ABSTRACT
Background
There is increasing evidence that face-to-face treatments for verb and sentence production deficits in aphasia can be effective. However, very few studies have investigated supplementing such treatments with self-managed computer-based home practice. Given the increasing importance of computer-based aphasia treatment, it is imperative that the feasibility of this mode of delivering verb and sentence treatments is explored.
Aims
This study explored the feasibility and preliminary effectiveness of a novel computer-based treatment for sentence production deficits in aphasia, delivered by a combination of face-to-face and self-managed treatment sessions. The effect of treatment on verb and sentence production, discourse and functional communication was assessed.
Methods & Procedures
The study used a pre-post design with six single cases: three males and three females aged 49 – 81 years. The Sentence Production Treatment (SPT) was developed based on the evidence from systematic reviews of verb-in-isolation and sentence treatments respectively. The SPT was low dose (8 hours) and clinician delivered, supplemented by a minimum set level (16 hours) of self-managed computer-based treatment. The feasibility of the SPT was investigated by: monitoring recruitment and retention of participants; logging any technical issues; assessing the fidelity of face-to-face treatment delivery using checklists; and monitoring compliance with self-delivered treatment.
Outcomes & Results
The SPT was found to be feasible and acceptable to the six participants. Treatment effects were noted on trained verb production and sentence production for five participants each. Generalisation to untrained verb and sentence targets and discourse was more limited, however four participants perceived functional communication improvements.
Conclusions
The study represents the first preliminary evidence that a computer-based sentence level treatment for sentence production deficits in aphasia, which included a self-managed component, is feasible and can be effective. Given these overall positive findings of feasibility and benefit, further feasibility testing is warranted, exploring intervention refinement and candidacy.
Introduction
Computer-based treatments and home-practice have become an increasingly important resource for people with aphasia (PwA) (e.g., Floel, Citation2019; Kurland et al., Citation2018; Palmer et al., Citation2019). This has been driven by several forces. These include the need to supplement the limited face-to-face treatment available to PwA. For example, Palmer et al. (Citation2018) found that the median amount of treatment received by PwA in the UK, in the first 3 months post-stroke, was just 6.3 hours (2014 - 2016). This is in the context of growing evidence that a larger dose of aphasia treatment is required for it to be effective: a Cochrane review of 57 randomised controlled trials (RCTs) of aphasia treatment found that functional communication improved significantly for PwA who received treatment at high intensity, high dose, or over a long period of time, compared with those who received lower intensity or dose (Brady et al., Citation2016). NICE guidelines also state that rehabilitation treatments, including those for communication difficulty, should be administered for at least 45 mins per day for at least 5 days per week (https://www.nice.org.uk/guidance/qs2/chapter/Quality-statement-2-Intensity-of-stroke-rehabilitation). The requirement for larger/more intense doses of aphasia treatment likely has a neurophysiological basis. That is, the neuroplastic changes which underlie (re)learning following brain damage are likely to require intense (massed) practice (e.g., Dignam et al., Citation2016; Kleim & Jones, Citation2008; Raymer et al., Citation2008) and computer-based, self-managed aphasia treatment has been demonstrated to increase the dose of treatment received (e.g., Des Roches et al., Citation2015; Godlove et al., Citation2019). Greater use of computer-based treatments has also been driven by an awareness of the potential for technology to enhance the treatment of aphasia. Examples include the use of virtual realities to improve the functionality of treatment by simulating real-life communication (e.g., the virtual world of Eva Park investigated by Carragher et al., Citation2021 and Marshall et al., Citation2016). Finally, the COVID pandemic has been influential because it has enforced the remote delivery of non-urgent treatments such as aphasia therapy. This has led to an increased need for patients to self-manage their treatment, and Braley et al. (Citation2021) recently demonstrated that it is feasible to deliver self-managed, computer-based aphasia treatment (Constant Therapy) entirely remotelyFootnote1 Several studies have also demonstrated that PwA find computer-based treatments an acceptable alternative to face-to-face treatment (e.g., Kearns et al., Citation2019; Palmer et al., Citation2013) but that supervision by a speech and language therapist (SLT) is important (although, as noted by Braley et al. (ibid) this support can be remote). Indeed, Harrison et al. (Citation2020) found that support from an SLT increased compliance with self-delivered treatment.
Although the use of self-managed, computer-based aphasia treatments has proliferated in recent decades (e.g., the Constant Therapy website reports that 150 million exercises have been completed, with 400,000 downloads and 37,000 clinician users (https://constanttherapyhealth.com/constant-therapy/), the evidence base for their effectiveness is limited. For instance, there are currently only two full-scale RCTs of such treatments (Braley et al., Citation2021; Palmer et al., Citation2019), though both found treatment to be effective in improving trained items. Four systematic reviews of computer-based aphasia treatment have been conductedFootnote2 (Allen et al., Citation2012; Lavoie et al., Citation2017; Repetto et al., Citation2021; Zheng et al., Citation2016). These reviews included a total of 37 studies published between 1987 and 2019, with 197 participants. All four reviews concluded that computer-based aphasia treatments were effective in improving trained items, but limitations were noted in terms of: the low level of evidence; limited generalisation of treatment to untrained items and to functional communication; and the concentration on treating single words (usually nouns). This led to a number of recommendations including: that personally relevant (PR) items be treated; that attention be paid to the assessment and treatment of functional communication; and that computer-based treatments should also target verbs.
Regarding verb and sentence treatments, Hickin et al. (Citation2020, Citation2022) carried out two systematic reviews of such treatments (of 37 and 33 studies respectively). They found both types of treatment were highly effective in improving trained items (for 80-83% of participants), and, whilst generalization of verb treatments to untrained verbs was minimal (15% participants), it was better for sentence treatments (untrained sentences improved for 59% participants). Additionally, sentence treatments yielded gains in discourse (70% participants), and whilst functional communication was only assessed in some studies (in 24%: Hickin et al., Citation2022), it improved for 89% of participants. Disappointingly, only 5/37 studies of verb treatments and 1/33 sentence treatment studies were computer-based. Given the effectiveness of verb and sentence treatments, their delivery by computer warrants more attention.
The lack of computer-based verb and sentence treatments likely stems from the perception that verbs are harder to treat than nouns because, for example, they are more abstract than nouns, and because verb and sentence treatments are complex (Hickin et al., ibid). This may have fostered the belief that verb and sentence treatments would not lend themselves to delivery by computer, that PwA would find it hard to self-deliver such treatments using a computer, and/or they would find such treatments unacceptable. Exploration of whether this is indeed the case is imperative, particularly given the context of increasing reliance of PwA on computer-based aphasia treatments, that this mode of treatment has the capacity to increase dosage, and that the pandemic has increased the need for self-managed treatment. This paper reports on the feasibility and preliminary effectiveness of a novelFootnote3 sentence production treatment (SPT) which was computer-based and delivered using a combination of clinician-led and self-managed sessions, charting its impact on verb and sentence production, and on discourse and functional communication.
Method
Ethics
Ethical approval for this study was granted by the Ethics Committee of the School of Health Sciences, City, University of London (14/12/2017).
Recruitment
A recruitment call was put out via community groups, professional networks and The City Aphasia Research Register held by the Division of Language and Communication Science (LCS). The register contains details of PwA who have completed previous research projects within LCS and given their consent to be contacted about future research. PwA who expressed interest in the study were initially screened against eligibility criteria over the phone/by email (e.g., whether they had access to a device to host the SPT) and were subsequently screened face-to-face. They were provided with information about the study via an aphasia-friendly PowerPoint presentation using guidelines from the National Institute for Health Research Clinical Research Network: Stroke (Citation2014). Before the study commenced, written informed consent was obtained for all participants.
Participants
Five of the six participants in the study were recruited via the City Aphasia Lab Research Register, with the remaining participant referred by her sister. The details of the type and severity of participants’ aphasia are given in (pseudonyms have been used). demonstrates that three participants had moderate nonfluent aphasia (Ian, Jennie and Wendy), one severe nonfluent aphasia (Dave), one severe fluent aphasia (Andy) and one mild anomia (Peggy). Eligibility criteria included: over 18 years of age; aphasia following a single CVA; chronic post-stroke aphasia (i.e., at least 6 months post-onset); sufficient comprehension to access the SPT (i.e., a score of >25/30 on the Spoken Word Picture Matching subtest of the Comprehensive Aphasia Test (CAT: Swinburn et al., Citation2004) and >27/30 on the CAT Written Word Picture Matching subtest); a score of >75% on the CAT Word Repetition subtest; score of 20% - 80% on a subset of matched verbs and nouns (n = 43) from the OANB (Druks & Masterson, Citation2000). Previous experience using technology was not an exclusion criterion, but participants needed to own their own device to host the SPT. The presence of a motor speech disorder was also not an exclusion criteria (with the proviso that participants needed to score at least 75% on word repetition as noted above). Data collection ran from January 2018 to October 2019. Assessment data were collected face-to-face in the participants’ homes or at the university clinic. During the study, all participants continued to attend community stroke groups but were not engaged in clinician-directed intervention. Four significant others (SOs) initially consented to participate in the study (Jennie’s sister, Wendy’s partner, Andy’s wife and Peggy’s husband). However, only two were able to honour this commitment (Jennie’s sister and Wendy’s partner)Footnote4 They completed a CETI (Lomas et al., Citation1989) at four time points during the study and participated in an exit interview about their views of the SPT (its acceptability and perceived impact). SOs were not required to assist with the delivery of the SPT, although Andy’s wife assisted with the downloading of exercises and occasionally helped Andy with SPT exercises at his request.
Table 1. Participants’ demographic information.
Feasibility and Study Design
The research reported in this paper is a feasibility study of the SPT which was computer-based and delivered using a combination of clinician-led and self-managed exercises. A feasibility study was used because this is recommended for complex intervention interventions such as the SPT (e.g., by the MRC: https://webarchive.nationalarchives.gov.uk/ukgwa/20220207162925/http://mrc.ukri.org/documents/pdf/complex-interventions-guidance/). Complex interventions have - amongst other complexities - multiple interacting components, and feasibility studies are recommended to explore, for example, the practicality of delivering the complex treatment, its acceptability and for preliminary efficacy testing. A pre-post design (SCRIBE guidelines: Tate et al., Citation2016) was used to explore feasibility and preliminary effectiveness of the SPT with six participants. Single case designs are recommended to explore feasibility of complex interventions such as the SPT before investing in larger scale designs (e.g., Bowen et al., Citation2009). The outcome measures used to assess feasibility in this study are reported in rows 1 – 4, and those used for preliminary effectiveness testing are reported in - rows 5a – 5e. Measures were administered at baseline during two pre-treatment assessment sessions eight weeks apart (T1 and T2). This was followed by an intervention phase also of eight weeks during which no further testing was administered. Outcome measures were repeated immediately post-treatment (T3) and eight weeks later (T4) - see .
Table 2. Outcome measures.
The MRC recommends that new complex interventions are developed using the best available evidence (ibid). Therefore, to inform the development of the SPT, two systematic reviews were carried out. The first review related to verb in isolation treatments (Hickin et al., Citation2020), and the second to sentence level treatments (Hickin et al., Citation2022). Elements of treatments with the best evidence were incorporated into the SPT- see further discussion below. A third narrative review - of the evidence relating to the self-delivery of computer-based aphasia treatment - was carried out to inform how the largely face-to-face treatments evaluated in the systematic reviews should be adapted for the component of treatment which was self-delivered via computer (Hickin et al., in preparation).
Post-treatment (at T4), the acceptability of the SPT to participants was investigated using a questionnaire based on that used by Palmer et al. (Citation2013) – see Appendix 1. Brief post-treatment interviews based on the topic guide used by Palmer et al. (ibid) were also carried out with participants and the two participating SOs. Participants with aphasia were asked three open-ended questions: Have there been any benefits of computer treatment? Are there any disadvantages of computer treatment? What would influence your decision to do computer treatment? The interviews with SOs were guided using the following topics: Prior expectations of computer therapy; Ease/acceptability of using a computer; Benefits of computer therapy for the participant; Disadvantages of computer therapy for the participant; Limitations of computer therapy; Perceived change in talking; Changes in daily activity; Benefits of computer therapy for SO.
Intervention overview
Prior to the start of intervention (during pre-treatment baseline assessment), participants’ ability to use the SPT was screened and extra training (approximately 30 minutes) was given to those needing this (Ian and Peggy). Additionally, goals for treatment were set using a Goal Action Planning procedure (GAP e.g., Scobbie et al., Citation2011; Citation2013). These goals were used to help identify a set of personally relevant (PR) verbs for treatment (n=40) for each participant. People, Situations and Topics prompt cards from the Conversation Analysis Profile for People with Aphasia (Whitworth et al., Citation1997) were also used to assist the selection of PR verb, as were the results of the CETI and general conversation during the completion of background assessments at baseline. Picture prompts were not used with the aim of encouraging participants to select more abstract/less concrete words for treatment (Renvall et al., Citation2013a & b). gives the topics to which the PR verbs chosen by participants belonged. The final selection of PR verbs was determined by a process of discussion between the clinician (JH) and each participant. However, Wendy’s PR verbs were selected entirely independently by Wendy and her SO. PR verbs were divided into control and treatment sets (n=20) matched for baseline performance (using McNemar’s TestFootnote5) and psycholinguistic variablesFootnote6
Table 3. The topics to which the PR verbs chosen by participants belonged (based on the classification system used in Palmer et al., 2017).
Planned intervention comprised eight face-to-face sessions of approximately one hour delivered weekly by the first author (JH who is an experienced SLT), supplemented by a recommendation of at least two hours a week of self-delivered treatment (total planned treatment = 24 hours). Face-to-face sessions took place in participants’ homes or a university clinic and were used to: upload, introduce and practise the SPT exercises which were presented in PowerPoint slides; review progress; provide encouragement; discuss any difficulties experienced with exercises. Any potential barriers to self-delivering the SPT were also discussed using a GAP procedure, and solutions identified.
The content of the individual SPT exercises was based on systematic reviews of verb treatment studies (Hickin et al., Citation2020) and sentence treatment studies (Hickin et al., Citation2022) respectively. These reviews were carried out specifically to ensure that the SPT was evidence-based as recommended by the MRC for a complex treatment (see earlier discussion). Thus, for example, the SPT comprised three phases -1. Verb Treatment, 2. Sentence Treatment and 3. Generalisation. This was because, the systematic reviews demonstrated that sentence treatments often included elements of verb treatments, particularly in the early stages of treatment (e.g. semantic and written cue provision in Step 1 of Verb Network Strengthening treatment (VNeST) - see Edmonds, 2014; Edmonds et al. Citation2015), with some studies pointing to the need for verb exercises to raise metalinguistic awareness of verbs prior to sentence treatment (e.g., Carragher et al., Citation2015). Thus, Phase 1 of the SPT comprised verb exercises and Phase 2 sentence exercises. Phase 3 (generalisation) was included as the systematic reviews also indicated that specific exercises were needed to facilitate generalisation of improved skills to real life communication (e.g. Byng et al., Citation1994; Newton et al., Citation2017). A detailed analysis of verb and sentence treatment content carried out during the systematic reviews informed the individual exercises in each treatment phase. (This analysis is reported for verb tratments in , in Hickin et al. (Citation2020) and for sentence treatments in , in Hickin et al. (Citation2022)). Treatments with the best evidence (reported in in both Hickin et al., Citation2020 and Citation2022) were incorporated into the SPT. Thus, for example, semantic feature analysis was included in verb treatment exercises based on the evidence from a series of studies by Wambaugh and colleagues (e.g., Wambaugh & Ferguson, Citation2007; Wambaugh et al., Citation2014); whilst VNeST was included in sentence exercises based on the work of Edmonds and colleagues (e.g., Edmonds, 2014; Edmonds et al., Citation2015).
Photographs of PR verbs were used as stimuli in all three phases of treatment. Where possible, these photographs were personal to participants with the aim of increasing the salience of stimuli (e.g., Raymer et al., Citation2008). Alternatively, Google Images were used. In addition to photographs, phase 3 used picture sequences, video retell and script training to facilitate generalisation to narrative production (e.g., Carragher et al., Citation2014; Cherney et al., Citation2015). Cueing hierarchies mirrored those reported in the systematic reviews, and included progressive sound and written cues in verb exercises, (e.g., Conroy et al., Citation2009a, b & c) and a sentence hierarchy in declarative sentence exercises (SV -> SVO -> SVOP, e.g., Bazzini et al., 2011). Colour coding and wh- questions were also used in sentence exercises to increase understanding of the thematic roles played by arguments in sentences (e.g. Byng, et al., Citation1994). Imperatives, yes/no and Wh- questions were also targeted in the SPT (e.g., Helm-Estabrooks, 1986). Cues and cueing hierarchies were demonstrated by the clinician in face-to-face sessions, with the clinician also ensuring that each participant was able to use cues independently, with extra demonstrations if required. Instructions and feedback given by the clinician in face-to-face sessions was also informed by the systematic reviews (e.g., explaining the nature of participants’ errors – VNeST: Edmonds, 2014)Footnote7 Verbs produced in isolation were marked correct if they were produced within 5 seconds. Sentence structure produced within 10 seconds was scored. A detailed treatment manual (for face-to-face sessions) is available on request from the first author, whilst the evidence base for the SPT is summarised in Supplementary Table A and the SPT is reported according to the Template for Intervention Description and Replication (TIDieR) Checklist (Hoffman et al., Citation2014) in Appendix 2.
Missing Data
The following assessment data were not recorded because of equipment failure: the SCT for Ian at T2; the SCT and sentence production using PR verbs at T3 for Wendy. Data on the AMI at T3 for Ian could not be collected due to his hospitalisation; and the SCT for Dave at T3 due to participant fatigue. The AMI was not administered to Dave because he found it distressing due to the severity of his expressive impairment. In terms of the assessment data from SOs, Wendy’s partner completed all CETIs; Jennie’s sister forgot to complete the CETI at T2 but completed all others.
Results
The results for the feasibility of the SPT will be reported first followed by preliminary effectiveness testing.
Feasibility
Regarding the feasibility of recruiting suitable participants for the SPT, 12 PwA were screened, eight were suitable and six of these consented to participate. The reasons participants did not participate in the study are given in below.
Table 4. Reasons screened participants did not participate in the research project.
In terms of participant retention, all participants were retained for the duration of the study. However it should be noted that, to retain participants, the clinician (JH) was very flexible in accommodating participants’ needs (e.g., visiting them at home when travel to the clinic was difficult) and this will be addressed further in the Discussion. In terms of the technical feasibility of the SPT, it was used successfully on a variety of devices (see - column 1), and, with the exception of Peggy, participants were able to use the SPT independently (see further discussion below).
Table 5. Feasibility of the SPT (participants reported in order of amount of self-managed practice completed).
In terms of the fidelity of the SPT, the intended duration of treatment was eight weeks. In actuality, the SPT was delivered over 8 – 17 weeks (see , column 6). This was mostly due to participants’ personal circumstances (e.g., health issues for Jennie, Andy, Ian and Peggy, and a holiday for Wendy), whilst travel issues for the clinician extended Dave’s treatment. Regarding the number of face-to-face sessions delivered, the intention was eight sessions, and these were delivered to 5/6 participants (Andy received only 6 sessions because he went to stay with his terminally ill mother – see , column 5). The fidelity of the SPT delivered face-to-face was assessed using treatment fidelity checklists developed from a SPT manual written prior to the start of treatment. Checklists were completed by the clinician (JH) after each session, noting presence /absence of expected behaviours, and 25% of sessions were cross-checked by listening to the audiotape of the session with 100% agreement. The fidelity of treatment delivery ranged from 92% - 100% with an average fidelity of 98%.
The fidelity of the self-managed component of the SPT was monitored by participants completing a diary. Diary sheets were provided to participants at the end of each face-to-face session and participants recorded a) the exercises completed, b) the length of time spent on each exercise, and c) how often each exercise was completed. The amount of practice completed by each participant is reported in , columns 7, 8 and 9. There was a large range in the amount and intensity with which the SPT was self-delivered (column 7 and 9 respectively). The average amount of treatment delivered per week (column 8) varied from nearly 5 hours 23 minutes (Wendy) to 24 minutes (Peggy). The total amount of treatment delivered (column 7) also varied widely, with Wendy, Steve and Andy far exceeding the requested amount of 16 hours. Jennie met the requested amount, although it should be noted that she did not complete her aphasia diary on two occasions but reported she had practised. Therefore, the reported amount of treatment is a likely underestimate. Ian and Peggy did not self-deliver the requested amount of treatment. The likely underlying reasons for this are reported in , columns 2, 3 and 4. Thus, Peggy was the only participant who was not a frequent computer-user at the start of treatment (column 2) although Peggy rated herself as very experienced at using a computer because she had previously used computers frequently at work, i.e., until her retirement 20 years earlier. Despite receiving training during baseline sessions, Peggy was unable to consistently use the SPT slides independently and needed help to self-manage her exercises (column 3) but did not have access to a carer who could help (column 4). This was the same for Ian who also did not self-manage the requested amount of treatment. Peggy and Ian contrast with Andy who needed some help with the SPT exercises but had a carer who could assist (his wife) and as a result was able to self-deliver (more than) the requested amount of treatment. Finally, it should be noted that Wendy, Steve and Peggy continued to practise the SPT between T3 and T4 (Wendy for an unspecified amount of time, Peggy for an additional eight hours and Steve for 12 hours) and therefore this does not constitute a maintenance phase for them. This is considered in the reporting and discussion of preliminary effectiveness testing below.
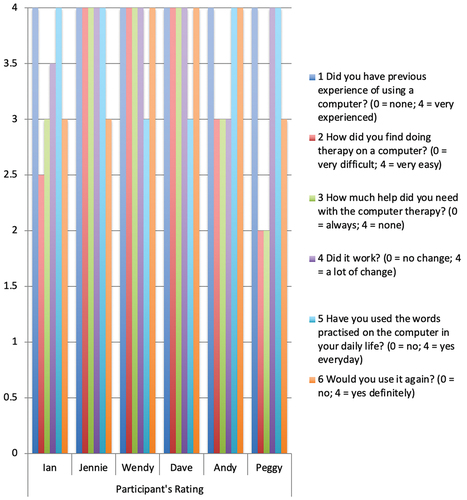
Regarding the acceptability of the SPT, participants’ responses to the questionnaire administered post treatment are reported in . All participants rated themselves as very experienced at using a computer (question 1). Wendy, Jennie and Dave found doing the therapy on the computer very easy (question 2) and needed no help (question 3); whereas Ian, Andy and Peggy found it less easy and needed a little or some help. All participants perceived change in their communication as a result of treatment (question 4), with four perceiving a lot of change (Wendy, Jennie, Dave, Peggy) and two some change (Ian, Andy), and all had used their words in daily communication either every day (Ian, Jennie, Andy, Peggy) or most days (Wendy, Dave) (question 5). Finally, three participants indicated that they would definitely use the SPT again (question 6), whilst three rated this as very likely (Ian, Jennie, Peggy).
Participants’ responses in the semi-structured interviews (which were kept brief to comply with the ethical approval for the study) indicated perceived improvements in confidence for three participants (Ian, Jennie and Dave). Jennie and Wendy also reported improvements in talking which were confirmed by their SOs (Jennie’s sister and Wendy’s partner) (question 1). Very few disadvantages were mentioned (Q2) by participants: technical issues were cited by Ian and Peggy, and Andy would have liked treatment to be even more intensive. Jennie and Wendy felt there were no disadvantages to computer-based treatment, and Dave was very eager to express his opinion that face-to-face visits were not necessarily needed to supplement computer delivered treatment. Ian and Andy commented that the impact of self-managed treatment on their confidence and sense of self-efficacy would influence their decision to do computer treatment (Q3). Dave indicated that improving his talking would be the main influence on his decision and that he did not see computer-based treatment as second best. Wendy responded that she would have liked some more difficult SPT exercises. Jennie indicated that time was an issue (i.e., having the time to practise) and that lack of face-to-face treatment meant that computer-based treatment was the only option for her (and by implication for many PwA). Peggy commented that she felt her age was an issue: she said she was “a bit old” to do computer-based treatment.
In terms of SOs’ views of the SPT, neither Jennie’s sister nor Wendy’s partner made any comments in relation to perceived disadvantages of the computer-based treatment. Indeed, Jennie’s sister commented on the realities of the availability of SLT services: she said if Jennie hadn’t done the computer-based treatment she wouldn’t get (and hadn’t got) any treatment in her area. Both SOs were positive about the impact of the SPT on talking and daily activity: for example, Wendy’s husband said that she had started to use words which were “unusual for her” and had started going to the gym, whilst Jennie’s sister commented on her being more fluent and talking in more structured sentences. She also felt that Jennie’s confidence had increased, specifically, that Jennie had started to answer the phone, and that she had rung her sister rather than texting as previously.
Preliminary Effectiveness Testing
The results of the preliminary effectiveness testing of the SPT are now reported, for the production of: i) trained and untrained verbs, ii) untrained nouns, iii) sentence production using trained and untrained verbs, iv) verb and sentence production in discourse and v) in functional communication as perceived by a) the participants with aphasia themselves and b) their SOs. summarises the impact of treatment at each of these levels of communication. A within-subject statistical analysis was carried out using a one-tailed McNemar’s Test for lexical retrieval of nouns and verbs, Chi Square for PAS in sentences and Friedman’s Test for CAT picture description and the CETI (significance level p. <0.05 in all cases). It should be noted that Wendy, Dave and Peggy continued to carry out SPT exercises between T3 and T4 so this is not a maintenance phase for them. This is taken into account in the ensuing discussion.
Table 6. Summary of the effect of the SPT on participants’ language and communication.
In summary, five of the six participants showed significant improvement in retrieval of verbs post-treatment, with a nonsignificant trend of improvement for the sixth participant (Dave). Improved verb retrieval was restricted to treated verbs for three participants: Ian and Wendy showed significant improvement in the production of untreated verbs (see Supplementary Table B) and for Wendy this appears to have been as a result of extra treatment she self-delivered between T3 and T4 . Five participants also showed significant improvements in lexical retrieval in sentences: Ian, Jennie, Wendy, Dave and Peggy. For Wendy and Peggy this again appears to have resulted from extra self-delivered treatment between T3 and T4. All five participants showed improved production of agents, three showed improved production of verbs, and two of objects (see Supplementary Table C). Predicate argument structure also improved for four participants. Jennie and Andy showed significant improvement in production of verbs with one argument, whilst for Ian and Wendy production of verbs with two arguments improved significantly, and again for Wendy this appears to have resulted from extra self-delivered treatment. Dave had been unable to produce a verb with an argument at all before treatment but showed a nonsignificant improvement in the production of verbs with one argument (agent) after treatment, with production of objects also emerging.The effect of the SPT on discourse was more limited, with three participants showing improvements (Jennie, Wendy and Andy). Four participants reported improvements in functional communication (Jennie, Wendy, Dave and Peggy), and these were corroborated by two SOs.
Discussion
The feasibility of the SPT will be discussed first, followed by the results of preliminary effectiveness testing.
In terms of the feasibility of recruiting suitable participants to the SPT, 12 participants were screened and of these, eight participants (66%) were suitable for the SPT, with six (75%) consenting to participate in the study and all these participants were successfully retained for the duration of the study. Bearing in mind the small number of participants, this suggests that it is feasible to recruit and retain participants to the SPT and that a future, larger scale study is achievable. Recruiting SOs to participate in a future study appears less feasible however, as only two of the four SOs who consented to participate did so successfully. In terms of retention, all six participants were retained for the duration of the study indicating that the self-delivery of the SPT was not too onerous for them. However, the researcher also implemented strategies to improve participant retention, namely visiting participants in their homes when they were unable to attend the clinic, accommodating their schedules in arranging treatment sessions (e.g., to allow Andy to visit his terminally ill mother) and keeping in regular communication with them. These strategies were amongst those found to be effective in improving retention by Spell et al. (Citation2020) in a treatment study involving 150 participants for a total of 42 weeks, and it is intended that similar strategies are implemented in any future study.
Regarding the technical feasibility of the SPT, the SPT worked on a variety of devices - namely tablets, laptops, desktops and a smart phone - and on Windows based and Apple devices. The capacity for computer-based aphasia treatment packages to work on multiple platforms is a high priority for SLTs as this is likely to maximise the amount of treatment self-delivered since PwA can practice on any device available to them (Swales et al., Citation2016). Another factor that could affect the technical feasibility of self-managed computer-based aphasia treatment was the ability of participants to use the SPT independently: five of the six participants (83%) achieved independent use of the SPT. This is similar to the percentage reported in other studies of self-delivered, computer-based treatments (e.g., Kurland et al. Citation2018; De Cock et al., Citation2021). The level of independent use likely reflects the aphasia-friendly design of the human-computer-interface (HCI) of the SPT which was informed by the small but developing field of research into aphasia-friendly HCIs (e.g., Brandenburg et al., Citation2013).
In terms of the acceptability of the computer based SPT, the six participants and the two SOs who completed exit interviews were very positive, with very few disadvantages identified. This is in line with the findings of Kearns et al. (Citation2019) who reviewed 27 studies that included self-report of the acceptability of computer-based aphasia treatment. The acceptability of the SPT likely reflects the following four key features of the SPT. First, its aphasia-friendly design which meant it was largely very accessible and hence presumably acceptable. Second, the targeting of PR verbs in the program which aimed to increase the saliency of the stimuli perhaps helped participants to stay interested and motivated. This would be in line with the findings of the Big CACTUS study where both participants with aphasia and SLTs implementing the treatment regarded personalisation of treatment as important to motivation (Harrison et al., 2021, Burke et al., Citation2021 respectively). Third, the SPT was related to participants’ goals: Kearns et al. (Citation2019) found this to be very important to the acceptability of computer-based treatment. Finally, the SPT included weekly contact with the clinician. Harrison et al. (2021) found both participants with aphasia and carers regarded support from an SLT/SLTA as an important factor in making self-managed computer-based treatment acceptable. Finally, the acceptability of the SPT is indicated by its continued use during the maintenance phase by three participants. Although this continued practice weakened the strength of the preliminary effectiveness findings, it was a deliberate decision to leave the SPT with participants to see if there was any continued use - in other words to determine the demand for the treatment which is an aim of feasibility studies (Bowen et al., Citation2009). The decision was informative in this regard. It also indicated that these participants perceived the SPT to be beneficial and demonstrated that Peggy - who was unable to self-manage the SPT independently during the treatment phase - was able to learn how to do this given extra time.
Regarding compliance with the SPT, four of the six participants (Jennie, Wendy, Dave and Andy) were compliant with the total amount of self-managed treatment requested (16 hours), and three participants delivered it to the requested intensity of at least two hours a week (Wendy, Dave and Andy), with Jennie also likely to have done so (she recorded an average of 1 hour 45 minutes treatment a week but reported that she had practised more than this). This yields a compliance rate of 66% for the SPT which is similar to that reported in Palmer et al. (2012) (66.7%) but lower than that in Kurland et al. (Citation2018) (83%). There was also very wide variation in the amount and intensity of treatment self-managed (planned:16 hours over 8 weeks): from <7 hours over 17 weeks (Peggy), to >59 hours over 11 weeks (Wendy). Ian also self-delivered a small amount of treatment: 11 hours over 11 weeks. The factors which appeared to interact to reduce Ian and Peggy’s compliance were in line with those identified by Harrison et al. (2021). First, Ian and Peggy had more limited competence with technology than the other four participants, with Peggy in particular standing out as the only participant who was not a frequent user of technology when she started treatment. This meant that both Ian and Peggy were not immediately independent in self-managing treatment (though Ian rapidly became so), whilst Peggy only learnt to use the SPT independently after the end of the treatment phase (when she practised between T3 and T4). Also of likely significance is that whilst Ian, Andy and Peggy all needed help to use the SPT, only Andy had access to someone who could help (his wife). When Ian and Peggy ran into difficulty with the SPT there was no one to assist them to overcome this (although the clinician attempted to help via the phone). Finally, of likely relevance is the health of Ian and Peggy: both were hospitalised during the treatment phase (twice in the case of Peggy) and this also reduced their ability to comply with treatment. In summary, the failure of Ian and Peggy to comply with the amount of treatment requested reflected the interaction of three factors namely - poorer competence with technology, lack of support to solve technical issues, and poor health.
In terms of the fidelity of the component of the SPT that was delivered face-to-face, this was assessed using checklists developed from a treatment manual written for the SPT. Face-to-face treatment was delivered to an average of 98% adherence to the treatment protocol (range 92-100%). This is similar to the levels of adherence to the VNeST treatment protocol reported by Edmonds and colleagues (e.g., Edmonds et al., Citation2014) who reported 98%-99% adherence. However, an important caveat is that fidelity was monitored by the clinician delivering treatment (JH) rather than an independent assessor – see Limitations below. The fidelity of the self-managed component of the SPT was assessed manually using an exercise diary, and only the time spent on exercises was recorded. In future studies it is intended that this will be monitored automatically by the platform used to deliver the SPT as recommended by Kurland et al. (Citation2018) and similar to, for example, Constant Therapy. This will allow success levels, rate of progress and use of cues in the SPT to be monitored (see e.g., Des Roches et al., Citation2017).
Regarding preliminary effectiveness testing, the results must be interpreted in the context of the lack of blinding of the assessor (who was the clinician delivering the treatment and assessments). Additionally, there was no inter-rater reliability for exploring broader fidelity aspects (i.e., with a blinded second rater) due to lack of funding to employ blind raters. Both of these factors undermine the validity of the effectiveness results (see further discussion in the Limitations section below). Bearing this important caveat in mind, the SPT resulted in significant improvement in personally relevant verb production for five of the six participants with the sixth participant (Dave) showing a non-significant trend of improvement. The effectiveness of the SPT in terms of verb production is similar to that found for face-to-face verb treatments (Hickin et al., Citation2020: 80%). Improvement in verb production was restricted to treated verbs for three participants, however Ian and Wendy also showed significant improvement in untreated verbs. This is worthy of further investigation since generalisation of self-delivered computer-based verb treatment has only been reported for one of the 27 participants included in previous reporting of such treatments (in Routhier et al., 2016). Sentence production using PR verbs also improved significantly for five of the six participants (83%), with Andy showing a non-significant trend of improvement. The improvement in sentence production reflected better lexical retrieval in sentences using both treated verbs (for Ian, Jennie, Wendy and Dave), and untreated verbs (Ian, Jennie, Dave and Peggy). Improvements in the production of sentence structure (PAS) were also found (for Ian, Jennie and Wendy), but these were largely restricted to treated verbs. This finding again suggests that verb and sentence treatments, despite their complexity, can be successfully delivered face-to-face using a computer and subsequently self-managed and that this field is worthy of more attention in the research literature (Hickin et al., Citation2020, Citation2022).
The impact of the SPT on discourse production was limited, with only one participant showing a statistically significant improvement (Jennie) and two showing a trend of improvement (Wendy and Andy). The reasons for the more limited impact of the SPT on discourse are unclear but may relate to the self-delivery of treatment via computer giving fewer opportunities to practise discourse. The Generalisation Phase of the SPT was specifically designed to address this potential weakness but on average participants spent least time in this phase of treatment. This will have diluted the dose of treatment given to discourse production and rendered it less effective. It might also indicate that participants found generalisation exercises harder to do independently which should be explored in future iterations of the SPT. The means used to gather a sample of discourse (the AMI) may also have been influential in that it likely produced a fatigue effect for five of the six participants. Thus, a future study of the SPT could use a different measure of discourse (e.g., The Scenario Test (van de Meulen et al., 2010)). In summary, it is not possible to reach any firm conclusions regarding the reasons for the more limited impact of the SPT on discourse and this would be a focus of future research.
Finally, the impact of the SPT on functional communication as assessed by the CETI was promising, with significant improvement perceived for four of the six participants. The perceived improvement in functional communication was backed up by improvements in language measures for all four participants (although for Peggy the perceived improvement likely reflected increased confidence when communicating, as improvements in her language per se were limited). The study thus provides preliminary evidence that sentence treatment delivered and self-managed by computer can have an impact on functional communication. This has only been formally investigated in one other study of self-delivered computer-based treatment. Palmer et al. (Citation2019) found no impact of StepByStep treatment on functional communication and highlight that developing self-delivered computer-treatments which have a functional impact should be an important priority of future research. The findings of this study represent a possible way forward here in that the personally relevant nature of the trained verbs may have been key to producing a functional impact. However, Palmer et al. also targeted personally relevant words which were in this case mostly nouns. It is therefore possible that the targeting of personally relevant verbs was key. Indeed, it has been proposed before that targeting verbs may induce greater improvement in real life communication because of their key role in sentence production (e.g., Conroy et al., Citation2006; Lavoie et al., Citation2017)). Finally, it must be noted again that three participants continued to use the SPT during the maintenance phase, and therefore no clear conclusions can be reached about the maintenance of treatment effects from the SPT.
In terms of candidacy for the SPT, all findings are tentative given the small number of participants (n = 6). There are, however, indications that the SPT is most suitable for participants with non-fluent aphasia, with relatively intact lexical retrieval and syntactic processing (Ian, Jennie and Wendy) – a finding in line with the research investigating VNeST (e.g., Edmonds et al., Citation2015). Dave, who was also non-fluent, had a more limited response to treatment and this likely reflected his more severe expressive impairment. It is possible he would have shown more improvement if given a larger amount of treatment. The two participants who responded least well to the SPT had fluent aphasia (Andy and Peggy) and fluent aphasia may therefore not represent good candidacy for the SPT. However, this requires further investigation as it is possible that floor effects were responsible for Andy’s limited response to the SPT (he was the most severely impaired of all the participants), whilst ceiling effects may have been present for Peggy who had the mildest impairment. Peggy also self-delivered the least amount of treatment over a prolonged period, reducing her dose. Finally, both Andy and Peggy did show some changes (e.g., Andy showed evidence of improved event processing in his attempts at sentence production post-treatment). Verb and sentence treatments have not been routinely trialled with people with fluent aphasia and this should be addressed (Hickin et al., Citation2020, Citation2022). Finally, it is of note that the impact of the SPT on verb and sentence production using personally irrelevant verbs was minimal. This indicates that personal relevance (i.e., salience) may make words more responsive to aphasia treatments (e.g. Raymer et al., Citation2008). However, much larger scale research is required to confirm this preliminary indicative finding. Finally, that three participants (Wendy, Peggy and Dave) continued to self-deliver the SPT between T3 and T4 undermined findings regarding the maintenance of treatment effects for the SPT. It did however indicate that these participants found the SPT acceptable and perceived it to be beneficial.
Limitations
The study used a pre-post treatment design with only six participants and as such represents a low level of evidence (e.g., Tate et al., Citation2016). Future studies will consider stronger designs such as a withdrawal design or a case series. Future studies would also implement a true maintenance phase for all participants by withdrawing the SPT at the end of the treatment phase. This study lacked blind and inter-rater assessment of effectiveness and future studies will include funding for this. Data were missing at some time points for 4/6 participants and steps will be taken to address this (e.g., by recording assessment data on two devices). The fidelity of the face-to-face component of the SPT was assessed by the clinician herself (JH) and in future studies this will be assessed by a researcher independent of the study. The fidelity of the self-delivered component of treatment was assessed manually by participants which made it subject to error, and in future studies this would be monitored automatically by the platform used to deliver treatment. The SPT was also not delivered to the intended amount or intensity for some participants. Future iterations of the SPT will consider remote delivery of the face-to-face component of treatment to minimise barriers to compliance such as travel difficulties (e.g., Braley et al., Citation2021), whilst automatic monitoring of compliance would facilitate early identification of poor compliance, allowing this to be addressed immediately hopefully improving control of the delivery of the treatment protocol.
Conclusion
The limited amount of face-to-face treatment available to PwA has led to a research-practice gap with doses of aphasia treatment given unlikely to be effective (Cavanaugh et al., Citation2021). Recent research also indicates that the amount of treatment received may be the most important predictor of response to treatment alongside the size and location of lesion (Hope et al., Citation2021). Finding ways to supplement aphasia treatment is therefore of paramount importance, with self-managed computer-based treatment a feasible means of doing this. However, computer-based treatments have limited evidence of functional impact. This may be due to the concentration on treating single words (nouns) which has overlooked the potential for verb and sentence treatments to generalise to real-life communication more readily. This feasibility study with preliminary effectiveness testing therefore investigated a novel computer-based treatment for sentence production deficits in aphasia, delivered by a combination of clinician-led and self-managed treatment sessions. The study found that the SPT was feasible and efficacious in improving trained verb and sentence production, with initial indications being that individuals with nonfluent aphasia benefitted most from treatment. The impact of treatment on untrained verb and sentence production and on discourse was more limited. However, four of the six participants perceived their functional communication to have improved, and the targeting of verbs which were personally relevant in treatment may have been important in producing functional impact, as well as contributing to compliance with and acceptability of the self-managed computer-based treatment.
APH-PA_22-046-File012.docx
Download MS Word (19.9 KB)APH-PA_22-046-File011.docx
Download MS Word (14.5 KB)APH-PA_22-046-File010.docx
Download MS Word (19.1 KB)APH-PA_22-046-File009.docx
Download MS Word (37.7 KB)APH-PA_22-046-File008.docx
Download MS Word (13.6 KB)Disclosure Statement
No potential conflict of interest was reported by the authors.
Supplementary information
Supplemental data for this article can be accessed online at https://doi.org/10.1080/02687038.2022.2116928
Notes
1. It should be noted that computer-based aphasia treatments can be either self-managed by PwA – usually with supervision from a speech and language therapist, or clinician delivered – i.e., the PwA only uses the computer-based exercises during face-to-face sessions. The treatment explored in this study, contains elements of both i.e. face-to-face sessions introduced computer-based exercises which were then self-delivered between face-to-face sessions.
2. Both self-managed and clinician delivered computer-based treatments were reviewed.
3. The treatment is novel in that it was developed from two systematic reviews of the literature relating to i) verb in isolation treatments (Hickin et al., Citation2020) and ii) sentence level treatments (HIckin et al., Citation2022). Thus, the SPT combined elements of treatments identified to have the best evidence base (e.g., sound and letter cues in verb treatment exercises and elements of mapping treatments in sentence exercises) and this has not been done before. Treatments included in the SPT were also adapted for self-delivery via computer this time informed by a narrative review of the evidence relating to the self-delivery of computer-based aphasia treatment (Hickin, in preparation) and this is also novel for sentence level treatments – see also discussion below.
4. Ian and Dave lived alone and did not identify a SO to participate in the study. Peggy’s husband consented to participate but his initial completion of the CETI caused some friction between them and the clinician did not therefore ask him to complete any further assessments. Andy’s wife also consented to participate but she was unable to honour this commitment due to personal cicumstances.
5. There were no significant differences between treated and untreated sets for any participant.
6. Concreteness, familiarity, frequency, imageability, number of syllables using the MRC psycholinguistic database (https://websites.psychology.uwa.edu.au/school/MRCDatabase/uwa_mrc.htm).
7. As the Powerpoint slides were a prototype they were not programmed to give feedback to participants during self-delivered exercises. It is intended that future versions of the SPT will have this capacity.
References.
- Allen, L., Mehta, S., McClure, J.A. & Teasell, R. (2012). Therapeutic Interventions for Aphasia Initiated More than Six Months Post Stroke: A Review of the Evidence. Topics in Stroke Rehabilitation, 19, 523–535. https://doi.org/10.1310/tsr1906-523.
- Bastiaanse, R., Edwards, S. & Rispens, J. (2002). The Verb and Sentence Test. Bury St Edmunds: Thames Valley Test Company Limited.
- Bazzini, A., Zonca, G., Craca, A., Cafforio, E., Cellamare, F., Guarnaschelli, G., Felicetti, G. & Luzzatti, C. (2012). Rehabilitation of argument structure deficits in aphasia. Aphasiology, 26, 1440–1460, doi:10.1080/02687038.2012.690023
- Bowen, D.J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L et al. (2009). How We Design Feasibility Studies. Am J Prev Med, 36, 452–457. doi:10.1016/j.amepre.2009.02.002.
- Brady, M.C., Kelly, H., Godwin, J., Enderby, P. and Campbell, P. (2016). ‘Speech and language therapy for aphasia following stroke’, Cochrane Database of Systematic Reviews, 6 (Art. No.: CD000425).doi: 10.1002/14651858.CD000425.pub4.
- Braley, M., Sims Pierce, J., Saxena, S., De Oliveira, E., Taraboanta, L., Anantha, V., Lakhan, S.E. and Kiran, S. (2021). A Virtual, Randomized, Control Trial of a Digital Therapeutic for Speech, Language, and Cognitive Intervention in Post-stroke Persons with Aphasia. Frontiers in Neurology, 12, Article 626780.
- Brandenburg, C., Worrall, L., Rodriguez, A. D. & Copland, D. (2013). Mobile computing technology and aphasia: An integrated review of accessibility and potential uses. Aphasiology, 27, 444–461.
- Burke, J., Palmer, R., & Harrison, M. (2021). What are the factors that may influence the implementation of self-managed computer therapy for people with long term aphasia following stroke? A qualitative study of speech and language therapists’ experiences in the big CACTUS trial. Disability and Rehabilitation, doi:10.1080/09638288.2020.1871519
- Byng, S., Nickels, L. & Black, M. (1994). Replicating therapy for mapping deficits in agrammatism: Remapping the deficit?, Aphasiology, 8, 315–341, doi: 10.1080/02687039408248663
- Carragher, M., Steel, G., Talbot, Devane, N., Rose, M.L. & Marshall, J. (2021). Adapting therapy for a new world: storytelling therapy in EVA Park, Aphasiology, 35:5, 704–729. doi: 10.1080/02687038.2020.1812249
- Carragher, M., Sage, K. and Conroy, P. (2015). Outcomes of treatment targeting syntax production in people with Broca’s-type aphasia: evidence from psycholinguistic assessment tasks and everyday conversation. International Journal of Language & Communication Disorders, 50, 322–336.
- Carragher, M., Sage, K. & Conroy, P. (2014). Preliminary analysis from a novel treatment targeting the exchange of new information within storytelling for people with nonfluent aphasia and their partners, Aphasiology, doi: 10.1080/02687038.2014.988110
- Cavanaugh, R., Kravetz, C., Jarold, L., Quique, Y., Turner, R. & Evans, W.S. (2021). Is There a Research–Practice Dosage Gap in Aphasia Rehabilitation? American Journal of Speech-Language Pathology, 30, 2115–2129.
- Cherney, L. R., Kaye, R. C., Lee, J. B., & van Vuuren, S. (2015). Impact of personal relevance on acquisition and generalization of script training for aphasia: A preliminary analysis. American Journal of Speech-Language Pathology, 24, S913–S922. doi:10.1044/2015_AJSLP-14-0162
- Conroy, P., Sage, K., & Lambon-Ralph, M. (2009a). A comparison of word versus sentence cues as therapy for verb naming in aphasia. Aphasiology, 23, 462–482 .
- Conroy, P., Sage, K., & Lambon-Ralph, M. (2009b). The effects of decreasing and increasing cue therapy on improving naming speed and accuracy for verbs and nouns in aphasia, Aphasiology, 23, 707–730.
- Conroy, P., Sage, K. & Ralph, M.A.L. (2009c). Errorless and errorful therapy for verb and noun naming in aphasia. Aphasiology, 23, 1311–1337.
- Conroy, P., Sage, K. & Ralph, M.A.L. (2006). Towards theory‐driven therapies for aphasic verb impairments: A review of current theory and practice. Aphasiology, 20, 1159–1185, DOI: 10.1080/02687030600792009
- Constant Therapy (undated) Available at: https://constanttherapyhealth.com/constant-therapy/ [Accessed 25th March 2022].
- De Cock, E., Batens, K., Feiken, J., Hemelsoet, D., Oostra, K., & De Herdt, V. (2021). The feasibility, usability and acceptability of a tablet-based aphasia therapy in the acute phase following stroke. Journal of Communication Disorders, 89. doi:10.1016/j.jcomdis.2020.106070
- Des Roches, C.A., Mitko, A. & Kiran, S. (2017). Relationship between Self-Administered Cues and Rehabilitation Outcomes in Individuals with Aphasia: Understanding Individual Responsiveness to a Technology-Based Rehabilitation Program. Frontiers in Human Neuroscience, 11, 7, doi: 10.3389/fnhum.2017.00007
- Des Roches, C.A., Balachandran, I., Ascenso, E.M.,Tripodis,Y., & Kiran, S. (2015). Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform. Frontiers of Human Neuroscience, 8, 1015, doi: 10.3389/fnhum.2014.01015
- Dignam, J. K., Rodriguez, A. D., & Copland, D. A. (2016). Evidence for intensive aphasia therapy: Consideration of theories from neuroscience and cognitive psychology. Journal of Injury, Function & Rehabilitation, 8, 254–267. https://doi.org/10.1016/j.pmrj.2015.06.010
- Druks, J. & Masterson, J. (2000) An Object Action Naming Battery. Hove: Psychology Press.
- Edmonds, L. A., Obermeyer, J., & Kernan, B. (2015). Investigation of pretreatment sentence production impairments in individuals with aphasia: Towards understanding the linguistic variables that impact generalisation in verb network strengthening treatment. Aphasiology, 29, 1312–1344. doi:10.1080/02687038.2014.975180
- Edmonds, L. A., Mammino, K., & Ojeda, J. (2014). Effect of verb network strengthening treatment (VNeST) in persons with aphasia: Extension and replication of previous findings. American Journal of Speech-Language Pathology, 23, S312–29. doi:10.1044/2014_AJSLP-13-0098
- Floel, A. (2019). Computerised speech and language therapy in post-stroke aphasia. The Lancet Neurology, 18, 806–807.
- Godlove, J., Anantha, V., Advani, M., Des Roches, C. and Kiran, S. (2019). Comparison of Therapy Practice at Home and in the Clinic: A Retrospective Analysis of the Constant Therapy Platform Data Set. Frontiers in Neurology, 10, Article 140. doi: 10.3389/fneur.2019.00140
- Harrison, M., Palmer, R. & Cooper, C. (2020). Factors associated with adherence to self-managed aphasia therapy practice on a computer—a mixed methods study alongside a randomized controlled trial. Frontiers in Neurology. doi: 10.3389/fneur.2020.582328
- Helm-Estabrooks, N. & Ramsberger, G. (1986) Treatment of agrammaticism in long term Broca’s aphasia. British Journal of Disorders of Communication, 21, 39–45.
- Hickin, J., Cruice, M. & Dipper, L. (2022). A systematically conducted scoping review of the evidence and fidelity of treatments for verb and sentence deficits in aphasia: sentence treatments. American Journal of Speech Language Pathology, 31:1, 431–462. https://doi.org/10.1044/2021_AJSLP-21-00120
- Hickin, J., Cruice, M. & Dipper, L. (2020). A systematically conducted scoping review of the evidence and fidelity of treatments for verb deficits in aphasia: verb in isolation treatments. American Journal of Speech Language Pathology, 29, 530–559. https://doi.org/10.1044/2019_AJSLP-CAC48-18-0234
- Hoffman, T.C., Paul P Glasziou, P.P., Boutron, I., Milne, R., Perera, R., Moher, D., Altman, D.G., … Michie, S. (2014). Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. British Medical Journal, 348,g1687 doi: 10.1136/bmj.g1687
- Hope, T., Nardo, D., Holland, R., Ondobaka, S., Akkad, H., Price, C. J., Leff, A. & Crinion, J. (2021). Lesion site and therapy time predict responses to a therapy for anomia after stroke: a prognostic model development study. Scientific Reports, 11, 18572. doi: 10.1038/s41598-021-97916-x
- Kearns, Á., Kelly, H., & Pitt, I. (2019). Self-reported feedback in ICT-delivered aphasia rehabilitation: A literature review. Disability and Rehabilitation, 1–15. doi:10.1080/09638288.2019.1655803
- Kleim, J.A. & Jones, T.A. (2008). Principles of Experience-Dependent Neural Plasticity: Implications for Rehabilitation After Brain Damage. Journal of Speech, Language, and Hearing Research, 51, S225–S239.
- Kopelman, M.D., Wilson, B.A. & Baddeley, A.D. (1989). The autobiographical memory interview: A new assessment of autobiographical and personal semantic memory in amnesic patients, Journal of Clinical and Experimental Neuropsychology, 11, 724–744, DOI: 10.1080/01688638908400928
- Kurland, J., Liu, A. and Stokes, P. (2018). Effects of a tablet-based home practice program with telepractice on treatment outcomes in Chronic aphasia. Journal of Speech, Language, and Hearing Research, 61, 1140–1156. https://doi.org/10.1044/2018_JSLHR-L-17-0277
- Lavoie, M., Macoir, J., & Bier, N. (2017). Effectiveness of technologies in the treatment of post-stroke anomia: A systematic review. Journal of Communication Disorders, 65, 43–53. http://dx.doi.org/10.1016/j.jcomdis.2017.01.001
- Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A. & Zoghaib, C. (1989) The Communicative Effectiveness Index: development and psychometric evaluation of a functional communication measure for adult aphasia. Journal of Speech and Hearing Disorders, 54, 113–124.
- Marshall, J., Booth, T., Devane, N., Galliers, J., Greenwood, H., Hilari, K. … Woolf, C. (2016). Evaluating the benefits of aphasia intervention delivered in virtual reality: Results of a quasi-randomised study. PLoS ONE, 11(8). doi:10.1371/journal.pone.0160381.
- Medical Research Council (2006) Developing and evaluating complex interventions:new guidance. Available at: https://webarchive.nationalarchives.gov.uk/ukgwa/20220207162925/http://mrc.ukri.org/documents/pdf/complex-interventions-guidance/. [Accessed 31st March 2022].
- National Institute for Health Research Clinical Research Network: Stroke. (2014). Engaging with people who have aphasia: A set of resources for stroke researchers” Author: Pearl, G.
- Newton, C., Kirby, P., & Bruce, C. (2017). Getting into shape: The effect of shape coding on the spoken language production of two men with chronic aphasia. Aphasiology, 1–23. doi:10.1080/02687038.2017.1306639
- NICE Guidelines. Stroke in Adults: Quality statement 2: Intensity of stroke rehabilitation. Available at: https://www.nice.org.uk/guidance/qs2/chapter/Quality-statement-2-Intensity-of-stroke-rehabilitation. [Accessed 31st March 2022].
- Palmer, R., Dimairo, M., Cooper, C., Enderby, P., Brady, M., Bowen, A. et al. (2019). Self-managed, computerised speech and language therapy for patients with chronic aphasia post-stroke compared with usual care or attention control (Big CACTUS): a multicentre, single-blinded, randomised controlled trial. Lancet Neurology, 18, 821–33
- Palmer R, Witts H, Chater, T. (2018). What speech and language therapy do community dwelling stroke survivors with aphasia receive in the UK? PLoS ONE 13, e0200096. https://doi.org/10.1371/journal.pone.0200096
- Palmer, R., Enderby, P. & Paterson, G. (2013). Using computers to enable self-management of aphasia therapy exercises for word finding: the patient and carer perspective. International Journal of Language & Communication Disorders, 48, 508–521.
- Raymer, A. M., Beeson, P., Holland, A., Kendall, D., Maher, L. M., Martin, N., … Gonzalez Rothi, L. J. (2008). Translational research in aphasia: From neuroscience to neurorehabilitation. Journal of Speech, Language, and Hearing Research (JSLHR), 51, S259–S275.
- Renvall, K., Nickels, L. & Davidson, B. (2013a). Functionally relevant items in the treatment of aphasia (part I): Challenges for current practice. Aphasiology, 27, 636–650, doi:10.1080/02687038.2013.786804
- Renvall, K., Nickels, L. & Davidson, B. (2013b). Functionally relevant items in the treatment of aphasia (part II): Further perspectives and specific tools. Aphasiology, 27, 651–677, doi:10.1080/02687038.2013.796507
- Repetto, C., Paolillo, M.P.,Tuena, C., Bellinzona, F. & Riva, G. (2021). Innovative technology-based interventions in aphasia rehabilitation: a systematic review, Aphasiology, 35, 1623–1646, doi: 10.1080/02687038.2020.1819957
- Scobbie, L., McLean, D., Dixon, D., Duncan, E. & Wyke, S. (2013). Implementing a framework for goal setting in community based stroke rehabilitation: a process evaluation. BMC Health Services Research, 13, 190. http://www.biomedcentral.com/1472-6963/13/190
- Scobbie, L., Dixon, D. & Wyke, S. (2011). Goal setting and action planning in the rehabilitation setting: development of a theoretically informed practice framework. Clinical Rehabilitation, 25, 468–482.
- Spell, L. A., Richardson, J. D., Basilakos, A., Stark, B. C., Teklehaimanot, A., Hillis, A. E., & Fridriksson, J. (2020). Developing, implementing, and improving assessment and treatment fidelity in clinical aphasia research. American Journal of Speech-Language Pathology, 29, 286–298. doi:10.1044/2019_AJSLP-19-00126
- Swales, M.A., Hill, A.J. & Finch, E. (2016). Feature rich, but user friendly: Speech pathologists’ preferences for computer-based aphasia therapy, International Journal of Speech-Language Pathology, 18, 315–328, doi:10.3109/17549507.2015.1081283
- Swinburn, K., Porter, G., and Howard, D., (2004). The Comprehensive Aphasia Test. Hove: Psychology Press.
- Tate, R., L, Perdices, M., Rosenkoetter, U., et al. (2016). The Single-Case Reporting Guideline In BEhavioural Interventions (SCRIBE) 2016 Statement. Journal of Clinical Epidemiology 73, 142–152.
- van der Meulen, I., van de Sandt-Koenderman, M.E., Duivenvoorden, H.J. & Ribbers, G.M. (2010). Measuring verbal and non-verbal communication in aphasia: reliability,validity, and sensitivity to change of the Scenario Test. International Journal of Language and Communication Disorders, 45, 424–435.
- Wambaugh, J. L., Mauszycki, S., & Wright, S. (2014). Semantic feature analysis: Application to confrontation naming of actions in aphasia. Aphasiology, 28, 1–24. doi:10.1080/02687038.2013.845739
- Wambaugh, J.l. & Ferguson, M. (2007). Application of semantic feature analysis to retrieval of action names in Aphasia. Journal of Rehabilitation Research and Development, 44, 381–394.
- Webster, J., Franklin. S. & Howard, D. (2007) An analysis of thematic and phrasal structure in people with aphasia: What more can we learn from the story of Cinderella? Journal of Neurolinguistics, 20, 363–394.
- Whitworth, A., Perkins, L. & Lesser, R. (1997) Conversation Analysis Profile for People with Aphasia. Whurr: London.
- Zheng, C., Lynch, L. & Taylor, N. (2016). Effect of computer therapy in aphasia: a systematic review, Aphasiology, 30:2-3, 211–244, DOI: 10.1080/02687038.2014.996521