Abstract
Objectives: Severe traumatic brain injury (TBI) is a potentially devastating insult to the brain with high rates of fatality and neurological deficits. TBI can result in substantial costs to the centre providing care. We sought to present the experience of a Major Trauma Centre (MTC) and ascertain the financial implications of this healthcare provision, in particular detailed costs, reimbursement and the surplus or deficit accrued by the centre.
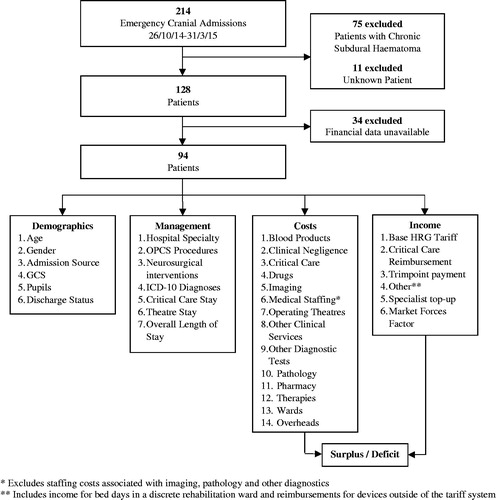
Design: All cranial non-elective neurosurgical admissions with a TBI over 4.5 months (26 October 2014 to 15 March 2015) were analysed retrospectively, excluding cases of chronic subdural haematoma, at an MTC in England. Demographic data were collected alongside detailed cost and income data.
Results: Ninety four patients were identified. The majority of patients presented with more than one diagnosis of cranial trauma. Average length of stay was 18.8 ± 21.6 days. Total deficits as a result of treating this cohort amounted to £558,034. There was a significant association between (i) more complex presentations and (ii) a longer length of stay and the deficit accrued by the centre. The major drivers of the financial outcome were costs associated with wards, medical staffing and overheads.
Conclusion: There was a substantial deficit accrued as a result of the management of patients with TBI at an MTC. The more complex the presentation, extensive the intervention, and lengthy the stay, the greater the deficit accrued by the centre. The current tariff payment system is not effectively reflecting the severity of injury or intensity of management of patients with TBI.
Introduction
Traumatic brain injury (TBI) remains the cause of approximately half of deaths secondary to trauma, the most common cause of death for those under the age of 35 in England and Wales.Citation1,Citation2 Complications of TBI include seizures, meningitis, hydrocephalus, cranial nerve and pituitary dysfunction, and long-term cognitive and emotional difficulties.Citation3 Commonly affecting children and young adults, the socioeconomic implications of a TBI and its complications can be profound. Challenges in the management of patients with TBI range from the importance of subspecialist trauma neurosurgical input throughout the acute hospitalisation phase in a large cohort, to major difficulties in securing rehabilitation services following discharge to the community.Citation4
There is existing evidence demonstrating that acute hospitalisation costs to treat patients with TBI are substantial and vary considerably. A population-based cohort study in Ontario published mean acute care costs for TBI of $19,083 (standard deviation $72,495) in the first year of injury.Citation5 Hospitalisation costs in a multihospital database in the USA ranged from an average of $8189 for moderate, $14,603 for serious, $16,788 for severe, to $33,537 for critical TBI.Citation6 In England and Wales, data from the Trauma Audit Research Network identified an average hospitalisation cost of TBI of £15,462 (standard deviation £16,844). Consistent with other national studies, there was substantial variation in cost depending on the Glasgow Coma Scale (GCS), age, Injury Severity Score, coexisting injuries and provision of neurosurgical services.Citation7
Whilst large-scale multicentre data on the costs of head injury exist, there remains very limited research regarding the associated income hospitals receive for providing care for patients with head injuries. A previous multicentre study in Australia reviewed the clinical coding and associated financial information of major trauma which included TBI, concluding that coding classifications were not commensurate with the expense of treatment.Citation8
TBI funding specifically in England is coordinated through tariffs as part of the National Tariff Payment System. This is an activity-based tariff payment system where healthcare providers are paid based on the number of procedures completed, and in 2014/15 amounted to £30 billion (27% of NHS England expenditure).Citation9 Studies leveraging this tariff data are extremely limited; to our knowledge only one study has undertaken a single centre evaluation based on tariff information, which presented data relating to hospital costs of out-of-hospital cardiac arrest patients treated in intensive care.Citation10
Therefore, we sought to conduct a service evaluation study in the UK to ascertain the financial outcome (the surplus and deficits as a result of providing the service) of providing tertiary centre care for patients with TBI in the National Health Service (NHS). We hypothesised that complex admissions were not adequately funded with the current tariff structure, and the more severely injured patients represented those admissions with the greatest financial deficits for the hospital providing the care.
Materials and methods
All cranial non-elective neurosurgical admissions with a TBI over 4.5 months from 26 October 2014 to 15 March 2015 were analysed retrospectively, excluding cases of chronic subdural haematoma, at Addenbrooke’s Hospital, the Major Trauma Centre (MTC) for the East of England. The date range was limited by the first day following the introduction of an electronic patient records system and the most recent date where full detailed financial data were available at the time the project was undertaken. Details of the admission source, admission GCS,Citation11 admission pupillary reactivity, nature of the neurosurgical management (including interventions and location), status at discharge, and basic demographic data were collected through the electronic patient record system. Data were also collected for the main hospital specialty involved, lengths of stay in critical care and in the centre, procedures performed with OPCS Classification of Interventions and Procedures (OPCS) coding, and diagnoses made with the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10).
Financial data were ascertained through collaboration with the hospital finance department. Cost data were collected leveraging the Patient Level Information Costing System (PLICS) for detailed cost pooling across 15 categories.Citation12 A breakdown of costs into fixed (costs that do not change over a 12-month period such as annual contracts), semi-fixed (costs that move with activity changes on a small scale, but jump or step up when a certain threshold is reached) and variable (costs directly affected by activities related to the patient such as drug costs) was also available.Citation13 Income data were also collected with specified components for analysis, reflecting all income received by the hospital for the clinical care of each patient. Specific adjustments to the national tariff for each treatment were identified to present the total remuneration for the centre as a result of the clinical care of each admission. Each admission was coded with a Healthcare Resource Group; national standard groupings of clinically similar treatments which use common levels of healthcare resource. Adjustments for the local economy (the Market Forces Factor), uplifts for the provision of specialist care (specialist top-up) and additional payments for critical care admissions or admissions beyond the forecasted length of stay specified by the HRG (trimpoint) were combined to present the total income for each admission.
Financial data were tested for normality assumptions using the Shapiro–Wilk test. The Kruskal–Wallis test was used for non-parametric group-wise comparisons of financial data for factors relating to the presentation of the patient. Components of costs and income were correlated with Pearson’s r to the financial outcome to identify potential drivers. All statistical analyses were performed in R.Citation14 Sub-group data were reviewed for patients with isolated TBI. This was defined as the absence of extracranial injuries that would require admission within their own right.Citation15 A second sub-group of 20 patients was developed representing the most significant deficits incurred by the centre as a result of treating the cohort, including patients with both isolated TBI and polytrauma. The project was registered as a service evaluation project with Cambridge University Hospitals NHS Foundation Trust. According to NHS Health Research Authority guidance, service evaluation projects do not require research ethics committee review.
Results
A total of 214 patients were identified initially. Following exclusion of cases with chronic subdural haematoma, and identification of cases where detailed PLICS data were available, a total of 94 patients were included in the detailed analysis ().
Total costs to treat the cohort of patients amounted to over £1.94 million, whilst income amounted to £1.38 million. Consequently, the hospital accrued a total financial deficit of £558,034 as a result of treating this cohort of patients. Financial data were not found to be normally distributed under the Shapiro–Wilk test (W = 0.712, p<.0001), thus non-parametric testing was performed for group-wise comparisons.
Descriptive statistics of the final cohort is provided in . The sample included was 75.5% male, with a mean age of 41.3 years. The majority of patients presented with mild TBI (GCS 13–15 n = 56, 56.2%) and with both reactive pupils (n = 76, 80.9%). All patients included in the analysis were initially managed in either critical care or with ward care in a dedicated Neurosciences Unit (NSU). There was a significantly lower length of stay recorded in patients with isolated TBI (mean 13.9 ± 15.8 days) relative to the total cohort (mean 18.8 ± 21.6 days, χ2=12.20, p<.001). A total of 11 patients died during their admission (11.7%). Clinical vignettes for three admissions (greatest deficit, greatest surplus and admission involving a craniotomy only) are provided in the Supplementary Material.
Table 1. Descriptive statistics of final cohort of 94 patients and subgroup of 67 patients with isolated TBI. Values shown are mean values with standard deviations in parentheses unless otherwise specified.
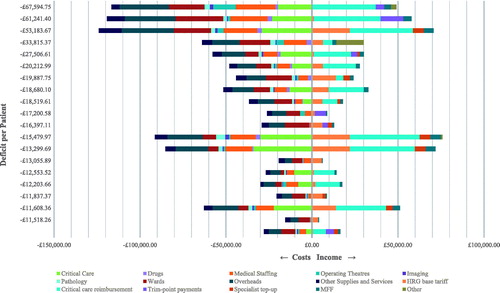
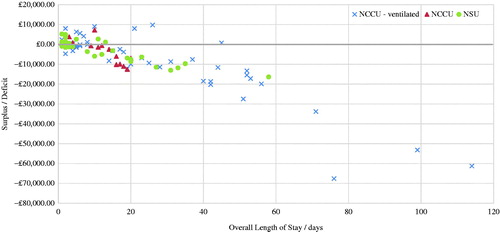
Deficits increased proportionately to the level of care required for the patient (). Financial deficits were higher in admissions requiring ventilation in critical care (n = 43, deficit −£9712±£17,264) relative to the deficits observed in patients admitted to critical care without ventilation (n = 16, deficit −£3125±£5715), and patients admitted to the NSU only (n = 35, deficit −£2584±£5336, χ2=4.00, p=.046).
Table 2. Financial information relating to type of neurosurgical intervention and level of care in the cohort of 94 patients, and subgroup of 67 patients with isolated TBI. Values shown are mean values with standard deviations in parentheses unless otherwise specified.
All neurosurgical interventions were associated with a financial deficit (). Greatest deficits were recorded in admissions managed with a decompressive craniectomy with intracranial pressure (ICP) monitoring (n = 2, deficit −£22,581 ± 43,279), and ICP monitoring alone (n = 9, deficit −£22,235 ± 26,307). Notably, the average HRG tariff (excluding extra reimbursement for critical care and excessive length of stay) for the implantation of an ICP monitor alone (n = 9, tariff £7142±£7110) exceeded the reimbursement for a craniotomy alone (n = 11, tariff £5346±£1965, Supplementary Material Table S1). Despite the fact that all admissions involved regular review by the neurosurgery team on dedicated neuroscience or critical care wards, only 38 (40.4%) of cases received a specialist top-up.
All ICD-10 diagnoses were associated with admissions that accrued a deficit (). Furthermore, the higher the number of the cranial diagnoses in a single admission, the greater the costs. This was accompanied with increased income, but disproportionately so. Subsequently, admission of patients with more complex injuries resulted in greater financial deficits for the hospital.
Table 3. Financial information relating to diagnoses in the cohort of 94 patients, and subgroup of 67 patients with isolated TBI. Values shown are mean values with standard deviations in parentheses unless otherwise specified.
Length of stay and its association with financial surplus/deficit is presented in . There was a significant correlation between overall length of stay and the financial outcome for the MTC (r= −.77, p<.001). All admissions with a length of stay in excess of 45 days resulted in a deficit for the centre. Brief descriptions of admissions with the greatest surplus, greatest deficit and length of stay in excess of 60 days are provided in the Supplementary Material. Taking all admissions with a length of stay of 17 days or less, the hospital generated a net surplus of £6402.
Figure 2. Surplus/deficit in neurosurgical admissions and relationship to length of stay. NCCU: Neurosciences Critical Care Unit; NSU: Neurosciences Unit.
For the overall cohort, strongest correlations with the amount of deficit or surplus accrued by the MTC were observed for costs related to wards (r=.84, p<.001), medical staffing (r=.79, p<.001) and overheads (r=.85, p<.001). Together, these categories made up the majority of total costs in the cohort (mean 61%, range 25–97%). There was little variation in total costs attributed as variable (mean 17.0 ± 4.6%), semi-fixed (60.7 ± 6.9%) and fixed costs (22.2 ± 5.0%). Specific fixed, semi-fixed and variable costs for each PLICS cost category were not available.
A total of 32 different HRGs were coded for tariff reimbursement (Supplementary Material Table S2). A financial surplus was associated with six of the identified HRGs. Four cases were coded as ‘Data invalid for grouping’, despite two of these cases involving a critical care admission and ICP monitor implantation.
The 20 admissions associated with the greatest financial deficits amounted to £467,214 (83.7% of cohort total). Subgroup demographic information is provided in the Supplementary Material (Table S3). Detailed cost and income data were reviewed and presented in . Average overall length of stay for this subgroup of patients was 50.4 days, with an average of 20.0 days in critical care and 5.8 h in theatre during their admission. Nine admissions were for isolated TBI, with 18 of the 20 patients admitted under the neurosurgery team. Fifteen of the 20 patients (75.0%) were ventilated in the critical care unit at some point of their admission. All patients survived.
Discussion
The results present the financial implications of the provision of care as an MTC in England over a period of 4.5 months for TBI. Excluding cases of chronic subdural haematoma, a total of 94 cases were identified. Total financial deficits accrued by the hospital in managing these admissions amounted to nearly £600,000. A minority of patients presented with a single cranial diagnosis; the majority were complex presentations requiring extensive interventions. Average cost data was somewhat higher than previously published national data from 2000 to 2005 in England and Wales (£20,651 vs. £15,462).Citation7
Critical care admission was associated with a substantially greater deficit. Average deficits for admissions with multiple cranial diagnoses were over three times greater than admissions with a single diagnosis. There was clear evidence to suggest that an increased length of stay was associated with a greater financial deficit. A total of 10 admissions extended beyond the trimpoint specified by the national tariff, only half of which referred to admissions with lengths of stay in excess of 50 days. The data therefore does not suggest that the admissions resulted in financial deficits as a result of excessive admission lengths compared to the national average (from which trimpoint are calculated).
Drivers of deficits accrued by the MTC included costs relating to wards, medical staffing and overheads. Unfortunately, identification of variable, semi-fixed and fixed costs within these categories was not possible. It is therefore not clear to what extent these reported costs are modifiable. With regards to income, the results identified a large number of HRG codes for these presentations. The HRG assigned to an admission is based off the combination of ICD-10 diagnoses and OPCS procedures reported in the notes, submitted to a national algorithm that determines the appropriate HRG. Each HRG has its respective tariff, and thus the centre is reimbursed. There is evidence to suggest that the tariff system is not effectively reflecting the severity of injury or intensity of management of patients with TBI; substantial variations were observed for similar levels of treatment intensity, while on several occasions the HRG coded was invalid for grouping. It is also unclear how the specialist top-up is allocated, given that all admissions involved care within the neurosciences department of an MTC with a catchment population in excess of four million.
Future directions
Although detailed financial data has been presented, further work is required to include cost-effectiveness analysis, with calculation of cost per quality-adjusted life year (QALY) and its relationship to the financial outcome in managing TBI as a tertiary centre. As these are the results of only one centre, further work is recommended with a multi-centre design to minimise bias. Such additional work could complement recently published research comparing the cost-effectiveness of management of severe TBI in neurocritical care versus general critical care units within neuroscience centres.Citation16 In addition, it may be useful to undertake specific analysis of procurement costs in order to identify cost saving opportunities and underpin policies for reimbursing TBI services appropriately.Citation17
Limitations
There are some limitations to this analysis. First, although this analysis benefits from the greatly improved granularity of the PLICS cost data, the provided data still leaves challenges in investigating areas for cost improvement work. Although fixed, semi-fixed and variable costs were available at the gross level for the overall admission, they were not available at the level of PLICS category. Such a breakdown of costs would enable greater focus for cost improvement programmes in the provision of care for patients with TBI. This study was furthered limited by a small sample size (n = 94) with a significant heterogeneity of presentations and interventions in patients with TBI. Consequently, caution is recommended in interpretation of sub-group analysis given such small sample sizes. However, our selection criteria included all possible patients admitted for TBI to an MTC excluding those with chronic subdural haematoma. Subsequently, our findings are representative of the case mix and financial outcome of running a TBI service at an MTC.
Conclusion
TBI remains a common presentation often requiring intensive and lengthy hospital admissions in cases of severe injuries. This study performed at a MTC identified a significant financial deficit associated with the provision of care for these patients. Furthermore, this financial deficit was significantly associated with intensity of management, severity of injury and overall length of stay. The major drivers of financial deficit were related to the costs of admission specifically related to costs associated with overheads, wards and medical staffing. There was substantial heterogeneity in the HRG tariffs coded for the admissions included. The current tariff payment system is not effectively reflecting the severity of injury or intensity of management of patients with TBI.
Acknowledgements
We would like to thank Emma Glover, Daniel Auberson and Jackie Neve for their help collecting the financial data for this analysis.
Disclosure statement
The authors report no declarations of interest.
Funding
PJH is supported by a NIHR Research Professorship and the NIHR Cambridge Biomedical Research Centre.
References
- Wilson MH, Kolias AG, Hutchinson PJ. Neurotrauma – a multidisciplinary disease. Int J Clin Pract 2014;68:5–7. doi:10.1111/ijcp.12246.
- Fuller G, Bouamra O, Woodford M, et al. Temporal trends in head injury outcomes from 2003 to 2009 in England and Wales. Br J Neurosurg 2011;25:414–21. doi:10.3109/02688697.2011.570882.
- Kolias AG, Guilfoyle MR, Helmy A, et al. Traumatic brain injury in adults. Pract Neurol 2013;13:228–35. doi:10.1136/practneurol-2012-000268.
- Mendelow AD, Timothy J, Steers JW, et al. Management of patients with head injury. The Lancet 2008;372:685–7. doi:10.1016/S0140-6736(08)61280-5.
- Chen A, Bushmeneva K, Zagorski B, et al. Direct cost associated with acquired brain injury in Ontario. BMC Neurol 2012;12:76. doi:10.1186/1471-2377-12-76.
- McGarry LJ, Thompson D, Millham FH, et al. Outcomes and costs of acute treatment of traumatic brain injury. J Trauma 2002;53:1152–9. doi:10.1097/01.TA.0000025801.33552.71.
- Morris S, Ridley S, Lecky FE, et al. Determinants of hospital costs associated with traumatic brain injury in England and Wales. Anaesthesia 2008;63:499–508. doi:10.1111/j.1365-2044.2007.05432.x.
- Curtis K, Lam M, Mitchell R, et al. Major trauma: the unseen financial burden to trauma centres, a descriptive multicentre analysis. Aust Health Rev Publ Aust Hosp Assoc 2014;38:30–7. doi:10.1071/AH13061.
- Monitor. 2014/15 national tariff payment system: Annex 4A. London, UK: NHS England; 2013.
- Petrie J, Easton S, Naik V, et al. Hospital costs of out-of-hospital cardiac arrest patients treated in intensive care; a single centre evaluation using the national tariff-based system. BMJ Open 2015;5:e005797. doi:10.1136/bmjopen-2014-005797.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. The Lancet 1974;304:81–4. doi:10.1016/S0140-6736(74)91639-0.
- Monitor. 2013/14 patient level cost collection: review and lessons for the future. London, UK: Monitor; 2015:7. Available from: https://www.gov.uk/government/publications/patient-level-cost-collection-201314-review-and-lessons-for-the-future.
- Monitor. Approved costing guidance updated February 2016. London, UK: Monitor; 2016:79.
- R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2008. Available from: http://www.R-project.org/.
- MRC CRASH Trial Collaborators. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 2008;336:425–9. doi:10.1136/bmj.39461.643438.25.
- Grieve R, Sadique Z, Gomes M, et al. Risk Adjustment In Neurocritical care (RAIN) Study Investigators. An evaluation of the clinical and cost-effectiveness of alternative care locations for critically ill adult patients with acute traumatic brain injury. Br J Neurosurg 2016;30:388–96. doi: 10.3109/02688697.2016.1161166.
- Alali AS, Burton K, Fowler RA, et al. Economic evaluations in the diagnosis and management of traumatic brain injury: a systematic review and analysis of quality. Value Health 2015;18:721–34. doi: 10.1016/j.jval.2015.04.012.