominant hand, not just how well the dominant hand performs (Elvrum et al., Citation2022).
In this present study using accelerometers, we suggest that the lack of correlation between the BoHA Each-Hand sub-score and mean activity for the dominant hand may be due to the measurement properties of wrist worn accelerometers. The primary tasks of the non-dominant hand in bimanual performance are movements that are detected by accelerometers such as reaching for, and stabilizing objects, and this is confirmed by the strong correlation between the BoHA Each-Hand sub-score and mean activity for the non-dominant hand. The dominant hand, however, often performs fine motor manipulation with the fingers. These small finger movements are not detected by the accelerometers situated on the wrist, but they do contribute toward a higher BoHA Each-Hand sub-score. For example, children with decreased fine motor skills were observed to sort cards by placing each card individually onto the table, rather than manipulating the cards within their hands. Sorting the cards in this manner leads to a lower BoHA Each-Hand score but higher activity count. In contrast, children with effective fine motor skills who were observed to use in-hand manipulation to sort the cards, received a higher BoHA Each-Hand sub-score but lower activity count.
Greater variability in the use of the dominant hand may also be a contributing a factor to the lack of correlation between the BoHA Each-Hand sub-score and mean activity for the dominant hand, as children classified in MACS levels II and III may use their dominant hand to compensate for decreased use or neglect of the more affected hand. For example, participants were observed to reach across the table with their less affected hand to grasp an object on their more affected side rather than use their more affected hand. This compensatory use of their less affected hand increased the activity counts for the dominant hand. Children with efficient and effective upper limb movement (MACS I) were observed to reach and grasp objects with less overreaching, under reaching, fumbling, and dropping of objects, and so received higher BoHA score but a lower activity count.
Other studies have investigated the relationship between upper limb functioning or capacity and wrist-worn accelerometry in children with CP. One study examined the utility of activity counts to evaluate the difference in performance between the dominant and non-dominant hands of 50 children and young people with unilateral CP undertaking the AHA (Beani et al., Citation2019). Our data mirrors the findings from this study, showing a gradient in both mean activity and asymmetry index for the non-dominant hand according to MACS level (Beani et al., Citation2019). This demonstrates that in children with both unilateral and bilateral CP, reduced upper limb function is related to increased asymmetry, quantifiable by both assessments of upper limb activity and device-based objective measures. The relationship between a different accelerometer-derived outcome, peak acceleration, and other validated upper limb activity assessments including the Jebsen Taylor Hand Function Test, the Quality of Upper Extremity Skills Test, and the Box and Blocks Test was investigated in 15 children with unilateral and bilateral CP (Kim et al., Citation2018). In this study, peak acceleration has a moderate-to-strong correlation with upper limb activity capacity and demonstrated excellent test-retest reliability.(Kim et al., Citation2018) Peak acceleration was also significantly different between the dominant and non-dominant hands (Kim et al., Citation2018).
Limitations of this study should be considered. A limitation of testing construct validity of the BoHA with activity counts from wrist worn accelerometers is that the accelerometer can only measure gross upper limb movement, not fine finger movements. Additionally, accelerometers capture the frequency and intensity of movement rather than the quality of the movement. Over-reaching, inaccurate, inefficient, or involuntary movements which are scored down on the BoHA, are ‘counted’ by an accelerometer, and accelerometers may have limited applicability in children with dystonia depending on the type of dystonia and their level of non-voluntary movements. Another limitation of this validity study is that the BoHA and accelerometry are tools which sit under different components of the International Classification of Functioning, Disability and Health—Children and Youth (World Health Organization, Citation2007). The BoHA is a measure of activity performance, while accelerometers on the wrists measure movement of the arms and may be considered to fall under the ICF category of Body Functions and Structures (‘Control of voluntary movement -b760) (World Health Organization, Citation2007). However, as measurement occurred during the BoHA play session, we consider the accelerometry to be a measure of body function during activity performance, and a credible method to test validity of the BoHA, particularly as an indicator pertaining to upper limb asymmetry. Future studies which examine construct validity may wish to examine the relationship between the BoHA and another measure of upper-limb activity performance, such as the ABILHAND-Kids.
Conclusion
This study provides further evidence of construct validity for the BoHA as a measure of upper limb activity performance in children with bilateral CP aged 6–12 years of age, classified as GMFCS I-IV. Three of the four hypotheses regarding the expected relationship between the BoHA and accelerometry were supported. There were significant, positive associations between the overall BoHA Units and the total mean activity, asymmetry in upper limb use as measured by the BoHA and accelerometer, and the BoHA Each-Hand sub-score and mean activity count for the non-dominant hand. The lack of association between the BoHA Each-Hand sub-score and mean activity count for the dominant hand may be reflective of the discrepancy between the information which is captured by the BoHA and what is measured by wrist-worn accelerometers, rather than concerns around the BoHA measure itself.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data of this study are available on request from the authors.
Additional information
Funding
Notes on contributors
Andrea Burgess
Andrea Burgess is an occupational therapist and postdoctoral research fellow at the Queensland Cerebral Palsy & Rehabilitation Research Centre at The University of Queensland. Her research has focused on examining the effectiveness of interventions and the development of self-care and motor skills in children with cerebral palsy.
Stina Oftedal
Stina Oftedal is a dietitian and Postdoctoral Research Fellow at the Queensland Cerebral Palsy Rehabilitation Research Centre at the University of Queensland. Her research interests include exploring how nutritional status and physical activity impact health outcomes in children with cerebral palsy.
Roslyn N. Boyd
Roslyn N. Boyd is Professor of Cerebral Palsy Research at the Queensland Cerebral Palsy and Rehabilitation Research Centre the Faculty of Medicine at the University of Queensland. Prof Boyd’s research focuses on the early detection and early intervention for infants with Cerebral Palsy in high and low resource settings.
Sarah Reedman
Sarah Reedman is a physiotherapist and research fellow at the Queensland Cerebral Palsy & Rehabilitation Research Centre at The University of Queensland. Her research spans participation-focused intervention, adapted physical activity and intensive functional motor rehabilitation for children with cerebral palsy.
Stewart G. Trost
Stewart G. Trost is Professor in Allied Health Research, a conjoint position with Children’s Health Queensland and The University of Queensland. His research is focussed on the use of wearable sensors to measure health outcomes in children and adults living with disability.
Robert S. Ware
Robert S. Ware is Professor of Biostatistics at Menzies Health Institute Queensland, Griffith University. Prof Ware is a methodologist and clinical statistician whose research focuses on improving the health and quality of life of people with developmental and intellectual disabilities.
Leanne Sakzewski
Leanne Sakzewski is an Associate Professor at the Queensland Cerebral Palsy and Rehabilitation Research Centre at The University of Queensland. Her research focuses on novel interventions to improve motor, social and participation outcomes of infants, children and adolescents with cerebral palsy and acquired brain injuries.
References
- Beani, E., Maselli, M., Sicola, E., Perazza, S., Cecchi, F., Dario, P., Braito, I., Boyd, R., Cioni, G., & Sgandurra, G. (2019). Actigraph assessment for measuring upper limb activity in unilateral cerebral palsy. Journal of NeuroEngineering and Rehabilitation, 16(1), 30. https://doi.org/10.1186/s12984-019-0499-7
- Boyd, R. N., Davies, P. S. W., Ziviani, J., Trost, S., Barber, L., Ware, R., Rose, S., Whittingham, K., Sakzewski, L., Bell, K., Carty, C., Obst, S., Benfer, K., Reedman, S., Edwards, P., Kentish, M., Copeland, L., Weir, K., Davenport, C., … Scuffham, P. A. (2017). PREDICT-CP: Study protocol of implementation of comprehensive surveillance to predict outcomes for school-aged children with cerebral palsy. BMJ Open, 7(7), e014950. https://doi.org/10.1136/bmjopen-2016-014950
- Boyd, R. N., Jordan, R., Pareezer, L., Moodie, A., Finn, C., Luther, B., Arnfield, E., Pym, A., Craven, A., Beall, P., Weir, K., Kentish, M., Wynter, M., Ware, R., Fahey, M., Rawicki, B., McKinlay, L., & Guzzetta, A. (2013). Australian Cerebral Palsy Child Study: Protocol of prospective population based study of motor & brain dev. of preschool CP. BMC Neurology, 13(1), 13–57. https://doi.org/10.1186/1471-2377-13-57
- Braito, I., Maselli, M., Sgandurra, G., Inguaggiato, E., Beani, E., Cecchi, F., Cioni, G., & Boyd, R. (2018). Assessment of upper limb use in children with typical development and neurodevelopmental disorders by inertial sensors: A systematic review. Journal of NeuroEngineering and Rehabilitation, 15(1), 94. https://doi.org/10.1186/s12984-018-0447-y
- Burgess, A., Boyd, R. N., Chatfield, M. D., Ziviani, J., & Sakzewski, L. (2021). Hand Function in 8- to 12-Year-Old Children with Bilateral Cerebral Palsy and Interpretability of the Both Hands Assessment. Physical & Occupational Therapy in Pediatrics, 41(4), 358–371. https://doi.org/10.1080/01942638.2020.1856286
- Burgess, A., Boyd, R. N., Ziviani, J., & Sakzewski, L. (2019). A systematic review of upper limb activity measures for 5‐ to 18‐year‐old children with bilateral cerebral palsy. Australian Occupational Therapy Journal, 66(5), 552–567. https://doi.org/10.1111/1440-1630.12600
- de Vet, H. C., Terwee, C. B., Mokkink, L. B., & Knol, D. L. (2011). Measurement in Medicine. Cambridge University Press.
- Eliasson, A. C., Krumlinde-Sundholm, L., Rosblad, B., Beckung, E., Arner, M., Ohrvall, A. M., & Rosenbaum, P. (2006). The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Developmental Medicine and Child Neurology, 48(7), 549–554. https://doi.org/10.1017/S0012162206001162
- Elvrum, A. G., Johansen, G. O., Vik, T., & Krumlinde-Sundholm, L. (2022). External validity of the Both Hands Assessment for evaluating bimanual performance in children with bilateral cerebral palsy. Developmental Medicine & Child Neurology, 64(5), 586–592. https://doi.org/10.1111/dmcn.15127
- Elvrum, A. G., Zethræus, B.-M., Vik, T., & Krumlinde-Sundholm, L. (2018). Development and Validation of the Both Hands Assessment for Children With Bilateral Cerebral Palsy. Physical & Occupational Therapy in Pediatrics, 38(2), 113–126. https://doi.org/10.1080/01942638.2017.1318431
- Gilmore, R., Sakzewski, L., & Boyd, R. (2010). Upper limb activity measures for 5- to 16-year-old children with congenital hemiplegia: A systematic review. Developmental Medicine and Child Neurology, 52(1), 14–21. https://doi.org/10.1111/j.1469-8749.2009.03369.x
- Kim, D. H., An, D.-H., & Yoo, W.-G. (2018). Measurement of upper limb movement acceleration and functions in children with cerebral palsy. Technology and Health Care : official Journal of the European Society for Engineering and Medicine, 26(3), 429–435. https://doi.org/10.3233/THC-171148
- Klevberg, G. L., Elvrum, A. G., Zucknick, M., Elkjaer, S., Østensjø, S., Krumlinde-Sundholm, L., Kjeken, I., & Jahnsen, R. (2018). Development of bimanual performance in young children with cerebral palsy. Developmental Medicine and Child Neurology, 60(5), 490–497. https://doi.org/10.1111/dmcn.13680
- Krumlinde-Sundholm, L., & Eliasson, A-c (2003). Development of the Assisting Hand Assessment: A Rasch-built Measure intended for Children with Unilateral Upper Limb Impairments. Scandinavian Journal of Occupational Therapy, 10(1), 16–26. https://doi.org/10.1080/11038120310004529
- Mokkink, L. B., Terwee, C. B., Patrick, D. L., Alonso, J., Stratford, P. W., Knol, D. L., Bouter, L. M., & de Vet, H. C. W. (2010). The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. Journal of Clinical Epidemiology, 63(7), 737–745. https://doi.org/10.1016/j.jclinepi.2010.02.006
- Occupational Therapy Australia (2019). Evidence-based practice position statement. https://www.otaus.com.au/sitebuilder/advocacy/knowledge/asset/files/21/ebppositionstatement.pdf
- Oldfield, R. C. (1971). The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychologia, 9(1), 97–113. https://doi.org/10.1016/0028-3932(71)90067-4
- Palisano, R. J., Rosenbaum, P., Bartlett, D., & Livingston, M. H. (2008). Content validity of the expanded and revised Gross Motor Function Classification System. Developmental Medicine and Child Neurology, 50(10), 744–750. https://doi.org/10.1111/j.1469-8749.2008.03089.x
- Rosenbaum, P., Paneth, N., Leviton, A., Goldstein, M., Bax, M., Damiano, D., Dan, B., & Jacobsson, B. (2007). A report: The definition and classification of cerebral palsy April 2006. Dev Med Child Neurol, 109(Supp), 8–14.
- Rosenbaum, P. L., Palisano, R. J., Bartlett, D. J., Galuppi, B. E., & Russell, D. J. (2008). Development of the Gross Motor Function Classification System for cerebral palsy. Developmental Medicine and Child Neurology, 50(4), 249–253. https://doi.org/10.1111/j.1469-8749.2008.02045.x
- Sakzewski, L., Bleyenheuft, Y., Boyd, R. N., Novak, I., Elliott, C., Reedman, S., Morgan, C., Pannek, K., Fripp, J., Golland, P., Rowell, D., Chatfield, M., & Ware, R. S. (2019). Protocol for a multisite randomised trial of Hand–Arm Bimanual Intensive Training Including Lower Extremity training for children with bilateral cerebral palsy: HABIT-ILE Australia. BMJ Open, 9(9), e032194. https://doi.org/10.1136/bmjopen-2019-032194
- Schober, P., Boer, C., & Schwarte, L. A. (2018). Correlation Coefficients: Appropriate Use and Interpretation. Anesthesia & Analgesia, 126(5), 1763–1768. https://doi.org/10.1213/ANE.0000000000002864
- Surveillance of Cerebral Palsy in Europe. (2000). Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys and registers (SCPE). Developmental Medicine & Child Neurology, 42(12), 816–824.
- World Health Organization (2007). International classification of functioning, disability, and health: Children & youth version: ICF-CY. World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/43737/9789241547321_eng.pdf