Abstract
Purpose: Meningiomas are the commonest predominantly non-malignant brain tumour in adults. The use of surgery appears to be increasing, and outcomes are thought to be good, but whole nation data for England is scarce. The aim of this report is to examine the epidemiology of patients operated for cranial and spinal meningioma in England, and to assess associations between outcomes and gender, age, meningioma site (cranial or spinal), and grade.
Material and methods: A search strategy encompassing all patients coded with cranial and spinal meningioma treated between January 1999 and December 2013 was obtained from data linkage between the National Cancer Registration and Analysis Service and Hospital Episode Statistics for England.
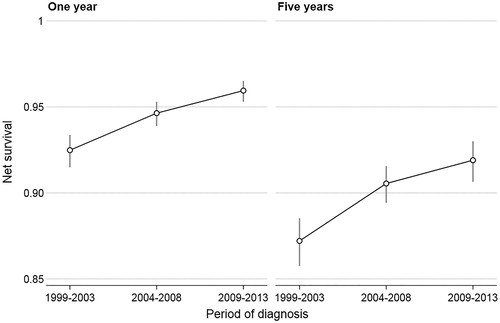
Results: 25,694 patients were diagnosed with meningioma in England between 1999 and 2013, in whom 24,302 were cranial and 1392 spinal. Of these patients, 14,229 (60%) cranial and 1188 (85%) spinal meningioma received surgery. Of those operated on 70.1% were women, and, where the tumour grade was recorded, 79.5% were WHO grade I, 18.4% grade II, and 2.1% grade III. Five and ten year net survival rates for surgically treated cranial meningiomas were respectively 90% and 81% for those with WHO grade I, 80% and 63% for grade II, and 30% and 15% for WHO grade III tumours. Overall survival after surgery is better in women, younger adults, and people with spinal or lower grade meningiomas. Outcomes have improved over the time period examined.
Conclusion: The outcome for patients with meningioma is good and is improving. However, there remains a significant mortality related to the disease process.
Introduction
Meningiomas are a group of mostly non-malignant, slow-growing tumours of the central nervous system that are thought to be derived from the meningothelial cells of the arachnoid layer ().Citation1 They account for 37% of brain tumours overall and 39% of spinal tumours, have a reported cranial incidence of 8.3/100,000 in the United States (US), are more common in older people, in people of Afro-Caribbean ethnicity, and in women (2.2 to 1).Citation2 They are increasingly found incidentally, with only 43% diagnosed from histological confirmation in the US, and are mostly World Heath Organization (WHO) grade I (80.6%), with fewer being of higher grades (Grade II 17.4%, and grade III 2.1%).Citation2 Common clinical symptoms include headache, progressive neurological deficit, and seizures. Management options include active monitoring, symptom control, surgical excision, external beam radiotherapy (EBRT), and stereotactic radiosurgery (SRS).Citation3 Maximal surgical excision remains the mainstay of treatment for all grades of cranial and spinal meningioma, but cranial SRS and EBRT are increasingly used.Citation3,Citation4
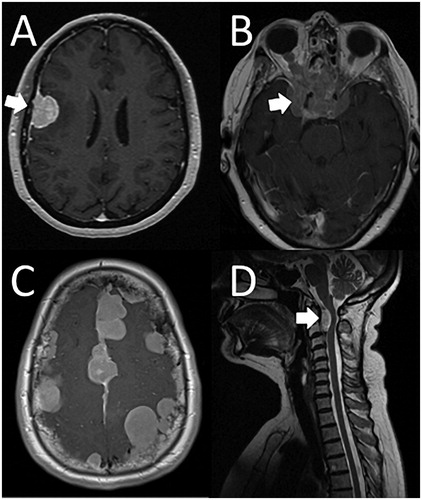
Figure 1. Meningioma clinical variety. A. Patient presented with a seizure and left hemiparesis, and had a WHO grade II meningioma excised uneventfully. B. Patient presented with visual deterioration, and had 2 surgeries, and radiotherapy over a 20 year period for a WHO grade I meningioma. Vision deteriorated further and the meningioma continued to grow. C. Patient with NF2 and multiple meningiomas presented de novo with headache at 52 yrs old. D. Patient presented with progressive weakness (Figure 1D courtesy of Dr S Mills, The Walton Centre, Liverpool).
There is little multicentre United Kingdom data published on outcome after surgery for meningiomas. In 2013 English cancer registry data were centralized allowing ready exploration of national data on patients with brain tumours across the whole of England (56.1 million people in 2011, Office for National Statistics). The data are linked to information on hospital admissions (Hospital episode statistics: HES), which include treatment related to surgery, and pathology and radiology reports. In addition, multidisciplinary team meetings (MDTs; or tumour boards) feed diagnostic and therapy data directly to the National Cancer Registration and Analysis Service (NCRAS). This makes England unique in having detailed whole nation incidence and treatment data for all patients diagnosed with a brain tumour. The aim of this study was to examine the epidemiology of patients having surgery for meningiomas, and the long-term outcome related to the age and sex of the patient, the site (cranial or spinal), and grade, over a 15 year period for the whole of England.
Methods
A retrospective population based search examined data from NCRAS, linked to Hospital Episode Statistics (HES), between 1st January 1999 and 31st December 2013 (a 15-year period). International Classification of Diseases (ICD) 10 O2 site codes used were C70, D32, and D42, ICD10 morphologies 9530–9539 and some M8000 in clinical/imaging diagnoses, and ICD10 O2 behaviours 0, 1, and 3 for WHO grades I (benign), II (atypical), and III (malignant) respectively. Vital status was checked using the NHS Personal Demographics Service (PDS) (http://systems.hscic.gov.uk/demographics/pds/).
Net survival percentages were calculated using the STRS (www.pauldickman.com/rsmodel/stata_colon/) commands respectively in Stata version 13.1 SE (http://www.stata.com). Net survival is the survival that would be observed if the only possible underlying cause of death was the disease under study.Citation5 Net survival was used as an adjunct to absolute survival, as patients with meningiomas can live for extended periods, and net survival takes into account expected mortality among patients of similar age and gender. Net survival therefore allows an assessment of the additional morbidity associated with the disease process.
Results
In England, between 1st Jan 1999 and 31st December 2013, 25,694 patients (71.1% female) were diagnosed with meningioma, of which 24,302 were cranial and 1390 were spinal (). Within this group, 15,417 (70.1% female) had surgery, 14,229 were cranial and 1188 were spinal. Meningioma numbers increased with increasing age, with a mean age at treatment of 57.5 years (standard deviation 14.4, range 0 – 98 years). This compared to a mean age of 73.9 of those who didn’t have surgery (range 0 – 104). Three times more women than men had surgery. 79.5% of tumours were WHO grade I, 18.4% grade II, and 2.1% grade III.
Table 1. Demographics of patients with meningioma treated with surgery in England 1999–2013.
Five and ten year net survival for cranial meningiomas were respectively 90% and 81% for WHO grade I, 80% and 63% for grade II, and 30% and 15% for WHO grade III tumours ( and ). There was a significant reduction in 5 year net survival over the age of 69 years, to less than 83% in men and 87% in women (). This means that 27% of men age 70 to 79 years who had surgery for a cranial Meningioma died within 5 years over and above what would be expected for their age, and hence may be attributable to their meningioma, treatment, or complications thereof. Patients with spinal meningiomas did better in all grades, gender and ages (, ). Women had better outcomes than men at all ages, both cranial and spinal locations, and grades.
Figure 2. Long term outcomes. Kaplan Meier estimates of overall survival by grade and site of patients with histologically confirmed (operated) meningiomas in England 1999–2013. G1: WHO grade I, G2: WHO grade II, G3: WHO grade III, GX: WHO grade unrecorded.
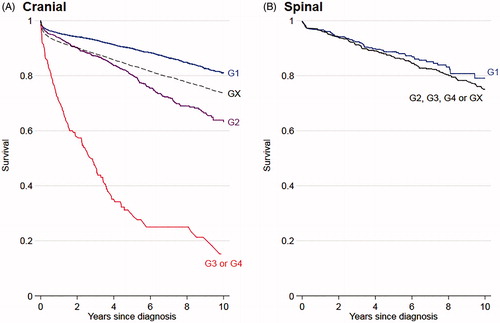
Figure 3. Influence of age. Net survival at 1 and 5 years for patients with WHO grade I cranial meningiomas diagnosed histologically (operated) 1999–2013 by age and sex.
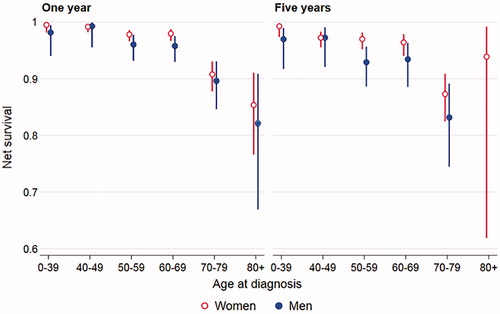
Table 2. Outcome for patients with meningioma in England treated with surgery 1999–2013.
Surgical outcomes improved over the 15-year period (). For both cranial and spinal meningiomas, in both genders, and at all ages and grades of tumour at both 1 and 3 years there was an improvement in net survival.
Discussion
More than 2000 patients are diagnosed with meningioma each year in England, with more than half receiving cranial or spinal surgery. Numbers have been increasing year-on-year, with 52% more diagnoses and 58% more resections in 2013 than 1999. Five and ten year survival rates post-surgery are high, and are increasing over time.
Meningiomas are the commonest primary cranial tumour type in adults, and are unsurprisingly the commonest cranial tumour operation.Citation2,Citation6 Incidence data published suggest 5.3 per 100,000 person years in the UK (7.19 for women, 3.05 for men), and an age adjusted rate of 8.14/100,000 in the US, but those may both be underestimates as rates of up to 2.3% at post-mortem have been suggested.Citation2,Citation7 Meningiomas are known to be more common with greater body adipose mass, which may relate to hormone responsiveness.Citation2,Citation8,Citation9 Growing obesity levels, as well as an ever increasing elderly population and the availability and use of brain imaging imply this number will continue to grow over time.
An examination of the demographic features shows consistency with previous reports in other nations.Citation2 A female preponderance is present for both cranial and spinal meningiomas (71.1% occur in women overall), which is consistent throughout the literature.Citation2 Meningiomas are more common with advancing age, and the peak operative age band was 60–69 years. The definition of meningioma grade has altered over the study period with three iterations of the WHO Classification of Tumours of the Nervous System.Citation1,Citation10,Citation11 These alterations have refined the diagnostic criteria for grade II meningiomas including brain invasion in the 2007 classification, which has led to a reported increase in incidence over the last 15 years, so the total figures provided in the current study should overestimate slightly the true incidence of grade I tumours, and underestimate that for grade II if histological examination were to repeated using the 2016 WHO classification.Citation12 The rates of grade I, II, and III tumours presented are however so similar to that from recent US reports (80.4% vs 79.5% for grade I, 17.4% vs 18.4% for grade II, and both at 2.1%) that it appears this change has not made a significant difference. This might be due to the US figures not incorporating the newer histological grading scheme, that some pathologists may have used brain invasion as a criteria for upgrading an otherwise grade I meningioma before 2007, that the US and UK are truly different populations, or more likely that the effect of the histological changes may not be as great as previously thought.
There is a substantial mortality associated with meningioma surgery that is related to increasing adult age, higher grade, subtotal resection, and being male.Citation13–16 In patients with grade I tumours, 19% of people are dead at 10 years over what one would expect without the disease, and 37% of patients with grade II tumours. This is a substantial reduction in survival for a ‘benign’ condition. For patients, their quality of life after surgery is also important. Two large studies of 1722 and 291 patients showed significant reductions in physical, cognitive, emotional, and social function, and patients suffered significant fatigue and sleep impairment following meningioma surgery.Citation17,Citation18
Cranial meningiomas can be broadly divided into skull base tumours and non-skull base. The Surgical morbidity and mortality described, might at first be thought to be related to a preponderance of skull base tumours. It was not possible in this study to differentiate between skull base and non-skull base meningiomas. Skull base meningioma are less common, have a higher recurrence rate and worse progression free survival, but are more likely to be grade I, have a slower growth rate, and reports suggest a comparable net survival rate.Citation16,Citation19,Citation20
Overall survival outcomes for surgically treated patients are getting better. This improving trend, in light of greater subspecialisation within surgical practice in the UK, may be used to further support the role of the specialty tumour surgeon.Citation6
Patients with surgically treated spinal meningiomas were even more likely to be female than those treated with cranial disease (3.5:1 vs 2.3:1). Differences in hormone responsiveness and genomic makeup have been suggested to explain this difference.Citation9,Citation21 Treatment for symptomatic spinal meningiomas is surgery and gross macroscopic resection with or without dural excision, with or without radiotherapy or SRS for residual or recurrent disease, or higher grade tumours.Citation22–24 Recurrences can occur years or decades later and in a representative case series of 62 patients, subtotal resection (Simpson grade III/IV) was associated with a 30% recurrence rate at a mean of 12 years later.Citation25 There is a 98% 5 year net survival, but it appears quality of life may be affected. A series of 13,792 admissions in the US for spinal meningiomas showed that 42% were discharged to facilities other than home or self-care suggesting an early associated morbidity.Citation26
Molecular markers of meningiomas are becoming increasingly important in clinical practice. Meningiomas are most commonly associated with monosomy of chromosome 22, but are also associated with deletion of Chromosome 1p, losses of chromosomes 6q, 9p, 10, 14q, and 18q in higher-grade tumours, as well as mutations in the NF2 gene in both patients with neurofibromatosis, and sporadic, meningiomas.Citation9,Citation27–30 Most meningiomas are monoclonal tumours, and sporadic, but a few are associated with tumour predisposition syndromes including neurofibromatosis type 2, multiple endocrine neoplasia, and some DNA repair gene abnormalities.Citation31,Citation32 Progesterone receptor expression is inversely associated with meningioma grade.Citation1 DNA methylation has been used to better predict disease progression and may be important in the future for predicting outcome, and further molecular marker studies are ongoing.Citation33,Citation34 Molecular markers were not available for the meningiomas in this study. Future epidemiological studies incorporating molecular subtypes will help improve our understanding of the associated clinical significance.
The Public Health England National Cancer Registration and Analysis Service is a partnership operated by Public Health England and amongst its aims is to promote efficient and effective data collection for tumour patients and to provide a common national database for cancer datasets. It has now become mandatory for all trusts to collate data on patients with brain tumours and forward them to a national repository. This central data repository allows whole country data for England to be analyzed to gain an insight into different patient tumour groups and hopefully improve services across the country.
Limitations of the current study include the absence of complete data on meningioma site (skull base vs non-skull base), radiotherapy use and dose, SRS use, comorbidities, complications, and further surgical episodes and treatment at recurrence. A number of patients did not have meningioma grade documented, but outcomes for that group suggest they were in similar proportions to those recorded. Not all patients with incidental untreated meningiomas will be coded and included in the NCRAS database, and this is supported by the difference in incidence rates between the US and UK populations.Citation2,Citation7 The recent inclusion of radiology reports in the national data registry should help address that issue. Net survival rates assume that patients with meningiomas are similar to age and sex matched controls. Patients with meningiomas are associated with greater body adipose mass, and greater adipose mass may be associated with other comorbidities including diabetes and vascular diseases, which have implications for survival. Therefore the net figures presented may overestimate slightly the effects of a diagnosis of meningioma on survival.
Conclusions
The outcome for patients with meningioma is good, is improving, is better for women, and for younger patients and those with spinal meningiomas. Despite this, there remains a significant mortality and morbidity related to this disease.
Disclosures statement
The authors have no potential conflict of interest.
References
- Louis DN, Ohgaki H, Wiestler OD. ed. 2016. WHO classification of tumours of the centre nervous system revised. 4th ed. Lyon: IARC.
- Ostrom QT, et al. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2011–2015. Neuro Oncol 2018;20:2018.
- Rogers L, Barani I, Chamberlain M, et al. Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg 2015;122:4–23.
- Goldbrunner R, Minniti G, Preusser M, et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 2016;17:e383–e391.
- Schaffar R, Rachet B, Belot A, et al. Estimation of net survival for cancer patients: relative survival setting more robust to some assumption violations that cause specific setting, a sensitivity analysis on empirical data. Eur J Cancer 2017;72:78–83.
- Williams M, Treasure P, Greenberg D, et al. Surgeon volume and 30 day mortality for brain tumours in England. Br J Cancer 2016;115:1379–82.
- Cea-Soriano L, Wallander M-A, García Rodríguez LA, et al. Epidemiology of meningioma in the United Kingdom. Neuroepidemiology 2012;39:27–34.
- Benson VS, Pirie K, Green J, et al. Lifestyle factors and primary glioma and meningioma tumours in the Million Women Study cohort. Br J Cancer 2008;99:185–90.
- Wiemels J, Wrensch M, Claus EB, et al. Epidemiology and etiology of meningioma. J Neurooncol 2010;99:307–14.
- Kleihues P, Cavenee WK. ed. 2000. Pathology and genetics of tumours of the nervous system. Lyon: IARC.
- Louis DN, Ohgaki H, Wiestler OD. ed, 2007. WHO classification of tumours of the centre nervous system. 4th ed. Lyon: IARC.
- Pearson BE, Markert JM, Fisher WS, et al. Hitting a moving target: evolution of a treatment paradigm for atypical meningiomas amid changing diagnostic criteria. Neurosurg Focus 2008;24:E3.
- Connolly ID, Cole T, Veeravagu A, et al. Craniotomy for resection of meningioma: an age-stratified analysis of the MarketScan longitudinal database. World Neurosurg 2015;84:1864–70.
- Poon MT-C, Fung LH-K, Pu JK-S, et al. Outcome of elderly patients undergoing intracranial meningioma resection–a systematic review and meta-analysis. Br J Neurosurg 2014;28:303–9.
- Aizer AA, Bi WL, Kandola MS, et al. Extent of resection and overall survival for patients with atypical and malignant meningioma. Cancer 2015;121:4376–81.
- Savardekar AR, Patra DP, Bir S, et al. Differential tumor progression patterns in skull base versus non-skull base meningiomas: a critical analysis from a long-term follow-up study and review of literature. World Neurosurg 2018;112:e74–e83.
- Benz LS, Wrensch MR, Schildkraut JM, et al. Quality of life after surgery for intracranial meningioma. Cancer 2017;124:161–6.
- Nassiri F, et al. Life after surgical resection of a meningioma: a prospective cross-sectional study evaluating health-related quality of life. Neuro Oncol 2019;14:i32–i43.
- Ohba S, Kobayashi M, Horiguchi T, et al. Long-term surgical outcome and biological prognostic factors in patients with skull base meningiomas. J Neurosurg 2011;114:1278–87.
- Mansouri A, Klironomos G, Taslimi S, et al. Surgically resected skull base meningiomas demonstrate a divergent postoperative recurrence pattern compared with non-skull base meningiomas. J Neurosurg 2016;125:431–40.
- Sayagués JM, Tabernero MD, Maíllo A, et al. Microarray-based analysis of spinal versus intracranial meningiomas: different clinical, biological, and genetic characteristics associated with distinct patterns of gene expression. J Neuropathol Exp Neurol 2006;65:445–54.
- Klekamp J, Samii M. Surgical results for spinal meningiomas. Surg Neurol 1999;52:552–62.
- Jenkinson MD, Simpson C, Nicholas RS, et al. Outcome predictors and complications in the management of intradural spinal tumours. Eur Spine J 2006;15:203–10.
- Ravindra VM, Schmidt MH. Management of spinal meningiomas. Neurosurg Clin N Am 2016;27:195–205.
- Nakamura M, Tsuji O, Fujiyoshi K, et al. Long-term surgical outcomes of spinal meningiomas. Spine 2012;37:E617–e623.
- Ambekar S, Sharma M, Kukreja S, et al. Complications and outcomes of surgery for spinal meningioma: a Nationwide Inpatient Sample analysis from 2003 to 2010. Clin Neurol Neurosurg 2014;118:65–68.
- Lekanne Deprez RH, Bianchi AB, Groen NA, et al. Frequent NF2 gene transcript mutations in sporadic meningiomas and vestibular schwannomas. Am J Hum Genet 1994;54:1022–9.
- Zang KD. Meningioma: a cytogenetic model of a complex benign human tumor, including data on 394 karyotyped cases. Cytogenet Genome Res 2001;93:207–20.
- Jansen M, Mohapatra G, Betensky RA, et al. Gain of chromosome arm 1q in atypical meningioma correlates with shorter progression-free survival. Neuropathol Appl Neurobiol 2012;38:213–9.
- Domingues P, González-Tablas M, Otero Á, et al. Genetic/molecular alterations of meningiomas and the signaling pathways targeted. Oncotarget 2015;6:10671–88.
- Jacoby LB, Pulaski K, Rouleau GA, et al. Clonal analysis of human meningiomas and schwannomas. Cancer Res 1990;50:6783–6.
- Bethke L, Murray A, Webb E, et al. Comprehensive analysis of DNA repair gene variants and risk of meningioma. J Natl Cancer Inst 2008;100:270–6.
- Sahm F, Schrimpf D, Stichel D, et al. DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol 2017;18:682–94.
- Suppiah S, Nassiri F, Bi WL, et al. Molecular and translational advances in meningiomas. Neuro-oncol 2019;21:i4–i17.