ABSTRACT
Objective: To investigate outpatient follow-up after mild traumatic brain injury (mTBI) by various medical specialists, for both hospitalized and non-hospitalized patients, and to study guideline adherence regarding hospital admission. Methods: Patients (n = 1151) with mTBI recruited from the emergency department received questionnaires 2 weeks (n = 879), 3 months (n = 780) and 6 months (n = 668) after injury comprising outpatient follow-up by various health care providers, and outcome defined by the Glasgow Outcome Scale Extended (GOS-E) after 6 months. Results: Hospitalized patients (60%) were older (46.6 ± 19.9 vs. 40.6 ± 18.5 years), more severely injured (GCS <15, 50% vs. 13%) with more Computed Tomography (CT) abnormalities on admission (21% vs. 2%) compared to non-hospitalized patients (p < 0.01) . Almost half of the patients visited a neurologist at the outpatient clinic within six months (60% of the hospitalized and 25% of the non-hospitalized patients (χ2 = 67.10, p < 0.01)), and approximately ten per cent consulted a psychiatrist/psychologist. Outcome was unfavourable (GOS-E <7) in 34% of hospitalized and 21% of non-hospitalized patients (χ2 = 11.89, p < 0.01). Conclusion: Two-thirds of all mTBI patients consult one or more specialists within six months after injury, with 30% having an unfavourable outcome. A quarter of non-hospitalized patients was seen at the outpatient neurology clinic, underling the importance of regular follow-up of mTBI patients irrespective of hospital admittance.
Introduction
Traumatic brain injury (TBI) is one of the most common acute neurological disorders. In Europe, approximately 100–300 per 100,000 inhabitants are admitted to the emergency department (ED) annually, and the amount of TBI-related hospital visits is increasing [Citation1,Citation2]. The associated direct health care costs for these hospital visits are estimated around €10 billion [Citation3]. The majority of TBIs (75–90%) are classified as mild TBI (mTBI) [Citation1], and although most patients with mTBI recover within weeks to months without residual impairments, persistent complaints and delayed return to work occur in 15–20% of all cases [Citation4,Citation5]. However, it is unclear how frequently mTBI patients return to the outpatient clinic for follow-up in case of persistent complaints.
Most studies on outcome after mTBI do not differentiate between hospitalized and non-hospitalized patients, while there are clear differences between the groups. First, hospitalized patients are more severely injured [Citation6], and second, since guidelines recommend different aftercare following mTBI after hospitalization or direct discharge, it is probable that different follow-up pathways exist. The decision whether a mTBI patient has to be admitted to the hospital ward (or Intensive Care Unit) has been studied in various mTBI cohorts, which has led to European guidelines for ED treatment, admission and follow-up for this patient category [Citation6,Citation7]. Outpatient follow-up in the sub-acute phase after injury is recommended at least once for hospitalized patients. Conversely, for non-hospitalized patients specialized follow-up is only indicated when patients have persisting complaints interfering with daily activities. Although follow-up is indicated in the case of delayed recovery, it is not specified who is the most appropriate specialist to refer to and within which time frame after injury.
The aim of this study was to examine outpatient follow-up by various health care providers in a prospective cohort of patients with mild traumatic brain injury (mTBI), up to 6 months after injury. Since hospital admission is closely related to follow-up, this was also investigated as part of this study. Given the assumed differences between hospitalized and non-hospitalized patients, we believe that it is relevant to determine care consumption and outcome separately for these subgroups of mTBI, to assess the clinical practice of aftercare for patients with mTBI.
Methods
Participants
This study was part of a prospective multicentre cohort study on mTBI (UPFRONT-study). Patients were recruited from 2013 to 2015 at the ED of three participating trauma centres in the Netherlands: University Medical Center Groningen (UMCG), Medical Spectrum Twente, and St. Elizabeth Hospital. All patients classified as mTBI according to the European Federation of Neurological Societies (EFNS) guidelines (i.e. GCS 13-15, PTA <24 hours and/or LOC <30 minutes) were eligible for inclusion [Citation7]. Patient and injury characteristics were obtained from medical records. Patients admitted to the hospital ward were defined as hospitalized, patients discharged directly from the ED were defined as non-hospitalized. The EFNS guideline for head injury treatment at the ED was applied in all participating centres. It comprises recommendations for treatment, discharge and follow-up, and describes criteria for hospital admittance. These criteria were used to evaluate the clinical practice of admission and follow-up in the UPFRONT-cohort.
CT-scans performed at the ED were classified according to the Marshall criteria [Citation8], scores were dichotomized into normal CT (score 1) and abnormal CT-scan (score 2–6). Abnormal scans included only trauma-related findings such as intracranial haemorrhage, contusions and oedema. Injury Severity Scores (ISSs) [Citation9] were calculated based on hospital records, to assess physical injuries.
Exclusion criteria were age under 16 years, substance abuse, language barrier and inability for follow-up. The study protocol was approved by the ethical committee of the UMCG. Informed consent was obtained from all participants, for patients with age 16–18 years, a parent/guardian also completed the informed consent form.
Measures
Participants of the UPFRONT-study were asked to complete questionnaires two weeks, three months and six months after injury regarding outpatient clinic visits and specific questionnaires for complaints and mood. The questions on outpatient clinic visits were aimed specifically to obtain information on aftercare or follow-up related to the trauma.
Head Injury Symptom Checklist (HISC) [Citation10,Citation11]. The HISC assesses posttraumatic complaints (PTCs) and is modified from the Rivermead Postconcussion Questionnaire [Citation12]. The checklist addresses 21 PTCs such as headache, dizziness, forgetfulness and fatigue on a 3-point Likert scale, comparing complaints before and after injury.
Hospital Anxiety and Depression Scale (HADS) [Citation13]. Symptoms of anxiety and depression were measured by means of the HADS. This questionnaire consists of two subscales with seven questions each (score 1–4). Sum scores vary from 1 to 28, with the cut-off for anxiety and depression set as 8 or higher.
Glasgow Outcome Scale Extended (GOS-E) [Citation14]. Outcome was determined six months after injury with the GOS-E. The GOS-E consists of an 8-point scale, ranging from death (score 1) to complete recovery (score 8). Favourable outcome is defined by a GOS-E score 7–8, unfavourable outcome by a score of <7.
Statistical analyses
The data were analysed using SPSS 22.0. Baseline characteristics were compared between hospitalized and non-hospitalized patients using parametric (Student t-test) and non-parametric (χ2-test, Mann–Whitney U test) testing when appropriate. Guideline adherence was measured based on patient and injury characteristics. Follow-up visits at the outpatient clinic and outcome were described for the entire cohort and compared between hospitalized and non-hospitalized patients.
Results
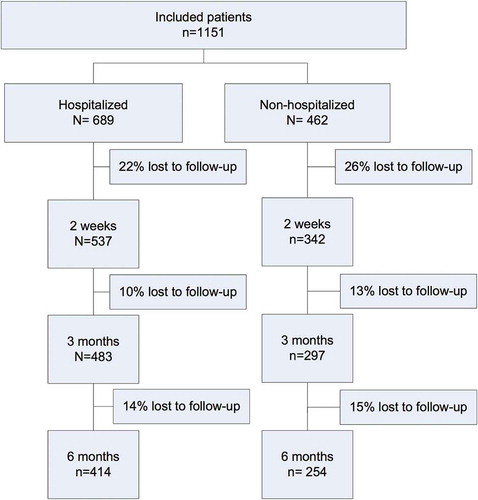
In total, 1151 patients were included in the UPFRONT-study. Sixty per cent of all patients were admitted to the hospital, mostly for one day (48%), with mean length of stay (LOS) of 3.4 days (±5.7). illustrates the distribution of participants among hospital admittance and discharge, and the number of complete information on pathways of care at different follow-up moments. Patients who did not complete the first questionnaire were significantly younger (37.5 vs. 46.2 years, p < 0.005) than patients who completed the first questionnaire, other patient characteristics did not differ significantly. The mean age of the overall cohort was 44 years (±19.6), most patients were male, and mainly injured by a traffic accident or fall. All baseline, injury and clinical characteristics are provided in .
Table I. Patient characteristics.
Posttraumatic complaints
Two weeks after injury, patients had on average five PTCs, with no significant difference between hospitalized and non-hospitalized patients. The five most common complaints were: fatigue, headache, dizziness, increased need for sleep and poor concentration. Of all patients, 16% scored above the cut-off value for depression, with no differences between hospitalized and non-hospitalized patients. In the non-hospitalized group a significantly higher percentage of patients scored above the cut-off for anxiety, compared to hospitalized patients (23% vs. 16%, p = 0.016).
Six months after injury, 46% of non-hospitalized patients reported more than one PTC, compared to 61% of the hospitalized patients (p < 0.001).
Outpatient follow-up
Almost all (98%) patients were discharged home either directly from the ED or hospital ward. A minority was discharged to a rehabilitation centre. presents outpatient follow-up visits for both hospitalized and non-hospitalized patients. Approximately half of the patients visited a neurologist in the first six months after injury (60% of hospitalized and 25% of non-hospitalized patients, χ2 = 67.1, p < 0.001). Seven per cent of the non-hospitalized and 12% of the hospitalized patients visited a psychiatrist or psychologist within six months after their injury.
Figure 2. Outpatient follow-up visits by different health care providers for hospitalized (A) and non-hospitalized (B) patients.
provides cumulative percentages of consulted specialists at each time interval. Most hospitalized patients were seen by one or several specialists within three months after injury, while more than half of the non-hospitalized patients did not consult a specialist. Six months after injury, 67% of the entire group had consulted at least one specialist (80% of hospitalized and 45% of non-hospitalized patients), with an average of five PTCs.
Outcome
Six months after injury, the majority of patients showed complete (GOS-E 8, 56%) or almost complete (GOS-E 7, 14%) recovery. Moderate disability (GOS-E 5–6) occurred in 22%, and severe disability (GOS-E <5) in 8% of cases. There were no significant within-group differences with regard to the ISS. Outcome of non-hospitalized patients was significantly more often favourable than of hospitalized patients (79% vs. 66%, χ2 = 11.89, p < 0.001).
Hospitalized vs. non-hospitalized patients
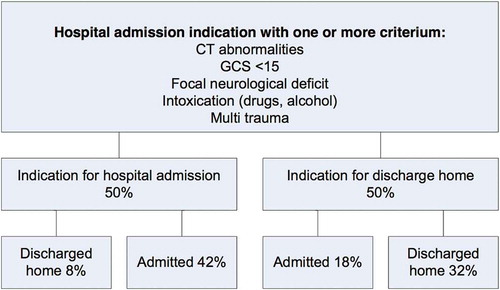
illustrates guideline adherence for hospital admittance, fifty per cent of patients met the criteria for hospital admission, the actual amount of admitted patients was 60%. Discharged patients who should have been admitted (n = 94, 8%) were relatively young (35.6 ± 15.6 years), more often male (72%) and more often intoxicated with alcohol (50%). The category of admitted patients who were not indicated for admission (n = 207, 18%) were older (49.3 ± 20.0 year), with mean LOS of 2.7 days (±6.4), 54% stayed for only one day.
Discussion
In this study we assessed outpatient follow-up after mTBI, separately for hospitalized and non-hospitalized patients. We found that two-thirds of all patients were seen at least once at an outpatient clinic, mostly by neurologists. For non-hospitalized patients, the follow-up rate at neurologists’ of 25% in the first six months and unfavourable outcome in one in five of patients were unexpected findings that highlight the importance of follow-up for all mTBI patients regardless of whether patients are admitted to the hospital.
We measured follow-up by different health care specialists up to six months after injury and demonstrated that two-thirds of all patients in our cohort were seen at least once at the outpatient clinic, mostly by neurologists. A considerable part of both the hospitalized and non-hospitalized patients were seen by surgeons and physical therapists, indicating that physical injuries might require attention up to six months after injury. The mean ISS was comparable with findings of the TRACK-TBI study, demonstrating that physical problems and related treatments are part of the heterogeneous mTBI spectrum [Citation15]. Most outpatient contacts declined over time, however, those with psychiatrists/psychologists showed a consult rate of approximately 10% after six months, a figure which was also observed in a recent study among moderate and severe TBI patients [Citation16]. Although the reason for consultation (e.g. due to psychological problems or complaints of cognitive nature) was outside the scope of this study, this finding indicates that psychological problems are long-lasting, and occur in patients with varying TBI severities. This implicates that not the injury itself but also pre-injury characteristics might be involved in the development of these problems [Citation17,Citation18].
More than half of the hospitalized patients consulted one or more specialist within six months after injury, probably due to problems on various levels of functioning (e.g. cognitive and physical). This is further supported by a reported average of five PTCs within different domains. Former studies have indicated that moderate and severe TBI patients often deal with various problems, and that rehabilitation physicians are important care providers in long-term aftercare for these patients [Citation16,Citation19]. We observed a relatively low follow-up rate with rehabilitation physicians. However, since persistent complaints and long-term vocational reintegration are a problem for a substantial part of the mTBI population [Citation20,Citation21], rehabilitation physicians might become more involved in a later phase, outside the time frame of the current study. Although guidelines specify that all patients who are admitted to the hospital should be seen at least once at the outpatient clinic, only 60% had visited a neurologist in the first six months after injury. An explanation for the fact that a large part was not seen for follow-up is that patients with a good recovery are expected not to feel the need for follow-up [Citation22].
Surprisingly, in the non-hospitalized cohort, 25% of all patients consulted a neurologist in the first six months after injury. This finding questions the clinical practice that only patients who are admitted to the ward should be seen for outpatient follow-up. Two weeks post-injury a comparable amount of PTCs were present in the two investigated groups. Yet, non-hospitalized patients were more often anxious, which might be related to uncertainty regarding the persistence of complaints [Citation23]. The non-hospitalized patients, who are expected to make a full recovery and are not scheduled for regular follow-up, might feel a lack in opportunity to ask additional questions on expected recovery, despite the fact that an information leaflet was provided on discharge from the ED [Citation10,Citation15]. Whether intensified follow-up could help dealing with this uncertainty towards recovery is largely uninvestigated. Two recent papers reported on the effect of an information intervention aimed at high-risk patients (≥three complaints 10 days after injury), in which the authors conclude that the intervention had no effect on activity or participation nor on PTC level after three months [Citation24,Citation25]. Since we found no differences in the average number of complaints between our two groups after two weeks, it might be argued that the identification of at-risk patients based on number of complaints is not appropriate for assessing the need for outpatient follow-up. Other factors such as anxiety might be more accurate in the identification for specialized aftercare, but more research is needed in this area [Citation26].
In our cohort, 30% of patients had an unfavourable outcome six months after injury, which is comparable to earlier findings. [Citation15] A recent study suggested that the relatively worse outcome for patients with mTBI, when compared to moderate TBI, is explained by sickness awareness [Citation27]; patients with mTBI are more aware of cognitive and behavioural disabilities and are therefore less satisfied with their outcome in comparison to more severely injured patients, who might be less aware of their problems. These mechanisms could also explain the unfavourable outcome in one in five of non-hospitalized patients; the awareness of their disabilities in combination with expectation of full recovery, which causes dissatisfaction with current levels of functioning.
The implication of the high rate of outpatient follow-up might be that aftercare should be scheduled for all patients irrespective of hospital admission. Although guidelines describe clear indications for hospital admission [Citation7], we found that hospital admission is not always guideline-based but varies according to clinical practice. Given the fact that mTBI guidelines for follow-up are solely based on hospital admission, and a substantial amount of non-hospitalized patients has an unfavourable outcome, a suggestion might be to alter the guidelines for follow-up, to ensure proper aftercare for all patients. Whether this aftercare should take place with follow-up at the outpatient clinic, within multidisciplinary teams or if phone counselling is sufficient, should be studied more extensively.
Limitations
Similar to most longitudinal mTBI studies, the generalizability of our findings are limited by selection bias and drop-out of patients. Research has shown that patients with good outcome are often lost to follow-up, which in our case could have led to an overestimation of outpatient visits and a bias towards worse outcome [Citation28,Citation29]. Another factor that questions the generalizability of our study is patient recruitment at the ED, while a part of the mTBI population does not consult any physician or only a general practitioner [Citation30,Citation31]. The burden of mTBI on society might be higher than estimated in the current and previous studies, if a part of this non-ED-visiting population also develops problems.
This study aimed at determining the aftercare of patients with mTBI, assessing follow-up by health care providers in different domains of care. However, we did not examine the reasons for outpatient follow-up, apart from it being trauma-related. We demonstrated that six months after injury many mTBI patients are still in the care system, with PTCs within several domains. Future studies should point us in the direction as to whether different specialists are dealing with different problems, which might lead to more clear guidelines for scheduled follow-up and referral.
Conclusions
n conclusion, the current study identified that 30% of all mTBI patients has an unfavourable outcome, and outpatient clinic visits are common. Even one in four of the non-hospitalized patients was seen by a neurologist in the first six months after injury and approximately ten per cent of all patients needed psychological care. Specialized follow-up related to problems in the physical domain comprised another substantial part of follow-up for both hospitalized and non-hospitalized patients, even up to six months after injury. For clinical practice, current guidelines should also take into account non-hospitalized patients to ensure early identification of all at-risk mTBI patients who are in need of follow-up to prevent development of complaints and unfavourable outcome.
Declaration of interest
This study was funded by the Dutch Brain Foundation (Grant no. PS2012-06).The authors report no declaration of interest.
Suppliers
IBM SPSS Statistics, SPSS Inc, Chicago, IL
References
- Cassidy JD, Carroll LJ, Peloso PM, Borg J, von Holst H, Holm L, Kraus J, Coronado VG. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(43 Suppl):28–60.
- Zonfrillo MR, Kim KH, Arbogast KB. Emergency department visits and head computed tomography utilization for concussion patients from 2006 to 2011. Acad Emerg Med. 2015;22:872–7.
- Olesen J, Gustavsson A, Svensson M, Wittchen HU, Jönsson B. The economic cost of brain disorders in Europe. Eur J Neurol. 2012;19:155–62.
- Ruff R. Two decades of advances in understanding of mild traumatic brain injury. J Head Trauma Rehabil. 2005;20:5–18.
- Laborey M, Masson F, Ribéreau-Gayon R, Zongo D, Salmi LR, Lagarde E. Specificity of postconcussion symptoms at 3 months after mild traumatic brain injury: results from a comparative cohort study. J Head Trauma Rehabil. 2014;29:E28–36.
- Vos PE, Alekseenko Y, Battistin L, Ehler E, Gerstenbrand F, Muresanu DF, Potapov A, Stepan CA, Traubner P, Vecsei L, von Wild K. Mild traumatic brain injury. Eur J Neurol. 2012;19:191–8.
- Vos PE, Battistin L, Birbamer G, Gerstenbrand F, Potapov A, Prevec T, Stepan CA, Traubner P, Twijnstra A, Vecsei L, van Wild K. EFNS guideline on mild traumatic brain injury: Report of an EFNS task force. Eur J Neurol. 2002;9:207–19.
- Marshall LF, Marshall SB, Klauber MR, Van Berkum Clark M, Eisenberg H, Jane JA, Luerssen TG, Marmarou A, Foulkes MA. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma. 1992;9 Suppl 1:S287–92.
- Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
- van der Naalt J, van Zomeren a H, Sluiter WJ, Minderhoud JM. One year outcome in mild to moderate head injury: the predictive value of acute injury characteristics related to complaints and return to work. J Neurol Neurosurg Psychiatry. 1999;66:207–13.
- Van Der Horn HJ, Spikman JM, Jacobs B, Van Der Naalt J. Postconcussive complaints, anxiety, and depression related to vocational outcome in minor to severe traumatic brain injury. Arch Phys Med Rehabil. 2013;94:867–74.
- King NS, Crawford S, Wenden FJ, Moss NE, Wade DT. The Rivermead Post Concussion Symptoms Questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995;242:587–92.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
- Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15:573–85. doi:10.1089/neu.1998.15.573.
- Lingsma HF, Yue JK, Maas AIR, Steyerberg EW, Manley GT, TRACK-TBI Investigators. Outcome prediction after mild and complicated mild traumatic brain injury: external validation of existing models and identification of new predictors using the TRACK-TBI pilot study. J Neurotrauma. 2015;32:83–94.
- de Koning ME, Spikman JM, Coers A, Schönherr MC, van der Naalt J. Pathways of care the first year after moderate and severe traumatic brain injury-discharge destinations and outpatient follow-up. Brain Inj. 2015;29:423–9.
- Wäljas M, Iverson GL, Lange RT, Hakulinen U, Dastidar P, Huhtala H, Liimatainen S, Hartikainen K, Öhman J. A prospective biopsychosocial study of the persistent post-concussion symptoms following mild traumatic brain injury. J Neurotrauma. 2015;32:534–47.
- Ponsford J, Willmott C, Rothwell A, Cameron P, Kelly A, Nelms R, Curran C, Ng K. Factors influencing outcome following mild traumatic brain injury in adults. J Int Neuropsychol Soc. 2000;6:568–79.
- Andelic N, Bautz-Holter E, Ronning P, Olafsen K, Sigurdardottir S, Schanke AK, Sveen U, Tornas S, Sandhaug M, Roe C. Does an early onset and continuous chain of rehabilitation improve the long-term functional outcome of patients with severe traumatic brain injury? J Neurotrauma. 2012;29:66–74.
- Boake C, McCauley SR, Pedroza C, Levin HS, Brown S a., Brundage SI. Lost productive work time after mild to moderate traumatic brain injury with and without hospitalization. Neurosurgery. 2005;56:994–1002.
- Cancelliere C, Kristman VL, Cassidy JD, Hincapié CA, Côté P, Boyle E, Carroll LJ, Stålnacke BM, Nygren-de Boussard C, Borg J. Systematic review of return to work after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95:S201–9.
- Vikane E, Hellstrøm T, Røe C, Bautz-Holter E, Assmus J, Skouen JS. Missing a follow-up after mild traumatic brain injury-Does it matter? Brain. Inj 2014;9052:1–7.
- Whittaker R, Kemp S, House A. Illness perceptions and outcome in mild head injury: a longitudinal study. J Neurol Neurosurg Psychiatry. 2007;78:644–6.
- Matuseviciene G, Borg J, Stålnacke B-M, Ulfarsson T, de Boussard C. Early intervention for patients at risk for persisting disability after mild traumatic brain injury: a randomized, controlled study. Brain Inj. 2013;27:318–24.
- Matuseviciene G, Eriksson G, Nygren C. Original report no effect of an early intervention after mild traumatic brain injury on activity and participation : a randomized controlled trial 2015.
- Carroll LJ, Cassidy JD, Holm L, Kraus J, Coronado VG, Injury WHOCCTF on MTB. Methodological issues and research recommendations for mild traumatic brain injury: the WHO collaborating centre task force on mild traumatic brain injury. J Rehabil Med. 2004;(43 Suppl):113–25.
- Patel MB, Wilson LD, Bregman J a., Leath TC, Humble SS, Davidson MA, de Riesthal MR, Guillamondequi OD. Neurologic functional and quality of life outcomes after TBI: Clinic Attendees versus Non-Attendees. J Neurotrauma. 2015;6:150424112216002.
- Corrigan JD, Harrison-Felix C, Bogner J, Dijkers M, Terrill MS, Whiteneck G. Systematic bias in traumatic brain injury outcome studies because of loss to follow-up. Arch Phys Med Rehabil. 2003;84:153–60.
- McCullagh S, Feinstein A. Outcome after mild traumatic brain injury: an examination of recruitment bias. J Neurol Neurosurg Psychiatry. 2003;74:39–43. doi:10.1136/jnnp.74.1.39.
- Scholten AC, Haagsma J a., Panneman MJM, van Beeck EF, Polinder S. Traumatic Brain Injury in the Netherlands: Incidence, Costs and Disability-Adjusted Life Years. PLoS One. 2014;9:e110905.
- Faul M, Xu L, Wald M, Coronado V. Traumatic brain injury in the United States: emergency departments visits, hospitalizations and deaths 2002-2006. Centers Dis Control Prev Natl Cent Inj Prev Control. 2010:2–70.