Abstract
Objective
The primary objective of this investigation is to systematically scrutinize extant surgical studies delineating Four-Level Anterior Cervical Discectomy and Fusion (4L ACDF), with a specific emphasis on elucidating reported surgical indications, clinical and radiological outcomes, fusion rates, lordosis correction, and the spectrum of complication rates.
Methods
The literature review was conducted in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, employing the MEDLINE (PubMed), Embase, and Scopus databases. This analysis encompasses studies implementing the 4L ACDF procedure, with detailed extraction of pertinent data pertaining to surgical methodologies, types of employed interbody cages, clinical and radiological endpoints, rates of fusion, and the incidence of complications.
Results
Among the 15 studies satisfying inclusion criteria, a marginal increment in the year 2022 (21.4%) was discerned, with a preponderance of study representation emanating from China (35.7%) and the United States (28.6%). 50% of the studies were single-surgeon studies. Concerning follow-up, studies exhibited variability, with 42.9% concentrating on periods of five years or less, and an equivalent proportion extending beyond this timeframe. Across the amalgamated cohort of 2457 patients, males constituted 51.6%, manifesting a mean age range of 52.2–61.3 years. Indications for surgery included radiculopathy (26.9%) and myelopathy (46.9%), with a predilection for involvement at C3–7 (24.9%). Meta-analysis yielded an overall complication rate of 16.258% (CI 95%: 14.823%–17.772%). Dysphagia (4.563%), haematoma (1.525%), hoarseness (0.205%), C5 palsy (0.176%) were the most prevalent complications of 4L ACDF. Fusion rates ranging from 41.3% to 94% were documented.
Conclusion
The 4L ACDF is commonly performed to address mylopathy and radiculopathy. While the surgery carries a complication rate of around 16%, its effectiveness in achieving bone fusion can vary considerably.
Keywords:
Introduction
Anterior cervical diskectomy and fusion (ACDF), first described in 1958, is considered the gold standard for many degenerative diseases of the cervical spine because of its relative simplicity and minima, risk.Citation1 1- and 2-level (1L and 2L) ACDF has been shown to be a highly successful procedure associated with significant improvement in clinical outcomes and high fusion rates (FR).Citation2 In cervical spine surgery, an increase of the number of instrumented levels is directly correlated with an increase in a number of postoperative complications.Citation3 As the number of involved levels increased, surgical results become worse in terms of operative time, blood loss, NDI (neck disability index) score, cervical ROM (range of motion) and complication rates postoperatively.Citation4 Three-level (3L) ACDF has been recently reported to as an effective surgery for symptomatic degenerative cervical disc disease which can be safely performed in the outpatient setting.Citation5 The number of complications is higher in patients with three- and four level ACDF compared to 1- and 2-level surgery.Citation5
Four-level (4L) ACDF comprises about 2.4% of all ACDF surgeries performed in the USA.Citation6 Recent national database analysis on 97,081 patients who underwent ACDF in the USA has shown that four-level cases had higher odds of adverse events than one-level cases with higher reoperation and dysphagia rates.Citation6 However, other studies report that 4-level ACDF is not necessarily associated with a greater number of or more severe complications than 3-level ACDF, with comparable clinical outcomes.Citation7 An equivalent rate of fusion and time to fusion between 3L and 4L surgeries has been recently reportedCitation8 as well as between long-segment and short segment cervical fusions.Citation8
The aim of our study was to perform a thorough literature review on all surgical studies which report on a significant number of patients with four-level ACDF, to analyze indications for surgery, clinical and radiological outcome, as well as complication rate. To our knowledge, this is the first literature review on four level ACDF.
Materials and methods
Study design and registration
A review was undertaken in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines established in 2021.Citation9 The study has been registered in the Open Science Framework (OSF) database, identified by the code OSF.IO/5NUPE.
Search strategy
The search strategy, as detailed in , is designed for database searches on the topic of ‘Four-level’ and ‘Anterior cervical discectomy and fusion ACDF’ or ‘ACDF’ across three platforms: MEDLINE (PubMed), Embase, and Scopus. Detailed search query is presented in Supplementary materials 1.
Table 1. Characteristics of included studies and samples.
Eligibility criteria
The inclusion criteria for this review were defined as follows: (a) Neurosurgical series on ACDF who report on at least one patient who underwent four-level procedure from 2000 to present day are included in the literature review (b) Publications in the English language were considered for inclusion; (c) Studies had to provide primary data on clinical and radiological outcomes and complication rates related to four-level ACDF; (d) Only studies with the full text available were included, ensuring a comprehensive examination of the research; (e) studies published from 2000 to 2023.
The exclusion criteria encompassed: (a) books and book chapters; (b) conference papers; (c) reviews, meta-analyses, or case reports; (d) publications not in the English language or lacking an English translation; (e) animal studies; (f) studies available only in abstract form; (g) studies with mixed cohorts of patients undergoing both ACDF and Anterior Cervical Corpectomy and Fusion (ACCF) unless results were separately reported for each technique; (h) patients who underwent 4L ACDF using hybrid methods; (i) studies without data of interest, such as: studies including mixed cohorts of 3, 4, and 5-level ACDF without differentiation in outcomes for the 4L surgeries.
Study selection
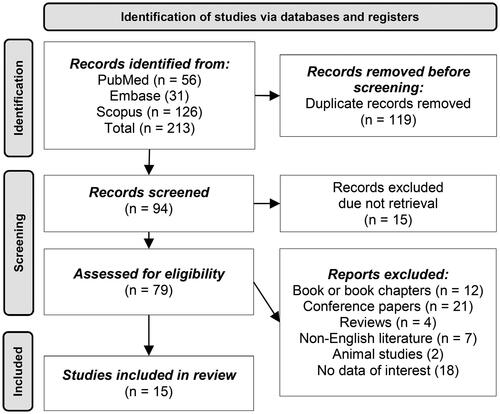
Initially, a comprehensive dataset comprising 213 records was compiled from PubMed (n = 56), Embase (n = 31), and Scopus (n = 126) (). Subsequent to this, the application of automated deduplication in Endnote X9 (Clarivate, London, United Kingdom), followed by manual deduplication, resulted in the removal of 119 duplicate records. This process yielded 103 unique records, which underwent systematic screening, leading to the exclusion of 15 records due to non-retrievability.
A comprehensive eligibility assessment was subsequently conducted on the remaining 89 records. The assessment was organized such that two independent blinded authors (AA and JM) analyzed the abstracts of the 79 studies. Discrepancies in the selection of studies were resolved through discussion and a final decision by the study supervisor (MP). This process led to the exclusion of reports falling into categories such as books (n = 12), conference papers (n = 21), reviews (n = 4), non-English literature (n = 7), animal studies (n = 2), and those lacking relevant data (n = 18). The result of this selection process identified 15 studies that met the pre-established criteria.
Data extraction and statistical analysis
Each incorporated article underwent scrutiny for bibliographic information, study design, participant demographics, patient characteristics, surgical techniques, types of utilized cages, clinical and radiological outcomes, fusion rates, and complication rates within surgical series encompassing individuals subjected to 4L ACDF.
The extracted data underwent statistical analysis using Microsoft Excel software (Microsoft Co., Redmond, Washington). The analysis included the presentation of frequencies and percentage representation for categorical variables. For the proportion of complications and weighted percentages, a fixed-effect calculation was used in the MedCalc software (MedCalc Software Ltd., Acacialaan, Ostend, Belgium), because of heterogeneity among included studies. The assessment of diagnostic accuracy in the included studies was not reported, therefore specificity, sensitivity, and the area under the curve (AUC) were not analyzed.
Risk of bias assessment
This study employed the Risk of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool, comprising seven domains, to assess potential biases in interventional observational studies.Citation24 These domains include: bias due to confounding, bias in the selection of participants into the study, bias in the classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in the measurement of outcomes, and bias in the selection of the reported result.Citation24 Two authors independently and blindly assessed the risk of bias, with disagreements resolved through discussion and consensus among all authors. Additionally, weighted assessments based on fixed-effect were conducted using the Robvis R-based application focusing on the variable of total complications.Citation25 Furthermore, the risk of publication bias was evaluated using the MedCalc software and visualized using a funnel plot.
Results
Characteristics of included studies and patients
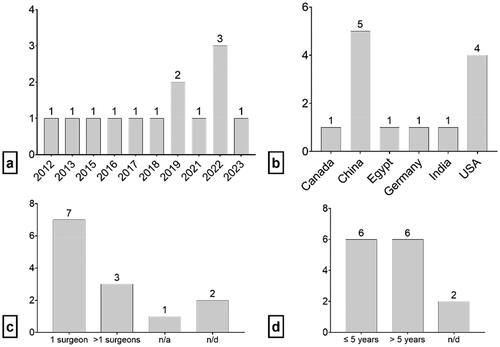
Fifteen studies met the inclusion criteria as outlined in .Citation7,Citation10–23 The temporal distribution of the included studies demonstrated a degree of consistency, with a marginal increase noted in 2022 (21.4%) (). This systematic review encompassed a diverse array of studies originating from various countries, notably with a predominant representation from China (35.7%) and the USA (28.6%) (). Half of the studies (50%) were conducted by a single surgeon, while 21.4% involved collaboration among multiple surgeons (). Additionally, the review included studies conducted over varying time spans, with 42.9% focused on periods of five years or less and an equivalent proportion extending beyond five years (). All included studies followed a retrospective methodological design.
Demographic and preoperative patients’ characteristics
The total patient cohort across the studies amounted to 2457, with 1256 (51.6%) being male, resulting in a male-to-female ratio of 1.04:1. The mean age ranged from 52.2 to 61.3 years across the studies.
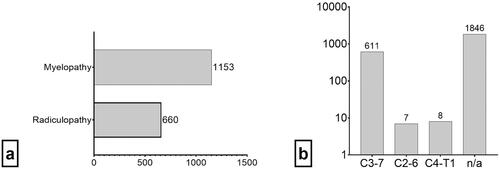
In included studies, it was reported that 660 (26.9%) patients had radiculopathy, while 1153 (46.9%) had myelopathy (). The data reveals that the majority of 4L ACDF surgeries were documented for patients with involvement at levels C3–7, constituting 611 cases (24.9%) ().
Type of cages used in 4L ACDF surgery
The types of cages used in the studies varied across studies. Wang et al.Citation12 employed standalone cages filled with hydroxyapatite-collagen artificial bone, Wang et al.Citation12 utilized PEEK cages with an anterior plate, Charalampidis et al.Citation13 utilized allografts with a titanium plate, Soliman et al.Citation14 utilized a lordotic cornerstone bone graft with a plate, Alhashash et al.Citation15 used a titanium rectangular cage filled with iliac graft, Kim et al.Citation7 used allografts with a plate, Li et al.Citation16 used interbody fusion cages with anterior dynamic cervical plates, Lin et al.Citation17 used autogenous iliac crest grafts or a titanium mesh cage and plate, Shousha et al.Citation18 used titanium rectangular cages without a plate, Li et al.Citation19 used PEEK cages and an anterior cervical plate, Chen et al.Citation21 used autogenous bone with a cervical locking plate, Kreitz et al.Citation22 used autogenous bone with an anterior cervical plate, and White et al.Citation23 used PEEK cages with structural allograft ().
Table 2. Data related to four – level anterior cervical discectomy and fusion (4L ACDF) surgery, complications, follow-up period, clinical outcome, and fusion rate.
Perioperative and postoperative complications
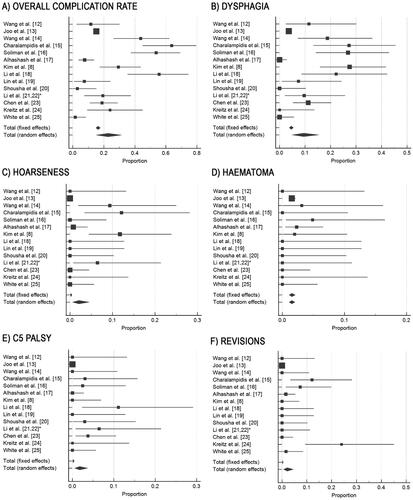
Overall complications, dysphagia, hoarseness, C5 palsy, and revisions exhibit significant heterogeneity (p < .0001), while hematoma shows no significant association (p = .8369) and minimal variability. Across the studies examined, the highest proportion of overall complications was reported by Charalampidis et al.Citation13 at 63.636%. However, the fixed effects analysis yielded an overall complication rate of 16.258%, with a narrow 95% confidence interval of 14.823% to 17.772%. Dysphagia, hoarseness, haematoma, C5 palsy, were the most prevalent complications of 4L ACDF surgery (). Dysphagia was notably reported highest by Charalampidis et al.Citation13 at 27.273%, while haematoma had the highest proportion from Soliman et al.Citation14 at 4.878%. The fixed effects analysis revealed dysphagia occurring in approximately 4.563% of patients and haematoma in about 1.525%. C5 palsy, with the highest proportion reported by Li et al.Citation16 at 11.111%, appeared relatively rare overall, with a fixed effects proportion of 0.176%. Similarly, revisions, although highest at 24.000% in the study by Kreitz et al.,Citation22 were relatively rare across studies, with a fixed effects proportion of 0.208% (Supplementary materials 2).
On cohort-based results, there were several rare complications documented in studies on four-level anterior cervical discectomy and fusion (ACDF). Joo et al.Citation11 documented sepsis (0.7%), deep venous thrombosis (0.6%), acute kidney injury (1.8%), urinary tract infection (3.8%), pneumonia (2.5%), wounds (0.6%), and respiratory deficits (9.38%). Wang et al.Citation12 reported hematoma (3.1%), respiratory deficits (9.38%), and hoarseness (9.38%). Charalampidis et al.Citation13 observed C7 nerve root injury (3.6%) and other complications (7%). Soliman et al.Citation14 noted dysphonia (7.3%), vertebral artery (VA) injury (2.4%), and superficial infection (2.4%). Alhashash et al.Citation15 documented transient paraparesis due to epidural hematoma (0.8%) and hoarseness (0.8%). Kim et al.Citation7 reported hematoma (2%). Li et al.Citation16 documented C5 palsy (3.3%), and Shousha et al.Citation18 observed C5 palsy (2.9%).
Follow-up and clinical outcomes
Wang et al.Citation12 reported the longest follow-up period, with a mean duration of 5 years. In contrast, Charalampidis et al.Citation13 and Soliman et al.Citation14 had a follow up period of 1 year.
Notable progress and improvements in clinical outcomes were observed in several investigations. Wang et al.Citation12 reported increased JOA scores from 10.1 ± 1.1 to 12.9 ± 1.2 following ACDF with a standalone cage filled with hydroxyapatite-collagen artificial bone. Wang et al.Citation12 demonstrated mid-term success with PEEK cages, showing significant improvements in VAS for neck and arm pain, NDI, and JOA scores over a 5-year follow-up period. Charalampidis et al.Citation13 observed significant clinical improvement at 12 months, with reduced NDI scores and improved VAS for neck pain. Soliman et al.Citation14 reported substantial improvements in neck and arm VAS scores at 12 months following 4L ACDF with a lordotic cornerstone bone graft and plate. Alhashash et al.Citation15 noted positive outcomes at 2 years, with significant enhancements in NDI and VAS for neck and arm pain.
Fusion rate and lordosis correction
Fusion was defined only in two studies, as the presence of trabecular bone across the interface between the cage and vertebral endplate, bony bridging formation between superior and inferior endplate and the presence of <1 mm of motion in dynamic X-rays (Alhashash et al., 2022) or as a distance less than 1 mm motion between spinous processes per fused level in flexion and extension.Citation22 Wang et al.,Citation12 Soliman et al.,Citation14 Alhashash et al.,Citation15 and Li et al.,Citation19 report fusion rates ranging from 80.77% to 94%. However, challenges and variability were evident in studies like Wang et al.,Citation10 Charalampidis et al.,Citation13 Kreitz et al.,Citation22 and White et al.,Citation23 where complications such as pseudoarthrosis, cage subsidence suggesting potential difficulties in achieving consistent fusion outcomes in some cases.
Quality and risk of bias assessment
Weighted fixed-effect assessment of the risk of bias indicates that the overall risk of bias is moderately prevalent. One study exhibited a critical level of bias, while another demonstrated a serious risk. Seven studies showed a low risk, whereas five studies indicated a moderate risk. Bias concerning the presentation of results is notable. Regarding publication bias, Egger’s test (p = .2081) and Begg’s test (p = .2259) did not reveal statistically significant deviations. Details regarding the assessment of the risk of bias are presented in Supplementary materials 3.
Discussion
The systematic review encompassed a total of 15 studies, with the majority being reported in China, followed by the United States. Regarding China, a notable increase in research interest in spinal surgery in this country was evident, as reported by Li et al.,Citation26 aligning with the findings of this study. All included studies employed a retrospective design. A major number of the studies reported a single surgeon performing 4L ACDF. Additionally, there were several studies that incorporated mixed cohorts involving both 3L and 4L ACDF procedures.Citation5–8,Citation27–30 Studies encompassed 2457 patients undergoing 4L ACDF, with no significant fluctuations observed in gender distribution. Statistically significant differences in age and gender characteristics were not noted in the study by Patel et al.Citation31 involving 1L and 2L ACDF, as well as in the study by Wang et al.Citation32 involving 3L ACDF.
Baseline characteristics of the patients with 4L ACDF
The mean age of patients who underwent four-level ACDF ranges from 55 to 65 years. The role of age and its influence on outcome following multilevel ACDF is not a subject of thorough analysis. In a recent multi-center retrospective evaluation in Michigan,Citation33 age is not found to be an independent risk factor for complications in patients that underwent ACDF. Independent preoperative ambulation is especially protective for major complications. However, this review of 9,135 patients with 2,266 complications did demonstrate that the elderly has a significantly higher rate of complications (31.5 vs 24%).Citation33 This study contains only 48 patients (24 with and 24 without complications) with four-level ACDF, so these results cannot be the sole basis of interpretation.Citation33 In a meta-analysis of 2868 patients with cervical spondylotic myelopathy, there was definitely a higher potential risk while operating on the elderly population, but no significant difference in the incidence of postoperative complications was noted.Citation34 Due to the cumulative risk of advanced age >70 years and the increase of complications with an increase of fused segments, four-level ACDF needs thorough surveillance postoperatively and should not be performed as an outpatient surgery in this specific group. Gender is not recognized as a risk factor for four-level ACDF. BMI is reported in several studies on four-level ACDF. Patients with a higher BMI, larger neck circumference, and shorter neck length may have longer operation duration, more blood loss, and more postoperative complications and have been thus identified as high-risk patients for three- and four-level ACDF.Citation35 Although diabetes has been discussed as a potential risk factor in patients undergoing ACDF,Citation36 none of the studies report on this matter. The greater the age, the longer the duration of symptoms and the more severe symptoms at presentation, the more adverse outcomes can be expected after surgery for CSM.Citation37
Indications for 4L ACDF surgery
Indications for surgery and surgical techniques have not been extensively detailed in the included studies. While variations existed in the reporting of radiculopathy and myeloradiculopathy symptoms in most studies, a common indication for 4L ACDF appears to be a multifocal spinal cord compression condition with either observable myelopathy changes on MRI or overlapping radiculopathy syndromes that cannot be distinctly correlated to a single level due to multisegmented compression evident on MRI.Citation38 The criteria for surgery encompassed absolute spinal canal stenosis, neuroforamen stenosis, or radiological indications of myelopathy.Citation39–41 Clinical manifestations of radiculopathy were observed in one or more levels, while radiologically, absolute spinal canal stenosis and/or neuroforamen stenosis extending across all four levels were identified.Citation15 In several studies, cervical spondylotic myelopathy emerged as the primary indication for surgery.Citation10,Citation42
Surgical approach and technique
The conventional Smith-Robinson ventrolateral, or anterior approach to the cervical spine,Citation43 was uniformly employed in the studies. Variations were noted in the surgical technique, specifically in the preparation of the endplates and the selection of the cage. The incorporation of additional posterior surgery was inconsistently reported. Shousha et al.Citation18 conducted additional posterior fixation in 9 out of 25 patients undergoing 4L ACDF. While this approach resulted in improved radiological outcomes, indicated by higher FRs compared to the non-fixation group, the observed difference did not attain statistical significance.
Anterior reconstruction of the cervical spine encompasses not only ACDF but also anterior cervical corpectomy and fusion (ACCF). Lin et al.Citation44 conducted a comparative analysis involving 120 patients, evaluating 3 and 4L ACDF alongside 4L ACCF. Their findings revealed no significant differences in terms of clinical symptom improvements between the two procedures. However, ACDF exhibited superior postoperative Neck Disability Index (NDI) scores, as well as advantages in terms of blood loss, lordotic curvature improvement, and lower rates of instrumentation and graft-related complications, with the exception of operation times. Li et al.Citation19,Citation20 conducted a comprehensive comparison within their two studies, examining 4L ACDF against 4L ACCF, as well as 4L ACDF with cage only versus 4L ACDF with a plate, utilizing the same cohort of 31 patients. The results indicated that 4L ACDF outperformed corpectomy in terms of maintaining cervical lordosis, achieving a higher FR, and exhibiting a lower incidence of dysphagia.
In addition to comparing various techniques for cervical spine reconstruction, two studies have undertaken a comparison between anterior multisegmental surgery and posterior multisegmental decompression and fusion in patients with spinal canal stenosis and cervical spondylotic myelopathy.Citation10,Citation21 These studies have revealed comparable clinical outcomes and complication rates between the two approaches. The ACDF group, in a study conducted by Chen et al.,Citation21 exhibited a higher loss of lordosis correction and pseudoarthrosis, with a similar degree of long-term neurological improvement. Notably, 4L ACDF, due to its lower blood loss compared to posterior surgery, along with comparable surgery time and complication rates, has been suggested as a more suitable option for elderly patients.Citation21 Additionally, hybrid techniques for anterior cervical spine reconstruction have been documented.Citation41 Ashkenazi et al.Citation45 reported on 12 patients who underwent 1L corpectomy and 3L discectomies, as well as 13 patients with 2L corpectomy and 4L adjacent diskectomy. These hybrid techniques have not gained widespread acceptance in clinical practice for anterior cervical spine reconstruction.
Mullins et al.Citation5 conducted an analysis of complication risks associated with outpatient and inpatient groups undergoing 3L or 4L ACDF surgery. They found that while individuals undergoing 3L or 4L surgery had an elevated risk of complications compared to those undergoing 1 or 2L surgery, the disparity between the two groups was minimal. This suggests that multilevel surgeries can be performed safely in an outpatient setting.
Operative timing and blood loss
The recorded duration of operative procedures exhibits variability, ranging from 139.3 minutes in the investigation conducted by Li et al.Citation20 to an average of 196 ± 46 minutes, as reported by Alshashash et al..Citation15 Wang et al.Citation12 demonstrated an operative time of 121 ± 24 minutes. Rajan et al.Citation46 concluded in their study that the length of the operative procedure may influence the occurrence of complications associated with anterior cervical diskectomy and fusion (ACDF). A significant difference is observed when comparing the duration of 4L ACDF to 1L ACDF in Rajan et al.,Citation46 with 104.33 ± 54.89 minutes for 1L ACDF, highlighting the increased complexity of 4L ACDF surgery. The study by Chang et al.Citation47 reported an operative time of 109.0 ± 104.14 minutes for 3L ACDF, with a high standard deviation indicating variability in the procedure duration.
The reported blood loss during these procedures was documented with an average of 500 ± 380 mL in the study by Alshashash et al..Citation15 Additionally, Wang et al.Citation12 reported a blood loss of 230 ± 93 mL. Intraoperative blood loss for 3-level ACDF in the study by Chang et al. was 238.5 ± 55.80 mL, while for 2-level ACDF, this value in the study by Cai et al.Citation48 was 102.70 ± 46.78 mL.
Type of the cage and plate-related considerations
Various types of cages utilized in 4L ACDF procedures may impact clinical outcomes and FRs, as evidenced by studies such as those conducted by Wang et al.,Citation12 Joo et al.,Citation11 and Soliman et al.Citation14 These investigations demonstrate the effectiveness of stand-alone cages, PEEK cages with plates, and lordotic cornerstone bone grafts with plates in treating cervical spondylotic myelopathy. Notwithstanding varying complications, including dysphagia and pseudoarthrosis, these studies collectively underscore the importance of carefully selecting the appropriate cage based on individual patient characteristics and surgical objectives.Citation49,Citation50 ACDF emerges as a consistently safe and effective approach for addressing cervical spine pathologies, emphasizing the critical role of cage choice in optimizing surgical success.
Most of the studies have used a ventral plate following 4L ACDF. Several exceptions are to be found in the literature,Citation12,Citation15,Citation18 but these groups have reported comparable clinical and radiological outcomes to studies where the plate was used. FR of 80.77% was reported in a series of 130 patients who underwent surgery with a standalone cage filled with iliac crest graft bone.Citation15 Shousha et al. report 87.5% fusion in their series of 25 patients who underwent 4 level ACDF with titanium mesh without a plate, with only one perioperative complication.Citation18
Clinical outcome
Studies on ACDF have consistently demonstrated improvements in clinical outcomes. Wang et al.,Citation10 Joo et al.,Citation11 Wang et al.,Citation12 Charalampidis et al.,Citation10 Soliman et al.,Citation14 Alhashash et al.,Citation15 Kim et al.,Citation7 Li et al.,Citation10 Shousha et al.,Citation18 Li et al.,Citation20 and White et al.Citation23 all reported positive outcomes, showcasing enhancements in various measures such as JOA scores, VAS for pain, NDI, and neurological improvement. Lin et al.Citation17 found no significant difference between four-level ACDF and posterior laminectomy, while Chen et al.Citation21 reported successful ACDF outcomes but with some cases of dysphagia. Despite a 31% radiographic nonunion rate, Kreitz et al.Citation22 reported consistent neurological improvement. Overall, the majority of studies support the efficacy of ACDF in achieving positive clinical results.
Radiological outcomes – fusion, adjacent segment disease, subsidence, and correction of cervical lordosis
Radiological outcomes encompass reports on fusion, occasionally noting changes in C2-C7 Cobb angle and an increase in cervical spine lordosis. However, the reporting of cage subsidence has been inconsistent. The substantial variation in the literature regarding fusion rates, pseudarthrosis, and subsidence following 4L ACDF may stem from diverse criteria employed for radiological assessment. Fusion definitions range from bridging bone between vertebral bodies to the absence of >1-mm motion on dynamic X-rays.Citation15 Fusion rates vary widely, reported from 41.3%Citation23 to 100%.Citation21 Stand-alone anterior cervical arthrodesis with allograft in 3L and 4L ACDF has shown a notable incidence of pseudarthrosis, particularly at the caudal level of the construct, with higher rates in patients undergoing 4L to 3L ACDF. Symptomatic pseudoarthrosis is typically treated with posterior fixation, with reported incidences of up to 11%. Fusion across levels is infrequently reported, with McClure et al.Citation8 presenting data on the achievement of fusion at different cervical levels in 3L and 4L ACDF patients. Multilevel ACDF has been demonstrated to significantly increase and maintain both segmental and global cervical lordosis up to 6 months post-surgery, with a positive correlation between the augmentation of C2-C7 global lordosis and the sagittal vertical axis. Katsuura et al.Citation29 observed a significant increase in cervical lordosis from preoperative 10.26°–4 weeks postoperative at 19.44°, sustained up to 6 months in a mixed cohort of patients with 3L and 4L ACDF.
Fusion across levels is reported only in one study by McClure et al. 88% and 82% of three- and four-level patients achieved fusion at C3–4, respectively; 85% of three-level and 89% of four-level patients achieved fusion at C4–5; 68% of three-level and 89% of four-level patients achieved fusion at C5–6; 44% of 3L and 42% of 4L patients achieved fusion at C6–7; and no patients achieved fusion at C7–T1.Citation8 The pseudarthrosis rate after multi-segment anterior cervical fusion has shown to have a direct correlation to the number of levels surgically fused.Citation51 Furthermore, failed arthrodesis and the need of posterior instrumentation can be reduced using osteobiological adjuvants.Citation51 A literature review on 893 patients reports superior surgical outcomes in ACDF procedures with anterior plate fixation (increased fusion, decreased subsidence) and slightly better VAS-neck pain scores at the last follow-up.Citation52 Due to the heterogeneity of the data and those different types of grafts were used among the same cohorts, a comparison of the type of graft to subsidence, hardware failure, and fusion is not able to be performed. In a literature review on 2363 patients who underwent ACDF with, a comparison of the long-term patient-reported and the radiographic outcomes associated with the use of titanium and PEEK, intervertebral body cages showed similar finding.Citation53
A prospective, randomized clinical trial in which patients undergoing one to three-level ACDF with increased postoperative segmental lordosis or maintained postoperative segmental sagittal alignment recorded significantly better patient-reported outcomes.Citation54 Multilevel ACDF has been shown to significantly increase and maintain both segmental and global cervical lordosis up to 6 months after surgery,Citation29 whereas increasing C2–C7 global lordosis is correlated with increasing positive sagittal vertical axis. In a mixed cohort of patients with three- and four-level ACDF, Katsuura et al. report that cervical lordosis significantly increased from pre-operatively 10.26°–4 weeks post-operatively 19.44° and is maintained up to 6 months at 19.34°.Citation29
The significance of cervical lordosis correction is emphasized in an analysis of 84 patients by Song et al.Citation55 A mild-to-moderate correction of cervical lordosis has been shown to be superior to complete correction in patients with kyphosis who undergo four-level ACDF because this approach is associated with lower axial stress and CSVA correction loss.Citation55 The rate of adjacent segment disease in this study is also high: mild correction group − 6 (21.43%), moderate − 9 (37.50%) and complete − 19 (59.38%).Citation23 The prevalence of the adjacent segment disease following cervical spine surgery has been shown to be up to 40%.Citation55 Since a high number of studies do not report on radiological outcome in detail, adjacent segment disease could be present more often than reported in the literature. The rate of adjacent segment disease has not yet been discussed between single-, two-, and multilevel ACDF, although evidence shows that the adjacent level disc height decreases and the incidence of adjacent segment disease increases with an increasing number of operative levels at 24 months of follow-up.Citation8 Adjacent-segment disease has been described in 27% of patients who underwent four-level ACDF in a series of 45 patients, all of which were asymptomatic.Citation56 The rate of adjacent segment degeneration is higher in patients with shorter fusions. Adjacent segment degeneration is less frequent among patients in whom C5–6 and C6–7 are fused than among those in whom C5–6 or C6–7 is left at an adjacent level, irrespective of the length of the fusion.Citation56
Perioperative and postoperative complications
The data from the studies included on perioperative and postoperative complications following 4L ACDF surgeries highlights a range of issues. Dysphagia emerges as the most frequently observed complication. Regardless of the number of levels affected by ACDF surgery, Tsalimas et al.Citation57 report that 19.4% of patients undergoing this procedure develop dysphagia. Haller et al.Citation58 report an overall dysphagia rate of 3.8%. However, there is considerable variation in reporting dysphagia as a complication, ranging from as high as 52%Citation59 to as low as 2.1%.Citation60 Our study’s calculation supports an average dysphagia rate of 5.33%. In addition to dysphagia, a variety of complications are reported, including sepsis, deep vein thrombosis, acute kidney injury, urinary tract infections, pneumonia, wounds, hematomas, hoarseness, respiratory deficit, cerebrospinal fluid leakage, C5 palsy, nerve root and vertebral artery injuries, dysphonia, and superficial infection. These complications are reported in similar proportions in other studies involving 1L, 2L, and 3L levels.Citation61
Reoperation rates at five years for four-level ACDF were 22.1%, compared to 13.0%, 13.5%, and 15.0% for 1L, 2L, and 3L cases.Citation11 The same group of authors compared 4L ACDF to 4L posterior cervical fusion. Posterior approach procedures were associated with approximately double the odds of any, serious, and minor adverse events, but around one third the rate of dysphagia and two thirds the rate of five-year reoperations.Citation11 This analysis of 1857 matched patients from both groups showed that the five-year reoperation rate was 26.3% for 4 level ACDF and 18.3% for posterior fusion at five years follow up.Citation11 Thus, it can be concluded that the complication rate for 4L ACDF is comparable to that of 1L, 2L, and 3L procedures.
Three vs. four level ACDF
De la Garza-Ramos et al. demonstrate that patients who underwent four-level ACDF have significantly higher rates of dysphagia, postoperative neck pain, and postoperative narcotic usage when compared with patients who underwent three-level ACDF. Pseudarthrosis and deep wound infection rates are also higher in the four-level group, although this did not reach statistical significance.Citation62 However, four-level ACDF is not always associated with a greater number of or more severe complications than three-level ACDF, but rather has comparable clinical outcomes.Citation7,Citation27 An equivalent rate of fusion and time to fusion between three- and four-level surgeries has been reported as well as between long-segment and short segment cervical fusions.Citation8 Comparable patient-reported clinical and radiological outcome has been reported in a retrospective study of Canseco et al.Citation27 There are no differences in analyses of complications and readmission rates between inpatient and outpatient surgery in the 3441 patients who underwent three- and four-level ACDF; nevertheless, outpatient surgery is more likely to be performed for three- than for four-level ACDF.Citation63
Inpatient versus outpatient setting
In 2011, only 7.0% of multi-level ACDF were performed outpatient, in contrast to 32.9% in 2018.Citation63 In this literature review, only three studies report on outpatient surgeries for four-level ACDF. Outpatient multilevel ACDF is performed in younger and healthier patients, with three-level being more common than four-level procedures.Citation63 Evidence increasingly suggests that four-level ACDF is a safe procedure to perform in the outpatient setting. The largest single-surgeon retrospective study analyzes the inpatient and outpatient setting, which includes patients who underwent 4-level ACDF.Citation5 Although outpatient and inpatient groups undergoing three- or four-level surgery have an increased risk of complications (compared with those undergoing one- or two-level surgery), there is a negligible difference between the two groups, suggesting that multilevel surgeries can also be safely performed in an outpatient setting.Citation5 A recent analysis of 337 procedures in patients with three- and four-level ACDF (102 outpatient and 11 inpatient four-level procedures), although without differentiation between three- and four-level surgery, has shown that this procedure is safe to perform in outpatient setting in select patients.Citation64 Perioperative complications, such as delirium and surgical site infections, correlate to the readmission rate, which was higher in outpatients.Citation64 In one further analysis of three- and four-level ACDF in 3,441 patients, there was no significant difference in the total complication rates (4.49% vs 2.49%) or unplanned readmissions (4.96% vs 3.72%) between inpatient and outpatient cohorts.Citation63
Limitations of the study and future directions for research
While the study diligently adhered to PRISMA guidelines and employed a comprehensive methodology, there are certain limitations to acknowledge. The search scope was confined to three databases, which may have excluded pertinent literature from other sources. Additionally, the relatively small number of included studies reflects the uncommon nature of 4L ACDF surgeries, which require specific expertise and resources. Another limitation stems from the heterogeneity in study design and postoperative monitoring approaches, posing challenges in data comparability across studies. Moving forward, it is recommended that future analyses of 4L ACDF incorporate standardized guidelines and follow consistent parameters. This approach will facilitate the possibility of conducting a meta-analysis, enhancing the ability to draw comprehensive and comparative conclusions across studies.
Conclusion
In essence, this systematic review of 15 studies, primarily retrospective and involving single-surgeon procedures, identified cervical spondylotic myelopathy as a prevalent indication. Despite variations in surgical techniques and cage choices, favorable clinical and radiological outcomes consistently affirmed the effectiveness of ACDF. Complications, particularly dysphagia, were on par with lower-level procedures. Reoperation rates at five years for 4L ACDF were higher than those for lower-level procedures but akin to 4L posterior cervical fusion. Evidence also supports that 4L ACDF is safe to perform in outpatient settings. Prospective studies with complete analysis of clinical and radiological outcomes and long-term follow up are needed for future assessment. The results of this systematic review suggests future analyses should adopt standardized guidelines for meta-analyses and underscores the pivotal role of meticulous cage selection for surgical success.
Supplemental Material
Download Zip (273 KB)Disclosure statement
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Funding
References
- Fowler SB, Anthony-Phillips P, Mehta D, et al. Health-related quality of life in patients undergoing anterior cervical discectomy fusion. J Neurosci Nurs 2005;37:97–100.
- Fraser JF, Härtl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. SPI 2007;6:298–303.
- Koller H, Hempfing A, Ferraris L, et al. 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J 2007;16:2055–71.
- Yu S, Li F, Yan N, et al. Anterior fusion technique for multilevel cervical spondylotic myelopathy: a retrospective analysis of surgical outcome of patients with different number of levels fused. PLOS One 2014;9:e91329.
- Mullins J, Pojskić M, Boop FA, et al. Retrospective single-surgeon study of 1123 consecutive cases of anterior cervical discectomy and fusion: a comparison of clinical outcome parameters, complication rates, and costs between outpatient and inpatient surgery groups, with a literature review. J Neurosurg Spine 2018;28:630–41.
- Joo PY, Zhu JR, Kammien AJ, et al. Clinical outcomes following one-, two-, three-, and four-level anterior cervical discectomy and fusion: a national database study. Spine J 2022;22:542–8. 04
- Kim S, Alan N, Sansosti A, et al. Complications after 3- and 4-level anterior cervical diskectomy and fusion. World Neurosurg 2019;130:e1105–e1110.
- McClure JJ, Desai BD, Shabo LM, et al. A single-center retrospective analysis of 3- or 4-level anterior cervical discectomy and fusion: surgical outcomes in 66 patients. J Neurosurg Spine 2020;34:45–51.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71.
- Wang B, Lü G, Kuang L. Anterior cervical discectomy and fusion with stand-alone anchored cages versus posterior laminectomy and fusion for four-level cervical spondylotic myelopathy: a retrospective study with 2-year follow-up. BMC Musculoskelet Disord 2018;19:216.
- Joo PY, Jayaram RH, McLaughlin WM, et al. Four-level anterior versus posterior cervical fusions: Perioperative outcomes and five-year reoperation rates: outcomes after four-level anterior versus posterior cervical procedures. N Am Spine Soc J 2022;10:100115.
- Wang SJ, Ma B, Huang YF, et al. Four-level anterior cervical discectomy and fusion for cervical spondylotic myelopathy. J Orthop Surg 2016;24:338–43. 24
- Charalampidis A, Hejrati N, Ramakonar H, et al. Clinical outcomes and revision rates following four-level anterior cervical discectomy and fusion. Sci Rep 2022;12:5339.
- R Soliman MA, Alkhamees AF, Khan A, et al. Instrumented four-level anterior cervical discectomy and fusion: long-term clinical and radiographic outcomes. Neurol India 2021;69:937–43.
- Alhashash M, Allouch H, Boehm H, et al. Results of four-level anterior cervical discectomy and fusion using stand-alone interbody titanium cages. Asian Spine J 2022;16:82–91.
- Li F, Li Z, Huang X, et al. Comparison of two reconstructive techniques in the surgical management of four-level cervical spondylotic myelopathy. Biomed Res Int 2015;2015:513906.
- Lin D, Zhai W, Lian K, et al. Anterior versus posterior approach for four-level cervical spondylotic myelopathy. Orthopedics 2013;36:e1431–e1436.
- Shousha M, Ezzati A, Boehm H. Four-level anterior cervical discectomies and cage-augmented fusion with and without fixation. Eur Spine J 2012;21:2512–9.
- Li Z, Wang H, Tang J, et al. Comparison of three reconstructive techniques in the surgical management of patients with four-level cervical spondylotic myelopathy. Spine 2017;42:E575–E583.
- Li Z, Huang J, Zhang Z, et al. A comparison of multilevel anterior cervical discectomy and corpectomy in patients with 4-level cervical spondylotic myelopathy: a minimum 2-year follow-up study: multilevel anterior cervical discectomy. Clin Spine Surg 2017;30:E540–E546.
- Chen Q, Qin M, Chen F, et al. Comparison of outcomes between anterior cervical decompression and fusion and posterior laminoplasty in the treatment of 4-level cervical spondylotic myelopathy. World Neurosurg 2019;125:e341–e347. 05
- Kreitz TM, Hollern DA, Padegimas EM, et al. Clinical outcomes after four-level anterior cervical discectomy and fusion. Global Spine J 2018;8:776–83.
- White MD, Farber SH, Pacult MA, et al. Pseudarthrosis after four-level anterior cervical discectomy and fusion without posterior fixation. Neurosurg FocusFocus. 2023;55:E4.
- Jonathan ACS, Miguel AH, Barnaby CR, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919.
- McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 2020;12:55–61.
- Li Y, Zheng S, Wu Y, et al. Trends of surgical treatment for spinal degenerative disease in China: a cohort of 37,897 inpatients from 2003 to 2016. Clin Interv Aging 2019;14:361–6. 2019/02/15
- Canseco JA, Minetos PD, Karamian BA, et al. Comparison between three- and four-level anterior cervical discectomy and fusion: patient-reported and radiographic outcomes. World Neurosurg 2021;151:e507–e516.
- Feng YT, Hwang SL, Lin CL, et al. Safety and resource utilization of anterior cervical discectomy and fusion. Kaohsiung J Med Sci 2012;28:495–9.
- Katsuura Y, Lemons A, Lorenz E, et al. Radiographic analysis of cervical and spinal alignment in multilevel ACDF with lordotic interbody device. Int J Spine Surg 2017;11:13.
- Wewel JT, Kasliwal MK, Adogwa O, et al. Fusion rate following three- and four-level ACDF using allograft and segmental instrumentation: A radiographic study. J Clin Neurosci 2019;62:142–6.
- Patel MR, Jacob KC, Parsons AW, et al. Impact of gender on postsurgical outcomes in patients undergoing anterior cervical discectomy and fusion. Int J Spine Surg 2022;16:991–1000.
- Wang W, Huang Y, Wu Z, et al. Comparison of 3-level anterior cervical discectomy and fusion and open-door laminoplasty in cervical sagittal balance: a retrospective study. Front Surg 2022;9:937479.
- Lawless MH, Tong D, Claus CF, et al. Age as a risk factor for complications following anterior cervical discectomy and fusion: analysis from the Michigan spine surgery improvement collaborative (MSSIC). Spine 2021;47:343–51.
- Madhavan K, Chieng LO, Foong H, et al. Surgical outcomes of elderly patients with cervical spondylotic myelopathy: a meta-analysis of studies reporting on 2868 patients. Neurosurg Focus 2016;40:E13.
- Qi M, Xu C, Cao P, et al. Does obesity affect outcomes of multilevel ACDF as a treatment for multilevel cervical spondylosis?: a retrospective study. Clin Spine Surg 2020;33:E460–E465.
- Sharif S, Afsar A. Diabetes: is it the troublemaker in anterior cervical discectomy and fusion? World Neurosurg 2017;103:914–6.
- Zileli M, Maheshwari S, Kale SS, et al. Outcome measures and variables affecting prognosis of cervical spondylotic myelopathy: WFNS spine committee recommendations. Neurospine 2019;16:435–47.
- Matz PG, Holly LT, Groff MW, et al. Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine 2009;11:174–82.
- Zou S, Gao J, Xu B, et al. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta-analysis of randomized controlled trials. Eur Spine J 2017;26:985–97.
- McGirt MJ, Rossi V, Peters D, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting: analysis of 2000 consecutive cases. Neurosurgery 2020;86:E310–E315.
- Begagić E, Pugonja R, Bečulić H, et al. The new era of spinal surgery: exploring the use of exoscopes as a viable alternative to operative microscopes–A systematic review and meta-analysis. World Neurosurg 2023;182:144–58.e1.
- Houten JK, Weinstein GR, Collins M. Long-term fate of C3-7 arthrodesis: 4-level ACDF versus cervical laminectomy and fusion. J Neurosurg Sci 2021;65:402–7.
- Eghbal K, Ahrari I, Kamrani F, et al. Multilevel anterior cervical fusion with standalone cage or cage-and-plate after cervical discectomy: benefits and drawbacks. Asian J Surg 2023;46:3760–5.
- Lin Q, Zhou X, Wang X, et al. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J 2012;21:474–81.
- Ashkenazi E, Smorgick Y, Rand N, et al. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine 2005;3:205–9.
- Rajan PV, Emara AK, Ng M, et al. Longer operative time associated with prolonged length of stay, non-home discharge and transfusion requirement after anterior cervical discectomy and fusion: an analysis of 24,593 cases. Spine J 2021;21:1718–28. 2021/10/01/
- Chang H-K, Huang W-C, Tu T-H, et al. Radiological and clinical outcomes of 3-level cervical disc arthroplasty. J Neurosurg 2020;32:174–81.
- Chang HK, Huang WC, Tu TH, et al. Radiological and clinical outcomes of 3-level cervical disc arthroplasty. J Neurosurg Spine 2019;32:174–81.
- Lonjon N, Favreul E, Huppert J, et al. Clinical and radiological outcomes of a cervical cage with integrated fixation. Medicine 2019;98:e14097.
- Yoo M, Kim WH, Hyun SJ, et al. Comparison between two different cervical interbody fusion cages in one level stand-alone ACDF: carbon fiber composite frame cage versus polyetheretherketone cage. Korean J Spine 2014;11:127–35.
- Khoueir P, Oh BC, DiRisio DJ, et al. Multilevel anterior cervical fusion using a collagen-hydroxyapatite matrix with iliac crest bone marrow aspirate: an 18-month follow-up study. Neurosurgery 2007;61:963–71.
- Oliver JD, Goncalves S, Kerezoudis P, et al. Comparison of outcomes for anterior cervical discectomy and fusion with and without anterior plate fixation: a systematic review and meta-analysis. Spine 2018;43:E413–E422.
- Onyedimma C, Jallow O, Yolcu YU, et al. Comparison of outcomes between cage materials used for patients undergoing anterior cervical discectomy and fusion with standalone cages: a systematic review and meta-analysis. World Neurosurg 2021;158:e38–e54.
- Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 2011;68:1309–16.
- Song QX, Su XJ, Wang K, et al. Is complete correction of cervical sagittal malalignment necessary during 4-level anterior cervical discectomy and fusion surgery in patients with kyphosis? Global Spine J 2021;13:1311–8.
- Komura S, Miyamoto K, Hosoe H, et al. Lower incidence of adjacent segment degeneration after anterior cervical fusion found with those fusing C5-6 and C6-7 than those leaving C5-6 or C6-7 as an adjacent level. J Spinal Disord Tech 2012;25:23–9.
- Tsalimas G, Evangelopoulos DS, Benetos IS, et al. Dysphagia as a postoperative complication of anterior cervical discectomy and fusion. Cureus 2022;14:e26888.
- Haller L, Mehul Kharidia K, Bertelsen C, et al. Post-operative dysphagia in anterior cervical discectomy and fusion. Ann Otol Rhinol Laryngol 2022;131:289–94.
- Mendoza-Lattes S, Clifford K, Bartelt R, et al. Dysphagia following anterior cervical arthrodesis is associated with continuous, strong retraction of the esophagus. J Bone Joint Surg Am 2008;90:256–63.
- Lied B, Rønning PA, Halvorsen CM, et al. Outpatient anterior cervical discectomy and fusion for cervical disk disease: a prospective consecutive series of 96 patients. Acta Neurol Scand 2013;127:31–7.
- Yee TJ, Swong K, Park P. Complications of anterior cervical spine surgery: a systematic review of the literature. J Spine Surg 2020;6:302–22.
- De la Garza-Ramos R, Xu R, Ramhmdani S, et al. Long-term clinical outcomes following 3- and 4-level anterior cervical discectomy and fusion. J Neurosurg Spine 2016;24:885–91.
- Boddapati V, Mathew J, Lee NJ, et al. Are outpatient three- and four-level anterior cervical discectomies and fusion safe? Spine J 2021;21:231–8.
- Khalid SI, Kelly R, Carlton A, et al. Outpatient and inpatient readmission rates of 3- and 4-level anterior cervical discectomy and fusion surgeries. J Neurosurg Spine 2019;31:70–5.