ABSTRACT
Purpose
Goal setting is an essential rehabilitation activity. However, multidisciplinary rehabilitation staff goal-setting practice with stroke survivors with aphasia and associated training needs are not well understood.
Methods
We designed, piloted, and conducted a survey of stroke rehabilitation staff in the UK, Australia, Aotearoa New Zealand, Canada, Ireland. Analysis included descriptive statistics, chi-square and Fisher’s exact tests, and qualitative content analysis.
Results
We received 251 responses from 118 SLTs and 133 non-SLTs. Most reported setting goals with most or all people with aphasia (78%, 197/251); 57% (138/244) rarely or never provided an accessible copy of goals. All disciplines reported significantly less confidence setting goals with people with aphasia than without aphasia (p = 0.012, n = 119). Barriers to goal setting included the communication impairment (especially severe aphasia) and poor insight. Staff described feeling ill-equipped to support people with aphasia in goal setting; only 27% (67/251) had accessed training to do so.
Conclusions
Rehabilitation staff described involving stroke survivors with aphasia in goal setting but lacked confidence doing so and receive inadequate training and support. Training should target multidisciplinary staff confidence and communication support strategies and resources so that people with aphasia and families are supported as goal-setting partners.
Introduction
Access to adequate rehabilitation is recognised as a human right by the World Health Organisation (Citation2011). Rehabilitation services must therefore be available to all who require it, including stroke survivors with aphasia, who require accessible communication options to participate in decisions about their rehabilitation. Goal setting is a key process in which these decisions are made and is recommended in stroke rehabilitation guidelines internationally (Clinical Centre for Research Excellence in Aphasia Rehabilitation, Citation2014; Green & Maddula, Citation2018; Heart and Stroke Foundation, Citation2018; Irish Heart Foundation: Council for Stroke, Citation2010; National Institute for Health and Care Excellence, Citation2013; NHS England, Citation2015; Royal College of Physicians, Citation2016; Stroke Foundation, Citation2017). As such, stroke survivors with aphasia have a right to be supported to take part in the goal-setting process. Person-centred goal-setting practice (Leach et al., Citation2010; Levack et al., Citation2006; Playford et al., Citation2009) ensures that goals address what is important to stroke survivors and their families (Bright et al., Citation2012; Leach et al., Citation2010). As well as supporting patient engagement (Kang et al., Citation2021), person-centred goal setting practice can enhance patient motivation, shared decision making, and functional outcomes in rehabilitation (2017). If stroke survivors with aphasia are not supported to express their personal goals, rehabilitation activities, and interventions may not address their priorities, needs, and preferences, thus compromising their ongoing recovery and wellbeing.
Rehabilitation staff consistently report communication impairment as a barrier to collaborative goal-setting practice (Plant & Tyson, Citation2018; Rosewilliam et al., Citation2011; Sugavanam et al., Citation2013). Our recent narrative review of communication accessibility revealed a lack of evidence-based interventions and strategies to support accessible goal-setting practice for stroke survivors with aphasia (Brown et al., Citation2021). In a UK-wide survey of community rehabilitation teams, goal-setting practice was highly variable, and involvement of patients with communication and cognitive impairment was reported as a moderate or low priority by 17% of teams (Scobbie et al., Citation2015). Evidence suggests that rehabilitation staff (both SLT and non-SLT) lack confidence supporting stroke survivors with aphasia in hospital settings (Cameron et al., Citation2018); however, the specific relationship between multidisciplinary staff confidence and goal-setting practice with stroke survivors with aphasia is unknown.
Although international rehabilitation guidelines recommend that multidisciplinary teams receive training to support people with aphasia (Clinical Centre for Research Excellence in Aphasia Rehabilitation, Citation2014; Green & Maddula, Citation2018; Heart and Stroke Foundation, Citation2018; Irish Heart Foundation: Council for Stroke, Citation2010; National Institute for Health and Care Excellence, Citation2013; NHS England, Citation2015; Royal College of Physicians, Citation2016; Stroke Foundation, Citation2017) and evidence suggests that training is beneficial (Coulter et al., Citation2015; Horton et al., Citation2016; Jensen et al., Citation2015; Simmons-Mackie et al., Citation2007), there remains a dearth of information internationally on the training and support required and received by multidisciplinary rehabilitation staff to support stroke survivors with aphasia to take part in collaborative goal setting.
To address this evidence-training-practice gap, we conducted a multinational survey of multidisciplinary rehabilitation staff goal-setting practice with stroke survivors with aphasia and their training needs. The survey aimed to investigate:
Rehabilitation staff goal-setting practices with stroke survivors with aphasia;
Barriers and facilitators to goal setting with stroke survivors with aphasia;
Confidence in goal setting with stroke survivors with and without aphasia;
Experiences of accessible goal-setting training and further training needs.
Materials and methods
Reporting guidelines
No consensus survey reporting guidelines are currently available. We referred to the Checklist for Reporting Results of Internet E-Surveys (CHERRIES; Eysenbach, Citation2004), including recent additions from Turk et al. (Citation2018) to support transparent reporting of this survey. Specifically designed to support reporting of online surveys, it is cited on the Equator Network as the relevant reporting guideline for surveys.
Study design
We designed a bespoke online survey using the Smart Survey® platform to collect information from rehabilitation staff from five English-speaking countries with broadly similar public health systems. We conducted a survey, as opposed to more in-depth methods, such as interviews or focus groups, to facilitate large-scale collection of data across these countries and determine patterns across different disciplines. The survey covered the following topic areas: (i) demographic information (i.e., clinical role, experience working with people with aphasia, team type, and other roles in the team), (ii) goal-setting practice with stroke survivors with aphasia, including tools and adaptations used to support stroke survivors with aphasia to communicate and participate in goal setting, (iii) confidence when goal setting with stroke survivors with and without aphasia, (iv) barriers and facilitators to goal setting with stroke survivors with aphasia, (v) experiences of training and education for communicating and goal setting with stroke survivors with aphasia, and (vi) training and education needs.
Development of the survey was informed by information gaps identified in the previous literature on goal setting and accessible communication (Brown et al., Citation2021; Cameron et al., Citation2018; Scobbie et al., Citation2015). Scobbie et al.’s previous UK-wide survey (2015) of goal-setting practice in community rehabilitation settings was used to develop questions about usual goal-setting practice with stroke survivors with aphasia. Questions were adapted to ensure they were relevant to stroke survivors with aphasia, for example, we asked about whether staff provided “an accessible copy of the person’s goals” (instead of “a copy of the person’s goals” as used in Scobbie et al.’s survey). Confidence questions were included based on Cameron et al.’s (Citation2018) Australian questionnaire, which asked healthcare professionals to rate their confidence when communicating with people with aphasia on a visual analogue scale (VAS). Our survey adapted the VAS into a Likert scale, and respondents were asked to rate their confidence in goal setting with stroke survivors with and without aphasia to establish any differences specific to goal setting.
The survey consisted predominantly of closed questions to increase the likelihood of completed responses, as odds of response have been found to decrease by more than half with the inclusion of open-ended questions (Edwards et al., Citation2009). However, free text boxes were used some questions to capture more in-depth responses. Most questions on goal-setting practice contained multiple-response options to capture the range of relevant experiences and behaviours that are likely to occur.
The survey, including participant information, was piloted in a two-stage process. First, stroke researchers from different rehabilitation disciplines (n = 5) provided feedback on the wording of questions, survey format, completion time, and usability. A revised version of the survey was then piloted with rehabilitation professionals from healthcare settings in each of the target countries (n = 6), including one occupational therapist, one physiotherapist, three speech, and language therapists (SLTs), and one rehabilitation assistant. The survey was further refined based on feedback given, and a final version of the survey was approved by the project team prior to distribution (Supplementary file 1).
Sample and inclusion criteria
Rehabilitation staff who were (a) currently working in any rehabilitation setting with stroke survivors on their caseload, (b) involved in delivering goal setting with any stroke survivors, (c) located in the UK, Ireland, Canada, Aotearoa New Zealand, or Australia, and (d) able to participate in a survey conducted in English were eligible to complete the survey. Rehabilitation staff typically represented in rehabilitation teams and likely to be involved in goal setting were targeted. This included SLTs, occupational therapists, physiotherapists, clinical or neuropsychologists, and other staff such as rehabilitation assistants, nurses, and dieticians, who may be involved in goal setting (Scobbie et al., Citation2015). Target countries included the UK, Ireland, Australia, Aotearoa New Zealand, and Canada, as they (a) are mainly English-speaking and (b) have similar public stroke rehabilitation services. Other countries were not targeted for recruitment as translations of the survey and the resulting data were not feasible. The target sample was a minimum of 200 completed returns, with no upper limit.
Recruitment strategy and ethical approval
Rehabilitation staff were recruited via (a) professional networks and special interest groups within the target countries and (b) social media. Participation was open to anyone meeting the inclusion criteria and was not restricted by invitation. We emailed 30 professional network and special interest groups about the survey, and 25 of these agreed to distribute the survey information to their membership via mailing lists, websites, and/or social media. Participants were provided with detailed information about the study and gave informed consent via the survey landing page. To ensure full anonymity of responses, no identifying information (including IP address) was collected or stored. Ethical approval was obtained from the School of Health and Life Sciences Research Ethics Committee at Glasgow Caledonian University prior to recruitment [HLS/NCH/19/060].
Data collection and analysis
The survey was distributed and live for a period of 6 weeks between August and October 2020. Email reminders were sent after 4 weeks by 11 of the 25 participating networks, and regular reminders to take part were posted by the project team and shared with colleagues on Twitter. The data were imported to the Statistical Package for Social Sciences (SPSS) v26. We analysed closed responses using descriptive statistics and inferential statistics, including the chi-square test of independence and Fisher’s exact test to compare relationships between responses from respondent sub-groups (e.g., confidence ratings from different rehabilitation disciplines). The chi-square test was used in the first instance, with Fisher’s exact test used if chi-square analysis was not possible (e.g., due to low cell count).
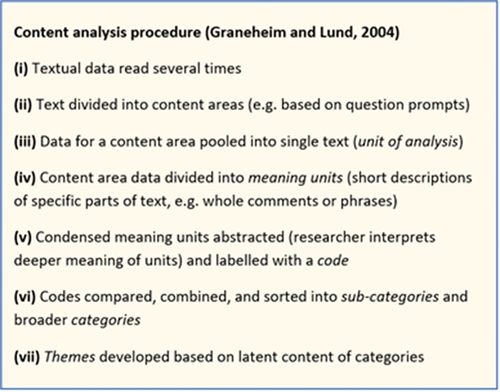
Open-ended responses were analysed by one researcher [EB] using qualitative content analysis (Graneheim & Lundman, Citation2004), which was used due to its suitability for small quantities of focused data typically captured in surveys. Inductive content analysis (Graneheim & Lundman, Citation2004) was used to identify meaning units, codes, sub-categories, categories, and themes. Data were pooled from open-ended responses on confidence, barriers, and facilitators and analysed inductively as per the procedure detailed in below. Sub-categories, categories, and themes were reviewed and discussed with the fourth author [LS].
Results
Quantitative results
Response rate and demographics
A total of 303 healthcare professionals responded to the survey. Of these, 52 provided demographic data only. A total of 251 responses (220 complete and 31 partials) were included in the analysis. As social media was used to distribute the survey, and some professional networks included members outside the target group, a definitive response rate could not be calculated. A completion rate of 73% was instead calculated based on the CHERRIES reporting guidelines, achieved by dividing the number of complete responses by the total number of responses (220/303).
The UK and Aotearoa New Zealand returned the highest number of responses. Across all countries, most respondents were SLTs (). Respondents worked in a range of hospital and community settings and most reported having more than 10 years of experience working with stroke survivors in rehabilitation. The vast majority of respondents worked in multidisciplinary teams; occupational therapists, physiotherapists, SLTs, nurses, and rehabilitation assistants were the most common roles represented in teams. The majority of respondents had an SLT on their team, but one third did not.
Table 1. Respondent demographics; total responses: n = 251.
Most respondents (43%, 107/251) reported a mixed patient group on their caseload (e.g., people with stroke, musculoskeletal conditions) or a neurological patient group (39%, 98/251; e.g., people with stroke, multiple sclerosis;). A minority of respondents (18%, 46/251) reported a stroke-specific caseload. For the majority of respondents (81%, 203/251), stroke survivors with aphasia made up more than 10% of their caseload.
Goal setting practice with stroke survivors with aphasia
Extent of goal setting with stroke survivors with aphasia: The majority of respondents reported setting goals with most or all stroke survivors with aphasia (). Most respondents who did not set goals with any stroke survivors with aphasia were rehabilitation assistants.
Goal-setting methods: Goal setting methods used were highly varied (). Respondents most often reported using SMART goals or no method at all when goal setting with stroke survivors with aphasia.
Table 2. Goal-setting methods* used with stroke survivors with aphasia.
Goal-setting activities: Respondents (n = 244) who indicated that they set goals with stroke survivors with aphasia rated how frequently they engaged in specific goal setting activities (). The most commonly reported activities were determining stroke survivors’ goal priorities and setting goals that were personally meaningful to patients and families. The least commonly reported activities were giving stroke survivors with aphasia accessible information about the goal setting approach, breaking goals down into action plans (or steps), and supporting people with aphasia to adjust or disengage from goals proving too difficult to achieve.
Communication tools and resources to support goal setting: Talking Mats were the most popular tool reported to support goal setting with stroke survivors with aphasia (41%, 100/244), followed by tools developed by respondents or their teams (34%, 83/244) and communication apps (28%, 68/244). The majority of Talking Mats users were SLTs (61%, 61/100). One-quarter of respondents did not use any tools or resources (26%, 63/244).
Communication strategies: Three communication strategies were used by 90% or more of respondents to support goal setting with stroke survivors with aphasia: checking that the stroke survivor had understood (97%, 237/244), using simple language (95%, 232/244), and checking that they had understood the stroke survivor with aphasia (93%, 226/244). The least reported strategy was providing information about goal setting in advance to the stroke survivor with aphasia (11%, 26/244). SLTs are reported using significantly more strategies than non-SLTs (p = <.001, n = 244).
Confidence in goal setting with stroke survivors with aphasia
The vast majority of respondents (92%, 228/248) reported being mostly or very confident in goal setting with stroke survivors without aphasia (). Confidence levels were lower when setting goals with stroke survivors with aphasia, with around half of respondents reporting that they were mostly or very confident (47%, 117/248).
Fisher’s exact test was used on grouped confidence ratings (0–3: not at all to somewhat confident; 4–5: mostly to very confident). Respondents reported significantly lower confidence with stroke survivors with aphasia than without aphasia (p = .012, n = 119). Chi-square results showed a significant difference between confidence among SLTs and non-SLTs when goal setting with stroke survivors with aphasia (p = .000, n = 248). Sixty-one percent (70/115) of SLTs was mostly to very confident (rating of 4–5), compared to 35% (47/113) of non-SLTs. Receiving training on goal setting with stroke survivors with aphasia was associated with significantly higher confidence (p = ,010, n = 132).
Barriers to goal setting with stroke survivors with aphasia
Respondents (n = 237) reported a range of barriers to setting goals with stroke survivors with aphasia (). The most frequently reported was the communication impairment and family members controlling conversations or speaking for the stroke survivor with aphasia. Barriers external to the stroke survivor with aphasia and their family were less frequently reported, including the goal-setting process being time consuming, staff not receiving adequate training, and lack of confidence.
Facilitators of goal setting with stroke survivors with aphasia
The most accessed facilitators were knowledge of strategies to support communication with stroke survivors with aphasia, support, or involvement from family members or community, and support or advice from the treating SLT or other more experienced SLTs (). Access to communication resources or accessible information was reported as a facilitator by more SLTs than non-SLTs (SLT 62%, 81/112; non-SLT 38%, 50/125). In contrast, more non-SLTs than SLTs reported access to support and advice from an SLT (SLT 26%, 43/112; non-SLT 71%, 103/125).
Training and education
Generic goal-setting training: Most respondents (70%, 165/234) had received training or education to set goals in rehabilitation with any patients. Developing targeted goals (e.g., SMART goals) were the most common training topic, followed by using a goal-setting method such as COPM or GAS (). The most common source of training was the workplace.
Table 3. Reported topics in training received on generic goal setting, aphasia-specific goal setting, and communication skills.
Aphasia-specific goal-setting training: Of the 66% (165/234) of respondents who had received training on goal setting with any patients, nearly half (41%, 67/165) had also received training on supporting stroke survivors with aphasia to take part in goal setting. Communication strategies and how to make written information accessible were the most common topics. Training was most often sourced through the workplace. Chi-square test results showed that significantly more SLTs than non-SLTs had accessed training to support goal setting with stroke survivors with aphasia (p = .000, n = 159). Respondents who had accessed this training also reported significantly fewer barriers than those who had not received it (p = 0.05, n = 159).
Communication skills: Two-thirds of respondents (70%, 160/227) had received training on supporting communication with stroke survivors with aphasia (not specific to goal setting). Strategies for communicating with stroke survivors with aphasia and information about aphasia and how it impacts on communication were the most common topics. The workplace was the most common source of training. Chi-square results showed that significantly more SLTs than non-SLTs had accessed communication training (p = .000, n = 227). Staff who had accessed communication training also reported significantly fewer barriers than staff who had not accessed training (p = .000, n = 227).
Training preferences: Despite lack of training being a less frequently reported barrier than stroke survivor factors (e.g., aphasia and family), most respondents (88%, 220/251) wanted to receive further training or education on supporting stroke survivors with aphasia to participate in goal setting. Respondents who did not want further training gave a range of reasons, such as having received sufficient training but lacking resources and time, already feeling fully qualified as an SLT to support goal setting, and limited opportunities to apply practice due to a hyperacute caseload. Strategies and resources to support stroke survivors with severe aphasia (76.4%, 168/220), how to use communication support tools (59.1%, 130/220), and goal-setting methods (e.g., GAS or G-AP; 56.4%, 124/220) were the most preferred training topics (). The most popular methods for receiving training were workshops (76%, 167/220) and videos demonstrating strategies (72%, 159/220).
Qualitative results
Three themes were developed from the analysis of 92 pooled open responses from 58 respondents: it depends on the stroke survivor; involving the stroke survivor, family, and others is challenging but important; and working environment makes a difference.
It depends on the stroke survivor
A generally held view was that goal setting is more challenging with stroke survivors with aphasia and that aphasia itself is a barrier (). For example, aphasia made it harder to explain the goal-setting process and discuss stroke survivors’ goal preferences and needs. Aphasia presentation determined how challenging goal setting could be. For example, receptive, global, and severe aphasia were highlighted as particularly difficult, with those stroke survivors needing more support.
Table 4. Theme 1 summary: It depends on the stroke survivor.
Issues beyond aphasia also affected goal setting. Emotional and psychological readiness for goal setting included stroke survivors with aphasia struggling to “accept a prognosis” or not feeling ready to start goal setting. One SLT highlighted the challenges of getting the timing right in rehabilitation:
Sometimes rehabilitation is provided at a set time in someone’s recovery, and it’s not always at the right time for them. I’ve worked with people who are ready to set goals only a few days after their stroke. But sometimes I’ve found that an individual may be ready much later in their journey … health services are not flexible enough to accommodate this, and so sadly some people with aphasia miss out on the rehabilitation that they could have benefitted from. (P16, SLT, ANZ)
This SLT went on to reflect on how this could have an emotional impact both on the stroke survivor with aphasia and the rehabilitation staff member:
Sometimes this is also clouded by a deep sense of failure when the person with aphasia has been involved in a poorly-timed or poorly-executed period of rehabilitation, and then that reinforced the perception that they can’t/won’t improve. I’m deeply saddened when I meet those individuals. (P16, SLT, ANZ)
Staff also reported medical and cognitive issues determining stroke survivors’ readiness for goal setting. Poor insight into impairments was considered challenging when negotiating goals. Similarly, stroke survivors just wanting to “get better” could find it challenging to express their goals or understand the need for specific plans.
Involving the stroke survivor, others, and family is challenging but important
Using a person-centred approach involved building rapport and understanding patient context (). Staff felt it was important to take time to build relationships with stroke survivors with aphasia, understand their communication history and find the right approach for each patient. However, they found communicating about goal setting challenging because it includes abstract concepts that could be difficult to communicate. Some respondents also had concerns about unintentionally leading stroke survivors with aphasia towards goals that were not their own priorities.
Table 5. Theme 2 summary: Involving stroke survivors, family, and others is challenging but important.
It was believed that working with families can help or hinder. Respondents recognised that family could be an important facilitator, knowing about the stroke survivor’s personal history and communication needs. However, family could at times bring their own agenda or speak for the stroke survivor with aphasia. Staff emphasised that this needed to be managed carefully to prioritise the stroke survivor’s own views and needs. Family acting as interpreters was also challenging, as it could be hard to guarantee accurate interpretations from both staff and the stroke survivor with aphasia.
Working environment makes a difference
It was important for staff to have access to quiet setting and communication resources (e.g., picture cards and iPads; ). Team working was recognised as an important facilitator. It was difficult to set multidisciplinary goals without a collaborative approach within the team, but a consistent team approach to goal setting with stroke survivors with aphasia supported staff confidence. Non-SLTs also reported relying on input from SLTs and that their confidence was improved with SLT involvement. Time was a facilitator when present and a barrier when absent. Adequate time for goal-setting sessions with stroke survivors with aphasia was considered highly important but was often limited, for example, in acute settings and when goal setting was expected to be completed in a set number of sessions.
Table 6. Theme 3 summary: Working environment makes a difference.
Key: R = respondent (e.g., R1 = Respondent 1); SLT = speech and language therapist; OT = occupational therapist; PT = physiotherapist; AUS = Australia; UK = United Kingdom; IRE = Ireland; CAN = Canada; ANZ = Aotearoa New Zealand
Discussion
This online multinational survey explored rehabilitation staff goal setting practice with stroke survivors with aphasia, barriers, and facilitators to goal setting, confidence, and training needs. The results largely reflected experiences of rehabilitation staff working in multidisciplinary teams with mixed patient groups, including stroke survivors with aphasia.
Key goal-setting activities are lacking
Reported goal-setting practice with stroke survivors with aphasia in this survey was highly variable and potentially sub-optimal. Providing accessible information about goal setting and an accessible copy of personal goals to stroke survivors with aphasia are fundamental activities within a person-centred, collaborative goal-setting process (Hersh, Worrall et al., Citation2012; Scobbie et al., Citation2015). However, these were among the least reported activities in this survey. Stroke survivors with aphasia rely on accessible information. Work in the area of capacity evaluation demonstrated that accessible information was vital to allow people with aphasia to demonstrate their capacity and provide informed consent (Carling-Rowland et al., Citation2014). Similarly, stroke survivors with aphasia cannot be expected to understand goal setting and communicate their priorities if they lack the information and support to do so.
Our findings also suggest that multidisciplinary staff do not routinely support stroke survivors with aphasia to adjust goals. This is concerning given goal adjustment is often necessary to support ongoing recovery in the first year after stroke (Scobbie, Brady et al., Citation2020). The “evolving” nature of goals has also been highlighted in the SMARTER framework to support person-centred goal setting with people with aphasia (Hersh, Worrall et al., Citation2012). Thus, it is vital that rehabilitation staff recognise the changing nature of goals throughout recovery and support patients to adjust goals, if necessary.
The problem with SMART goals
Goals were most commonly set using SMART goals or informally through discussion with no method. SMART appears to be ubiquitous in clinical education and practice (Hersh, Worrall et al., Citation2012). However, SMART describes target characteristics of individual goals (e.g., Specific and Measurable) and is not a goal-setting method with guided stages. Key stages of the goal setting process (Scobbie et al., Citation2013) may therefore be lacking or delivered sub-optimally, with no consistent approach to negotiating, setting, pursuing, and reviewing goals and progress. This is borne out in the limited delivery of key goal-related activities described above. Staff members using different processes, which may or may not include key goal-related activities, are likely to cause difficulty collaborating across disciplines. The variable and informal approaches reported by respondents risk creating confusion for stroke survivors with aphasia when working with multiple staff. The lack of a consistent, collaborative, and systematic goal setting approach is also likely to make it difficult to adequately evaluate practice and determine how person centred it really is, a vital step towards improving practice. Among SLTs working with people with aphasia, rigid adherence to the SMART acronym has also been associated with more therapist-led goal setting and a more restrictive approach, potentially dismissing patient goals if they do not fit the SMART criteria (Hersh, Sherratt et al., Citation2012).
Inadequate use of communication support tools and strategies
There is a need for greater awareness and provision of communication support tools. Communication support tools have been identified as facilitators for goal setting with stroke survivors with aphasia (Bornman & Murphy, Citation2006; Murphy & Boa, Citation2012; Murphy et al., Citation2005), but our survey revealed respondents reported low use of such tools, which may further contribute to sub-optimal goal setting for stroke survivors with aphasia. In Shrubsole et al.’s (Citation2019) Australian interview study, SLTs also reported a lack of suitable goal-setting resources as a barrier to implementing collaborative goal setting with stroke survivors with aphasia. The reported low use of tools and limited availability is unsurprising, given that in a recent narrative review of accessible goal setting, limited evidence was found describing or evaluating communication support tools in goal setting (Brown et al., Citation2021). It is therefore important that future accessible goal-setting training for staff includes the dissemination of existing communication tools, such as Talking Mats (Talking Mats Ltd, Citation2021) and ParticiPics (Aphasia Institute, Citation2021).
The gap between SLT and non-SLT knowledge of communication strategies is also a concern, with SLTs in this survey reporting significantly more strategies than non-SLTs, who seemed to rely on SLT input to set goals. As a result, stroke survivors with aphasia may not receive consistent communication support across the multidisciplinary team, further reducing their ability to participate in goal setting. Although not specific to goal setting, Cameron et al.’s (Citation2018) survey on the knowledge and confidence of 90 healthcare professionals working with people with aphasia in hospitals also found lower knowledge of strategies among non-SLTs compared to SLTs. This discrepancy in knowledge of strategies is therefore an important gap to be addressed in goal-setting training to ensure that stroke survivors with aphasia receive the same level of support in goal setting regardless of which clinician they work with.
Aphasia as a barrier to goal setting
A finding of this survey, and a theme in the wider goal setting literature (Parsons et al., Citation2018; Plant et al., Citation2016; Rosewilliam et al., Citation2011; Sugavanam et al., Citation2013), is the perception of aphasia or communication impairments as the primary barrier to goal setting, with family involvement also considered potentially problematic (Levack et al., Citation2009; Parsons et al., Citation2018). In previous studies, rehabilitation staff have identified aphasia and family tensions as barriers to goal setting in rehabilitation, but communication impairments are often mentioned incidentally or are not the main focus of goal-setting research (Plant & Tyson, Citation2018; Rosewilliam et al., Citation2011; Sugavanam et al., Citation2013; Van Rijssen et al., Citation2021). Therefore, despite evidence that aphasia is viewed as a barrier to goal setting, there is limited evidence describing how to overcome it in the context of goal setting. If people with aphasia’s rights to communication and adequate rehabilitation are to progress, it is vital that research starts to address why aphasia is still seen as such an insurmountable barrier and exactly how they can be supported in the goal-setting process by multidisciplinary rehabilitation staff.
Rehabilitation staff in this survey and SLTs in Shrubsole et al.’s (Citation2019) interview study reported a range of barriers to goal setting that could impact on the perception of aphasia as a barrier, such as lack of time allocated to goal setting with stroke survivors with aphasia, lack of resources, and lack of consistency and leadership in the multidisciplinary team with goal setting. Facilitators such as an aphasia lead or “champion” and additional time for goal-setting sessions are recommended in studies addressing communication training for staff working with stroke survivors with aphasia (Horton et al., Citation2016; Simmons-Mackie et al., Citation2007). However, our findings suggest limited availability of these facilitators in multidisciplinary stroke rehabilitation practice.
It is therefore vital to begin changing the narrative from aphasia as a barrier to goal setting to aphasia as a common impairment that can be supported by providing staff with training in accessible goal-setting practice and a rehabilitation environment that is designed with aphasia accessibility in mind. If aphasia remains an insurmountable barrier to goal setting, people with aphasia will not receive adequate support to participate in goal setting, and their right to rehabilitation will not be fulfilled.
The impact of confidence
Confidence was significantly lower among all respondents when setting goals with stroke survivors with aphasia compared to stroke survivors without aphasia. This is a key issue, because if staff lack confidence, aphasia may feel like an insurmountable challenge, and goal setting will not be delivered adequately. In Bandura’s social cognitive theory, self-efficacy specifically refers to how confident a person feels in their capacity to achieve goals with barriers and facilitators present (Bandura, Citation1997). It is linked to beliefs about expected performance (Can I do this?) and outcomes (Will doing this result in a positive outcome?). Thus, self-efficacy plays a key role in motivation to engage in a behaviour (Bandura, Citation1997). It then follows that a lack of self-efficacy or confidence in goal setting with stroke survivors with aphasia will result in rehabilitation staff being less motivated to engage in goal-setting activities and attempt communication strategies. While confidence has previously been reported as a barrier by multidisciplinary staff to communicating with people with aphasia, such findings have concerned general hospital interactions (Cameron et al., Citation2018; Carragher et al., Citation2020)). The nature of goal-setting interaction is likely to introduce further complexity. Low confidence risks rehabilitation staff not delivering key goal-setting activities or giving up with a person with aphasia because goal setting is felt to be too challenging.
In our survey, rehabilitation staff reported a range of challenges impacting on their confidence and ability to set goals with stroke survivors with aphasia. Having limited opportunities to practice working with stroke survivors with aphasia because of competing clinical priorities (e.g., dysphagia) has been reported as a reason for lack of confidence (Cameron et al., Citation2018; Shrubsole et al., Citation2019). Although SLTs also reported significantly higher confidence when goal setting with stroke survivors with aphasia compared to non-SLTs, 39% of SLTs rated their confidence as low to moderate. Similarly, in Shrubsole et al.’s (Citation2019) interview study, SLTs’ beliefs about their capabilities influenced their implementation of collaborative goal setting as an aphasia guideline recommendation. This suggests that confidence is a cross-discipline issue and a key influence on staff goal-setting practice. However, it is also complex, and a range of factors can potentially influence confidence. Qualitative findings in our survey suggest that experience and work context play a role in confidence, especially for non-SLTs. For example, staff working in acute settings cited the additional time pressures and medical challenges as impacting on goal setting. It is therefore vital that rehabilitation staff are not only equipped with adequate facilitators to support goal setting with stroke survivors with aphasia but feel confident in their ability to overcome any barriers.
Training is a key unmet need
Our findings show that training to support accessible goal setting with stroke survivors with aphasia is a fundamental unmet need among rehabilitation staff, and its potential role in confidence cannot be ignored. Training has been highlighted as a key pillar in a previous proposed model to support accessible goal-setting practice (Brown et al., Citation2021). Training on goal setting with stroke survivors with aphasia was also associated with significantly higher confidence. However, most rehabilitation staff in our survey had not accessed training specifically on goal setting with stroke survivors with aphasia, and the majority wanted further training. There is then a clear gap between what rehabilitation staff require to make goal-setting accessible and the support they receive to do so.
Appropriate and mandatory training for all staff working with stroke survivors with aphasia is advocated in stroke rehabilitation guidelines (Heart and Stroke Foundation, Citation2018; Irish Heart Foundation: Council for Stroke, Citation2010; National Institute for Health and Care Excellence, Citation2013; NHS England, Citation2015), but participating countries in this survey do not seem to routinely provide communication partner training or accessible goal-setting training to rehabilitation services. The lower confidence among non-SLTs compared to SLTs also suggests gaps in training across disciplines. SLTs are likely to have received more training on communication but still appear to lack specific training on supporting goal setting with stroke survivors with aphasia. Training to support goal setting with stroke survivors with aphasia should therefore be a multidisciplinary endeavour, particularly important given that most respondents worked within multidisciplinary teams.
To change the narrative from aphasia as a barrier to goal setting to creating accessible pathways to goal setting, resources, and training must be developed and made freely available. Our findings indicate a clear desire for further training among multidisciplinary staff, especially on strategies and resources to support stroke survivors with severe aphasia. However, SLTs in Shrubsole et al.’s interview study reported limited opportunities to practice goal setting with survivors with aphasia (Shrubsole et al., Citation2019). In our survey, rehabilitation staff also described being uncertain about which strategies to use with stroke survivors with aphasia. Accessible goal-setting training therefore needs to include more than just knowledge of communication strategies. Training should be experiential, with opportunities to apply skills in practice. In Bird et al.’s (Citation2019) systematic review of 16 randomised controlled trials investigating implementation of stroke rehabilitation evidence, education interventions alone were not enough to improve practice; a combination of education, mentoring, site-specific performance feedback, and local tailoring were needed.
Another example is a recently developed goal-setting package supplement for stroke survivors with aphasia based on the SMARTER framework. Elston et al. (Elston et al., Citation2021) designed training for multidisciplinary staff to use the supplement, which included a manual with information on different communication impairments, a sample script to explain the concept of goal setting and ways to provide support (e.g., communication strategies). A video of a goal-setting session between a stroke survivor with aphasia and a researcher was also included, which addressed key aspects of the goal-setting process according to the package, such as prioritising goals and documenting goals and strategies for working towards goal attainment. This training, found to be acceptable to staff, illustrates the value of designing training specifically for goal setting with people with aphasia.
It is also important to consider how and to whom training is delivered. Training staff should not automatically be the responsibility of SLTs. While SLTs can at times be seen as solely responsible for communication accessibility (Carragher et al., Citation2020)), our findings show that SLTs do not necessarily receive training on communicating or goal setting with stroke survivors with aphasia as part of their qualification. A more suitable model, used successfully by Jensen et al. (Jensen et al., Citation2015) in a communication partner training intervention with staff and people with aphasia, involved training a core group of multidisciplinary staff to act as more experienced practitioners or mentors. This could be applied in an accessible goal-setting training intervention to ensure that all multidisciplinary team members receive the training they need and that goal setting with stroke survivors with aphasia is seen as a shared responsibility.
Implications for clinical practice
This survey’s findings have several implications for accessible goal setting in clinical practice. Accessible goal-setting training for rehabilitation staff should extend beyond knowledge of aphasia and communication strategies. Training should focus on goal-setting scenarios and include ways to apply communication strategies and tools in practice while managing difficult conversations under time pressure. Accessible goal-setting training should also include ongoing support for rehabilitation staff and be linked to practice and service change (Brown et al., Citation2021). Knowledge of aphasia and communication strategies is not enough. Instead of focusing only on individual staff behaviour, training should support services to create a whole environment that supports collaborative accessible goal setting (Brown et al., Citation2021). Staff capacity to implement accessible goal-setting strategies may be limited if service policies do not provide the required infrastructure, including access to resources, enough time to support stroke survivors with aphasia, and a common accessible goal-setting approach within the team.
When implementing accessible goal-setting practice, rehabilitation staff should be supported to collaborate with and consult each other across disciplines. SLTs may not always be available within a team, and assuming responsibility for supporting all other members of staff could create an unmanageable workload. To support staff confidence in setting goals with stroke survivors with aphasia, multidisciplinary teams should have a common approach to goal setting and accessible communication. For example, all staff could use the same goal-setting method, share access to communication resources, and have standard procedures for giving stroke survivors with aphasia-accessible goal-setting information.
Future research
Future training development and evaluation of additional resources to help rehabilitation staff to support stroke survivors with aphasia through the goal-setting process should be a priority. Collaborative, team-based approaches to accessible goal setting should also be evaluated, for example, by exploring the potential of accessible goal setting as an interdisciplinary practice. The cross-disciplinary and collaborative characteristics of interdisciplinary working could be applied to goal setting to ensure that accessible goal-setting methods and strategies are used consistently. Future training should ideally be co-designed with all relevant stakeholders, including rehabilitation staff, stroke survivors with aphasia, and their carers, to harness their expertise and experience. Training evaluation should then be conducted through a feasibility study or pilot randomised control trial, employing measures of staff communicative competence, confidence, and satisfaction with training.
Strengths and limitations
Our survey produced new insights relevant to accessible goal setting with stroke survivors with aphasia. We had a multinational reach and contributed novel comparisons between SLT and non-SLT practice and confidence. Including the frequency of specific goal-setting activities also allowed us to complement and extend earlier findings from Scobbie et al.’s (Scobbie et al., Citation2015) UK-wide survey of multidisciplinary rehabilitation teams by providing unique insights into goal-setting practice with stroke survivors with aphasia.
In addition to its strengths, several limitations must be acknowledged. Although we reached our target completion rate of more than 200 completed responses, our recruitment (August–October 2020) was affected by the COVID-19 pandemic. Healthcare professionals were under significant and unprecedented pressure, and professional networks faced challenges in continuing their regular activity while supporting members’ needs during the pandemic, impacting on survey distribution plans. Online surveys proliferated during this time and “survey fatigue” may have affected the response rate. The disparities between country response figures also prevented comparisons between countries, which may have yielded useful data. While it would have been beneficial to have responses from a wide range of disciplines, respondents mainly included SLTs, occupational therapists, and physiotherapists. Future accessible goal setting research should therefore target other multidisciplinary team members not usually captured in stroke rehabilitation goal-setting research, such as nurses and rehabilitation assistants. Finally, inpatient rehabilitation settings were grouped as a single question response, so survey findings were not differentiated for staff working in acute care settings, who may face different goal-setting challenges compared to those working in sub-acute or rehabilitation units.
Conclusion
Goal-setting practice with stroke survivors with aphasia is embedded in routine practice but is highly variable. Key parts of the process are often reported missing, such as giving patients accessible information about goal setting. SLTs and non-SLTs report experiencing significantly different levels of confidence in goal setting with stroke survivors with aphasia, and staff across disciplines report lower confidence setting goals with stroke survivors with aphasia than those without aphasia. Staff urgently need further training to support goal setting with stroke survivors with aphasia. Future training development should address the limited time and resources available for goal-setting conversations, the perception of aphasia and family involvement as barriers to goal setting, the lack of collaborative and consistent practice within teams, and the need for skills and resources to support stroke survivors with severe aphasia. Training should be adapted for different rehabilitation contexts and accompanied by appropriate service policy and infrastructure to support a consistent approach to accessible goal setting within teams. It is vital that stroke survivors with aphasia receive the support they need to participate in goal setting and fulfil their right to rehabilitation.
APH-PA_21-140-File008.docx
Download MS Word (1.5 MB)Acknowledgments
The authors would like to thank the people with aphasia and rehabilitation staff who gave their time to take part in this study.
Disclosure statement
EB was supported by a Glasgow Caledonian University PhD studentship and Foundation for Women Graduates Foundation grants. LS is supported by a Stroke Association Clinical Lectureship award (TSA LECT 2016/02). The Nursing, Midwifery, and Allied Health Professions Research Unit and MCB are supported by the Chief Scientist Office, Scottish Government Health, and Social Care Directorate, UK. The views expressed here are those of the authors and not necessarily those of the funders.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Aphasia Institute. (2021). ParticiPics. https://www.participics.ca/
- Bandura, A. (1997). Self-efficacy: The exercise of control. W.H. Freeman.
- Bird, M.-L., Miller, T., Connell, L. A., & Eng, J. J. (2019). Moving stroke rehabilitation evidence into practice: A systematic review of randomized controlled trials. Clinical Rehabilitation, 33(10), 1586–1595. https://doi.org/10.1177/0269215519847253
- Bornman, J., & Murphy, J. (2006). Using the ICF in goal setting: Clinical application using Talking Mats®. Disability and rehabilitation. assistive technology, 1(3), 145–154. https://doi.org/10.1080/17483100612331392745
- Bright, F., Boland, P., Rutherford, S., Kayes, N., & McPherson, K. (2012). Implementing a client-centred approach in rehabilitation: An autoethnography. Disability and Rehabilitation, 34(12), 997–1004. https://doi.org/10.3109/09638288.2011.629712
- Brown, S. E., Brady, M. C., Worrall, L., & Scobbie, L. (2021). A narrative review of communication accessibility for people with aphasia and implications for multi-disciplinary goal setting after stroke. Aphasiology, 35(1), 1–32. https://doi.org/10.1080/02687038.2020.1759269
- Cameron, A., McPhail, S., Hudson, K., Fleming, J., Lethlean, J., Tan, N. J., & Finch, E. (2018). The confidence and knowledge of health practitioners when interacting with people with aphasia in a hospital setting. Disability and Rehabilitation, 40(11), 1288–1293. https://doi.org/10.1080/09638288.2017.1294626
- Carling-Rowland, A., Black, S., McDonald, L., & Kagan, A. (2014). Increasing access to fair capacity evaluation for discharge decision-making for people with aphasia: A randomised controlled trial. Aphasiology, 28(6), 750–765. https://doi.org/10.1080/02687038.2014.895975
- Carragher, M., Steel, G., O’Halloran, R., Torabi, T., Johnson, H., Taylor, N. F., & Rose, M. (2020). Aphasia disrupts usual care: the stroke team’s perceptions of delivering healthcare to patients with aphasia, 1(12), 3003–3014 doi:10.1080/09638288.2020.1843079.
- Clinical Centre for Research Excellence in Aphasia Rehabilitation. (2014). Aphasia rehabilitation best practice statements: Comprehensive supplement to the Australian aphasia rehabilitation pathway. http://www.aphasiapathway.com.au/flux-content/aarp/pdf/2014-COMPREHENSIVE-FINAL-01-10-2014-1.pdf
- Coulter, A., Entwistle, V. A., Eccles, A., Ryan, S., Shepperd, S., & Perera, R. (2015). Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database of Systematic Reviews, 3(CD010523). https://doi.org/10.1002/14651858.CD010523.pub2
- Edwards, P. J., Roberts, I., Clarke, M. J., DiGuiseppi, C., Wentz, R., Kwan, I., Cooper, R., Felix, L. M., & Pratap, S. (2009). Methods to increase response to postal and electronic questionnaires. Cochrane Database of Systematic Reviews, 3(MR000008). doi:10.1002/14651858.MR000008.pub4
- Elston, A., Barnden, R., Hersh, D., Godecke, E., Cadilhac, D. A., Lannin, N. A., Kneebone, I., & Andrew, N. E. (2021). Developing person-centred goal setting resources with and for people with aphasia: A multi-phase qualitative study. Aphasiology, 1–20. https://doi.org/10.1080/02687038.2021.1907294
- Eysenbach, G. (2004). Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). Journal of Medical Internet Research, 6(3), e34. https://doi.org/10.2196/jmir.6.3.e34
- Graneheim, U. H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. https://doi.org/10.1016/j.nedt.2003.10.001
- Green, G., & Maddula, M. (2018). New Zealand Stroke Rehabilitation: A strategy. https://strokenetwork.org.nz/new-zealand-stroke-rehabilitation–a-strategy
- Heart and Stroke Foundation. (2018). Canadian stroke best practice recommendations (6th Edition ed.). Heart and Stroke Foundation.
- Hersh, D., Sherratt, S., Howe, T. J., Worrall, L., Davidson, B., & Ferguson, A. (2012). An analysis of the “goal” in aphasia rehabilitation. Aphasiology, 26(8), 971–984. https://doi.org/10.1080/02687038.2012.684339
- Hersh, D., Worrall, L., Howe, T., Sherratt, S., & Davidson, B. (2012). SMARTER goal setting in aphasia rehabilitation. Aphasiology, 26(2), 220–233. https://doi.org/10.1080/02687038.2011.640392
- Horton, S., Lane, K., & Shiggins, C. (2016). Supporting communication for people with aphasia in stroke rehabilitation: transfer of training in a multidisciplinary stroke team. Aphasiology, 30(5), 629–656. https://doi.org/10.1080/02687038.2014.1000819
- Irish Heart Foundation: Council for Stroke. (2010). National Clinical Guidelines and Recommendations for the Care of People with Stroke and Transient Ischemic Attack ( revised version). http://irishheart.ie/wp-content/uploads/2017/04/guidelines.pdf
- Jensen, L. R., Løvholt, A. P., Sørensen, I. R., Blüdnikow, A. M., Iversen, H. K., Hougaard, A., Mathiesen, L. L., & Forchhammer, H. B. (2015). Implementation of supported conversation for communication between nursing staff and in-hospital patients with aphasia. Aphasiology, 29(1), 57–80. https://doi.org/10.1080/02687038.2014.955708
- Kang, E., Kim, M. Y., Lipsey, K. L., & Foster, E. R. (2021). Person-centered goal setting: a systematic review of intervention components and level of active engagement in rehabilitation goal-setting interventions. Archives of Physical Medicine and Rehabilitation, 103(1), 121–130.e3. https://doi.org/10.1016/j.apmr.2021.06.025
- Leach, E., Cornwell, P., Fleming, J., & Haines, T. (2010). Patient centered goal-setting in a subacute rehabilitation setting. Disability and Rehabilitation, 32(2), 159–172. https://doi.org/10.3109/09638280903036605
- Levack, W. M. M., Sigert, R. J., Dean, S. G., & McPherson, K. M. (2009). Goal planning for adults with acquired brain injury: how clinicians talk about involving family. Brain Injury, 23(3), 192–202. https://doi.org/10.1080/02699050802695582
- Levack, W. M. M., Taylor, K., Siegert, R., Dean, S., McPherson, K., & Weatherall, M. (2006). Is goal planning in rehabilitation effective? A systematic review. Clinical Rehabilitation, 20(9), 739–755. https://doi.org/10.1177/0269215506070791
- Mats Ltd, T. (2021). Talking Mats. www.talkingmats.com
- Murphy, J., & Boa, S. (2012). Using the WHO-ICF with talking mats to enable adults with long-term communication difficulties to participate in goal setting. Augmentative and Alternative Communication, 28(1), 52–60. https://doi.org/10.3109/07434618.2011.653828
- Murphy, J., Tester, S., Hubbard, G., Downs, M., & MacDonald, C. (2005). Enabling frail older people with a communication difficulty to express their views: The use of talking mats as an interview tool. Health & Social Care in the Community, 13(2), 95–107. https://doi.org/10.1111/j.1365-2524.2005.00528.x
- National Institute for Health and Care Excellence. (2013). Stroke rehabilitation: Long term rehabilitation after stroke (Clinical Guideline 162). https://www.nice.org.uk/guidance/cg162/evidence/full-guideline-pdf-190076509
- NHS England. (2015). Stroke Services: Configuration Decision Support Guide. https://www.england.nhs.uk/mids-east/wp-content/uploads/sites/7/2018/03/stroke-services-configuration-decision-support-guide.pdf
- Parsons, J. G. M., Plant, S. E., Slark, J., & Tyson, S. F. (2018). How active are patients in setting goals during rehabilitation after stroke? A qualitative study of clinician perceptions. Disability and Rehabilitation, 40(3), 309–316. https://doi.org/10.1080/09638288.2016.1253115
- Plant, S., & Tyson, S. F. (2018). A multicentre study of how goal-setting is practised during inpatient stroke rehabilitation. Clinical Rehabilitation, 32(2), 263–272. https://doi.org/10.1177/0269215517719485
- Plant, S., Tyson, S., Kirk, S., & Parsons, J. (2016). What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clinical Rehabilitation, 30(9), 921–930. https://doi.org/10.1177/0269215516655856
- Playford, E. D., Siegert, R., Levack, W. M. M., & Freeman, J. (2009). Areas of consensus and controversy about goal setting in rehabilitation: A conference report. Clinical Rehabilitation, 23(4), 334–344. https://doi.org/10.1177/0269215509103506
- Rosewilliam, S., Roskell, C., & Pandyan, A. (2011). A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clinical Rehabilitation, 25(6), 501–514. https://doi.org/10.1177/0269215510394467
- Royal College of Physicians. (2016). National clinical guideline for stroke, Royal College of Physicians.
- Scobbie, L., Brady, M. C., Duncan, E. A., & Wyke, S. (2020). Goal attainment, adjustment and disengagement in the first year after stroke: A qualitative study. Neuropsychological Rehabilitation 31(5) ,1–19. https://doi.org/10.1080/09602011.2020.1724803
- Scobbie, L., Duncan, E. A., Brady, M. C., & Wyke, S. (2015). Goal setting practice in services delivering community-based stroke rehabilitation: A United Kingdom (UK) wide survey. Disability and Rehabilitation, 37(14), 1291–1298. https://doi.org/10.3109/09638288.2014.961652
- Scobbie, L., McLean, D., Dixon, D., Duncan, E., & Wyke, S. (2013). Implementing a framework for goal setting in community based stroke rehabilitation: A process evaluation. BMC Health Services Research, 13(190), 1–13. https://doi.org/10.1186/1472-6963-13-190
- Shrubsole, K., Worrall, L., Power, E., & O’Connor, D. A. (2019). Barriers and facilitators to meeting aphasia guideline recommendations: What factors influence speech pathologists’ practice? Disability and Rehabilitation, 41(13), 1596–1607. https://doi.org/10.1080/09638288.2018.1432706
- Simmons-Mackie, N. N., Kagan, A., Christie, O., Huijbregts, C., McEwenS, M., & Willems, J. (2007). Communicative access and decision making for people with aphasia: Implementing sustainable healthcare systems change. Aphasiology, 21(1), 39–66. https://doi.org/10.1080/02687030600798287
- Stroke Foundation. (2017). Clinical Guidelines for Stroke Management. https://files.magicapp.org/guideline/a0e5b148-3f2b-46c5-a68e-ab8e678e6f1b/published_guideline_3973-5_4.pdf
- Sugavanam, T., Mead, G., Bulley, C., Donaghy, M., Wijck, V., & F. (2013). The effects and experiences of goal setting in stroke rehabilitation a systematic review. Disability and Rehabilitation, 35(3), 177–190. https://doi.org/10.3109/09638288.2012.690501
- Turk, T., Elhady, M. T., Rashed, S., Abdelkhalek, M., Nasef, S. A., Khallaf, A. M., Mohammed, A. T., Attia, A. W., Adhikari, P., Amin, M. A., Hirayama, K., & Huy, N. T. (2018). Quality of reporting web-based and non-web-based survey studies: What authors, reviewers and consumers should consider. PLOS ONE, 13(6), e0194239. https://doi.org/10.1371/journal.pone.0194239
- van Rijssen, M. N., Veldkamp, M., Bryon, E., Remijn, L., Visser-Meily, J. M. A., Gerrits, E., & van Ewijk, L. (2021). How do healthcare professionals experience communication with people with aphasia and what content should communication partner training entail? Disability and Rehabilitation, 1–8. https://doi.org/10.1080/09638288.2021.1878561
- World Health Organisation. (2011). World report on disability. The Lancet, 377(9782), p. 1977. doi:10.1016/S0140-6736(11)60844-1