Abstract
Objectives
The COVID-19 pandemic required a change in resource priority from Neurosurgical care in order to treat medically unwell patients suffering from the complications of COVID-19 infections. We demonstrate the impact of COVID-19 on total bed days in 24 Neurosurgical centres in England offering adult Neurosurgery as well as the total spells (single inpatient episodes) for operative Neurosurgical patients between 2020 and 2022 when compared with 2019.
Methods
We used Capse Healthcare Knowledge System software iCompare in order to show the change in total spells for patients undergoing a primary or secondary Neurosurgical procedure as defined using the National Neurosurgical Audit Programme (NNAP) OPCS-4 coding framework between 2019 and 2022.
Results
The overall mortality rate of COVID-19 patients was 12.3% and the percentage of total bed days taken up by COVID-19 patients in hospitals at large was on average 7.7%. The total number of spells for all procedures over the 24 centres in 2022 was 39,019 compared with 45,742 in 2019. There was a cumulative deficit of 24,904 spells. The loss of spells was not equally distributed across regions and hospital Trusts. The average number of referral to treatment pathways completed within 18 weeks has declined from 76% to 57% over the study period and the referral to treatment clearance time has risen from 17 to 24 weeks.
Conclusions
The mean elective cranial output in 2022 compared with 2019 is at 88% with spinal output lagging at 69%. If the rate of change year on year were to remain at current levels then we would reach pre-pandemic levels of output by 2026.
Keywords:
Introduction
The COVID-19 pandemic necessitated a significant reduction of elective surgical services in the National Health Service (NHS) in order to safeguard emergency care and treat an unprecedented influx of acutely unwell patients with respiratory illness.Citation1 It has been previously described that the volume of all elective surgical procedures in England and Wales dropped by 51.8% in 2020.Citation1 We know that the initial impact of the COVID-19 virus was variable in different regions of England and therefore Neurosurgical services were variably affected.Citation2
Decisions had to be made across the NHS regarding which patients to prioritise. This necessarily led to a downturn in elective surgical work and the surgical work that was prioritised was often oncological work or other more ‘semi-elective’ cases.Citation3 We also know that the COVID-19 infection itself prevented some elective surgery going ahead as planned due to increased risk to the patient.Citation4–6 The surgical backlog incurred by the pandemic is not evenly distributed throughout subspecialties and spinal surgery, for example, experienced a far more precipitous downturn compared with cranial work.Citation7 However, the exact variation between subspecialties as well as centres has not previously been explored in Neurosurgery.
Efforts have been made since the COVID-19 pandemic to jumpstart activity and begin to reverse the trend of the ever-lengthening waiting lists.Citation8 There is also evidence of a ‘hidden waiting list’ created by the COVID-19 pandemic that includes many patients who are not captured statistically due to stasis in the system and issues with access to healthcare that have been compounded.Citation9 This means that any data on the growth of waiting lists, for example, most likely underestimate the problem. There is a growing appreciation that returning to pre-pandemic levels of activity has not been straightforward. Despite a number of initiatives elective neurosurgical activity has not returned to its pre COVID levels.Citation10,Citation11
Here we report the results of a retrospective analysis of the prospectively collected total spells for primary and secondary procedures over 24 Neurosurgical centres in England using spells as a proxy for surgical activity. We describe how activity has changed since the index year of 2019 for both cranial and spinal work as well as looking at the differences between elective and emergency output. We also estimate when levels may reach pre-pandemic norms and the possible extent of the deficit by this point.
Methods
Study design
This was a population based epidemiological study describing all spells including either a primary or secondary Neurosurgical procedure at any of the 24 adult Neurosurgical centres in England between the 1st January 2020 to the 31st December 2022 inclusive. A spell in Hospital Episode Statistic data is described as an uninterrupted inpatient stay at one hospital.Citation12 We used data from the 1st January 2019–31st December 2019 by way of a pre-pandemic comparator year. A method that has been previously described by the COVIDSurg Collaborative.Citation13
Data sources
All data utilised in this study was compiled using the CHKS Limited iCompare© systemCitation14 as well as Model Hospital. CHKS's iCompare© is an audit and benchmarking tool that allows for comparison of a bespoke peer group over a range of metrics. CHKS iCompare© uses data provided by patients and collected by the NHS as part of their care and support. Where HES data is used, it is with permission of NHS England.Citation12
Study population
Neurosurgical centres used in this study were defined as those offering adult Neurosurgical services in England. However, all patients of any age admitted during the time period who underwent either a primary or secondary Neurosurgical procedure were included in the study. Neurosurgical procedures were defined using the National Neurosurgical Audit Programme (NNAP) coding framework as previously described.Citation15 We divided Neurosurgical procedures into either cranial, spinal or other procedure.
Outcomes
The primary outcome was the number of hospital spells with an associated Neurosurgical procedure.
Data processing
Filters were utilised on the iCompare platform with respect to Neurosurgical centres, the specialty code ‘150’ to define a Neurosurgical admission and the OPCS-4 codes as previously described in order to ensure only operative admissions and not admissions for investigations or conservative management were included. With respect to the data analysing the impact of the first and second waves of COVID-19 we used pragmatic dates spanning peaks of infection rates as defined by the Office for National Statistics as no exact dates for these waves have been defined.Citation16 These were a first wave from 1st March to the 31st April 2020 and a second wave from 1st September 2020–28th February 2021. For the purposes of pre-pandemic comparison years we have used the most recent previous year to define ‘normal’ activity. 95% confidence intervals were also calculated based on Poisson process.
Microsoft Excel for Mac Version 16.72 used for collection and analysis of data as well as STATA/MP version 18.0.
Results
Impact of the COVID-19 pandemic investigated using mortality rates and total bed days
We used the mortality rate from COVID-19 as well as the percentage of bed days taken up by COVID-19 patients as a heuristic for how bad the impact of the COVID-19 pandemic was at each centre. The overall mortality rate of COVID-19 patients was 12.3% (SD 2.55) with a minimum of 7.9% and a maximum of 17.3%. The percentage of total bed days taken up by COVID-19 patients was on average 7.7% (SD 2.16) with a minimum of 0.7% and a maximum of 10.9%.
We compared both of these against the percentage change in elective surgical output from each institution in 2022 compared with 2019 but there was no correlation found with either metric as demonstrated in supplementary figure 1.
Comparison with pre-COVID annual activity
shows the number of total elective spells between 2019 and 2022 using the NNAP OPCS-4 coding framework to define operative cases. Comparison made between total elective cases in 2020 and 2022 against 2019 levels as well as showing the number of cranial elective procedures performed as a percentage of the total in 2019 and 2022.
Table 1. Total elective Neurosurgical operative spells 2019–2022.
shows the number of total emergency spells between 2019 and 2022 using the NNAP OPCS-4 coding framework to define operative cases. Comparison made between total emergency cases in 2020 and 2022 against 2019 levels as well as showing the number of cranial emergency procedures performed as a percentage of the total in 2019 and 2022.
Table 2. Total emergency Neurosurgical operative spells 2019–2022.
and show the number of total spells with either a primary or secondary procedure and the Neurosurgery specialty code 150. They show an initial decline in overall elective work between 2019 and 2020 of 30% with a decrease in emergency activity of 6%. This has recovered year upon year, however, the percentage change in cranial elective surgery in 2022 compared with 2019 remains −12% with spinal surgery significantly lower at −31% of where it was in 2019. also demonstrates a shift towards cranial elective work with it making up on average 55% of the elective work in 2019 whilst it makes up 61% of the total spells in 2022. This pattern is not replicated in where cranial work is 75% of the total work in both 2019 and 2022. Supplementary tables 1 and 2 break this data down by individual trust.
Each Trust has recovered at a different rate as shown in . The mean elective cranial output in 2022 compared with 2019 is at 88% with spinal output lagging at 69%. 6 Trusts are above the output of 2019 for elective cranial surgery and only 2 Trusts have increased their elective spinal output by 2022. The change in overall activity for each trust is mapped as a timeline in .
Figure 1. Bar chart comparing the percentage output of cranial and spinal work in the 24 Neurosurgical centres of 2022 with 2019.
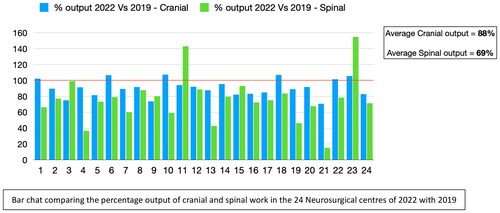
Figure 2. (A, B) Timelines comparing the changes in total spells for emergency and elective activity before, during and after the Pandemic across all 24 Trusts.
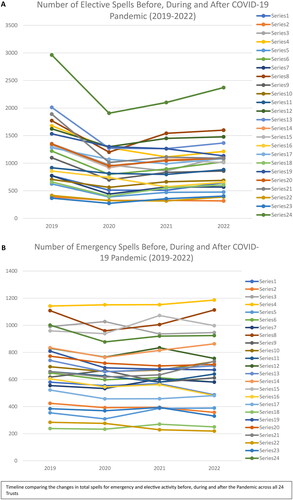
Emergency surgery is down by 4% in 2022 when compared with 2019. Supplementary figure 2 demonstrates that following the initial downturn in activity in the first year of COVID, emergency activity has remained relatively stable compared with elective work and the ‘deficit’ when comparing 2019 to the three subsequent years is only 2381 spells.
Deficit of surgical activity
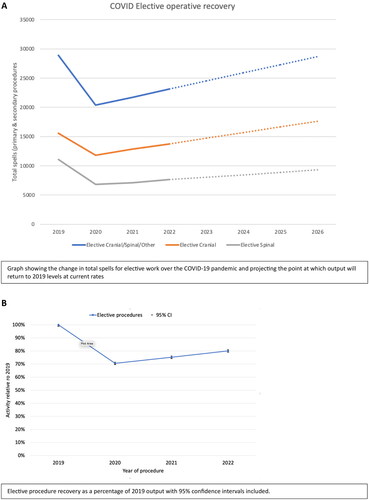
The current deficit of total spells for all elective surgery between 2019 and 2022 is 22,523. This breaks down as 8,263 cranial spells and 11,654 spinal spells. shows a graphical representation of growth at the current rate and projects that pre-Pandemic levels of overall activity will be reached by 2026. However, levels of elective spinal output will still not have reached pre-Pandemic levels by this point. The potential deficit of total spells by 2026 would be 33,480 patients at the current rate of recovery. then shows the percentage of elective service recovery when compared with 2019 with 95% confidence interval also demonstrated. The level of elective activity in 2022 is currently 80% of what it was in 2019 having been as low as 70% in 2020.
Figure 3. (A). Graph showing the change in total spells for elective work over the COVID-19 pandemic and projecting the point at which output will return to 2019 levels at current rates. (B). Elective procedure recovery as a percentage of 2019 output with 95% confidence intervals included.
Supplementary table 3 shows the numbers of orthopaedic spine elective procedures performed at the Neurosciences centres over the study period. The average output of those centres that have Orthopaedic spinal services was 83% in 2022 compared with 2019 with a surgical deficit over the study period of 5423 spells. 7 centres have no Orthopaedic Spinal service and 3 centres had multiple years without any Orthopaedic spinal surgeries being performed.
Impact of COVID-19 pandemic on neurosurgical outpatient waiting lists
Supplementary figure 3 utilises Model Hospital and CHKS data to show that overt the study period the amount of time patients are waiting for treatment has grown significantly. Supplementary figure 3(A) shows a decline of referral to treatment within 18 weeks from 76% to 57%. The Referral to Treatment (RTT) operational standard is that more than 92% of patients should have been treated within 18 weeks. As well as this the RTT clearance time has increased from 17 weeks to 24 weeks. A clearance time of over 12 weeks is described as making the operational standard for RTT impossible to deliver.
Discussion
Significant disruption to elective work has continued to affect Neurosurgical services following a return to ‘normality’ post COVID-19.Citation17 The key finding of this study is objective evidence of a long ‘tail’ in reduced neurosurgical activity following the COVID-19 pandemic. We find that levels of activity in the last normal year before the pandemic have not been reached in most trusts in England offering adult Neurosurgery in either cranial or spinal surgery. We have found that cranial surgery has recovered at a faster rate and this may be due to cranial pathologies being prioritised as ‘semi-elective’ and being less likely to be cancelled as services attempt to return to normal. We also note that spinal emergency work did not suffer as great a downturn as cranial emergency work and therefore we speculate that there were spinal patients who crossed over to emergency work as a result of long waits and evolving pathologies.Citation18
We demonstrate a significant variation between different Trusts in terms of the rate of recovery when comparing total spells with levels in 2019. It is beyond the scope of this study to comment on the precise reasons for this disparity. However, looking at purely the crude impact of the COVID-19 pandemic in terms of mortality rates of patients with COVID-19 and % of hospital bed days taken up with COVID-19 patients there appears to be no correlation between the extent of the impact and the elective recovery by 2022. We used these particular metrics as demonstrable ones for how severe the pandemic was for different hospitals since we know this was felt variably throughout the UK. Our hypothesis was that hospitals where the metrics suggest a more severe COVID-19 pandemic would have redistributed services in a way that would have had a greater impact upon Neurosurgical elective services. However, we cannot find evidence to support this supposition. There are likely to be local factors that have affected a return to normal levels of activity. Some Trusts have coped better than would be expected and other Trusts that have coped less well.
When looking at the seven trusts that have either cranial or spinal output of greater than 100% when compared with 2019 there is no distinct pattern in terms of how they were affected by the COVID-19 pandemic. Standalone Neurosurgical units, which are those units without an Emergency Department, might have been predicted to have been less affected by the downturn in activity following COVID, however, we find that none of these Trusts have returned to 2019 levels in either spinal or cranial work. The size of the unit also did not appear to have a bearing upon the extent of the recovery. It is imperative that we elucidate the reasons for the variability in recovery as this has potential ramifications for service orientation in the NHS going forwards. Further work will be needed in order to better define what makes certain Trusts more resilient than others. Ongoing work such as the COVID-19 Related Service Adjustment In Referral practice (CORSAIR) will also give us an understanding of how the changes that have affected Neurosurgical services have translated into the management of Neurosurgical emergencies. It is important to have both quantitative and qualitative impressions of the impact of COVID-19 on British Neurosurgery.
This study is the first study to objectively quantify the scale of the surgical resource deficit in Neurosurgical centres in England. This study shows that the downturn in activity was ubiquitous and that spinal surgery has struggled to recover to a greater extent than cranial surgery. We show how emergency surgery was protected during the pandemic by the sacrifice of elective work, as the rates remained relatively stable. We recognise that the recovery does not obviously correlate with crude metrics on the severity of the COVID-19 pandemic. Further work will be needed to be done by NNAP to better understand the reasons for the variability and translate this into shared learning for the specialty.
There are limitations to the current study. Total spells with either a Neurosurgical primary or secondary procedure and the Neurosurgical specialty code 150 is not the same as an operative count. We have used this as an efficient proxy for surgical activity, however, exact operative numbers cannot be derived from the CHKS database.Citation14 We also used 2019 as the pre-COVID index year for comparison and therefore the use of only a single year of pre-Pandemic activity relies on the data of a single, albeit most recent, year of activity. This data did not include operations that took place in the independent sector and it is well recognised that there have been efforts at waiting list initiatives in the private sector in order to make inroads into the backlog.Citation17 Especially with respect to spinal surgery this may well be why some hospitals have particularly low rates of spinal spells when compared with 2019. Orthopaedic spinal surgery performed within the same centres has also shown a downturn in output and therefore does not support the idea that some Neurosurgical spinal work is now being taken on by orthopaedic surgeons. Given the significant deficit we believe rates of operating within Trusts should be at or above pre-pandemic levels and therefore that the publication of these results is of significant interest. Further work is needed to corroborate whether this reduction is confounded by work being shifted to nearby independent providers.
Conclusion
This study is the first to attempt to quantify the deficit in Neurosurgical activity as a result of the COVID-19 pandemic for adult Neurosurgical centres in England. The volume of elective surgical activity dropped by 30% in the year 2020 and since this point has steadily risen to being at 80% of 2019 levels. This means a deficit of elective spells of 22,523 up to the end of 2022. The mean elective cranial output in 2022 compared with 2019 is at 88% with spinal output lagging at 69%. Whilst spinal surgery, particularly high volume degenerative spinal surgery, is considered as lower clinical priority, it nevertheless has an impact on patient’s quality of life and ability to return to work.Citation19 Further work is needed to understand why there was been significant variability across the country with respect to the extent of the recovery so far and to share best practice COVID recovery strategies.
Authors contributions
Daniel Thompson – Instrumental to design of study, data collection, analysis and write-up. Adam Williams – Design, manuscript review. Peter Whitfield – Manuscript preparation. Peter Hutchinson – Manuscript preparation. Nicholas Phillips – Manuscript preparation. David Cromwell – Manuscript preparation. Adel Helmy – Design, analysis, manuscript review.
Supplemental Material
Download Zip (193.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Dobbs TD, Gibson JAG, Fowler AJ, et al. Surgical activity in England and Wales during the COVID-19 pandemic: a nationwide observational cohort study. Br J Anaesth 2021;127:196–204.
- Bottle A, Faitna P, Brett S, Aylin P. Factors associated with, and variations in, COVID-19 hospital death rates in England’s first two waves: observational study. BMJ Open 2022;12:e060251.
- Kasivisvanathan R, Tilney HS, Jhanji S, et al. The 'hub and spoke model’ for the management of surgical patients during the COVID-19 pandemic. Int J Health Plann Manage 2021;36:1397–406.
- Fountain DM, Piper RJ, Poon MTC, et al. CovidNeuroOnc: a UK multicenter, prospective cohort study of the impact of the COVID-19 pandemic on the neuro-oncology service. Neurooncol Adv 2021;3:vdab014.
- El-Boghdadly K, Cook TM, Goodacre T, et al. SARS-CoV-2 infection, COVID-19 and timing of elective surgery. Anaesthesia 2021;76:940–6.
- COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020;396:27–38.
- Wordie SJ, Tsirikos AI. The impact of the COVID-19 pandemic on spinal surgery. Orthop Trauma 2021;35:314–20.
- Clifford RE, Rajput K, Naing CY, MacDonald K, Pantak T, Kaul A. Reducing waiting lists for laparoscopic cholecystectomy: an intensive approach to aid COVID-19 recovery. Eur Surg 2022;54:113–6.
- Nepogodiev D, Acharya R, et al. Forecasting waiting lists for elective procedures and surgery in England: a modelling study. medRxiv 2022.06.20.22276651.
- Carr A, Smith JA, Camaradou J, Prieto-Alhambra D. Growing backlog of planned surgery due to covid-19. BMJ 2021;372:n339.
- https://www.england.nhs.uk/coronavirus/delivering-plan-for-tackling-the-covid-19-backlog-of-elective-care/
- Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P. Data resource profile: hospital episode statistics admitted patient care (HES APC). Int J Epidemiol 2017; 46:1093–1093i.
- COVIDSurg Collaborative. Projecting COVID-19 disruption to elective surgery. The Lancet 2022;399:233–4.
- https://live.chks.co.uk/portal
- https://www.sbns.org.uk/index.php/audit/nnap-reports-and-publications/
- https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionssurveytechnicalarticle/wavesandlagsofcovid19inenglandjune2021”/l”:∼:text=The%20estimated%20dates%20for%20the,2020%20to%2024%20April%202021
- https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/waiting-times-non-urgent-treatment
- Naskar R, Baryeh KW, Pavuluri S, Rajagopal T. The changing pattern of acute spinal referrals during primary and secondary waves of the COVID-19 pandemic. Musculoskeletal Care 2022;20:316–20.
- https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/labourproductivity/articles/sicknessabsenceinthelabourmarket/2022

