ABSTRACT
Primary objective: Communication impairments associated with acquired brain injury (ABI) are devastating in their impact on family, community, social, academic, and vocational participation. Despite international evidence-based guidelines for communication interventions, evidence practice gaps include under identification of communication deficits, infrequent referrals, and inadequate treatment to realize functional communication outcomes. Evidence-informed communication intervention requires synthesis of abundant interdisciplinary research. This study describes the development of the model of cognitive-communication competence, a new model that summarizes a complex array of influences on communication to provide a holistic view of communication competence after ABI.
Research design: A knowledge synthesis approach was employed to integrate interdisciplinary evidence relevant to communication competence.
Methods and procedures: Development of the model included review of the incidence of communication impairments, practice guidelines, and factors relevant to communication competence guided by three key questions. This was followed by expert consultation with researchers, clinicians, and individuals with ABI.
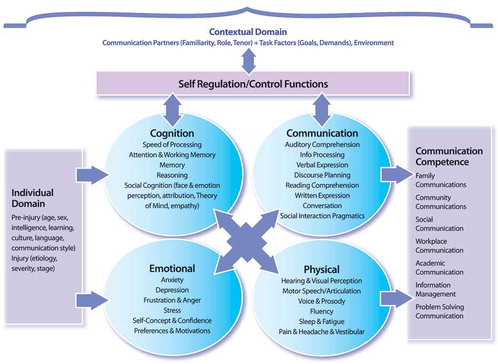
Main outcomes and results: The resulting model comprises 7 domains, 7 competencies, and 47 factors related to communication functioning and intervention.
Conclusion: This model could bridge evidence to practice by promoting a comprehensive and consistent view of communication competence for evidence synthesis, clinical decision-making, outcome measurement, and interprofessional collaboration.
Introduction
This paper presents the development of the model of cognitive-communication competence to assist in conceptualizing the full range of communication impairments after acquired brain injury (ABI), the influences on communication, and the analysis of evidence-based interventions. Such a model could be used not only to guide clinical decision-making but also to promote a shared understanding of communication deficits and interventions among health policy advisers, administrators, and funders who create the conditions for implementation of practice guidelines. It is proposed that such a model could be used as a basis for education, identification, programme planning, assessment planning, and treatment design to facilitate implementation of existing practice guidelines and to identify opportunities for development of new ones. The paper ends with a summary of evidence-based best practices that can help to reduce the negative effects of communication disorders and improve the lives of those who experience them.
Communication impairments after ABI are prevalent and devastating. The majority of individuals who sustain an ABI will experience some form of communication impairment with reported incidence rates commonly higher than 75% (Citation1-Citation4). Research indicates that even those with mild brain injury should be screened and evaluated for possible communication disorders (Citation5–Citation7). These communication deficits disrupt family communications (Citation8,Citation9); social participation (Citation10,Citation11), independence in community interactions (Citation12), academic success (Citation13–Citation17), and successful return to competitive employment (Citation18–Citation20).
There is a growing body of evidence that speech-language pathology (SLP) interventions can be effective in improving cognitive and communication functioning and ultimately improving the lives of those with ABI (Citation10,Citation21–Citation24). International standards and guidelines indicate that all individuals with communication impairments after ABI should be provided with SLP intervention (Citation24). Speech-language pathologists have the knowledge and skills to address communication impairment (Citation24,Citation25). Evidence supports SLP interventions to improve attention (Citation26), memory (Citation27,Citation28), social communication (Citation10,Citation29), reading comprehension (Citation30), and executive function and metacognition (Citation31). SLP assessments have been shown to be helpful in detecting subtle but debilitating deficits (Citation2,Citation6,Citation32,Citation33) and in guiding return to school (Citation14,Citation16,Citation34) and return to work (Citation19,Citation20). Evidence supports SLP involvement for individuals with ABI in acute care (Citation35–Citation37), inpatient rehabilitation (Citation38–Citation40), and community-based interventions including several years post injury (Citation8,Citation41).
Evidence to practice gaps in communication intervention
A number of evidence to practice gaps for those with communication impairment have been reported. First, while there are a range of evidence-based SLP interventions available, estimates indicate that fewer than 50% of individuals are in fact referred for SLP services (Citation1,Citation36,Citation42). In a study of 11 226 adults receiving SLP services in outpatient rehabilitation programmes in the USA, more than 54.9% had not received SLP services before being admitted to an outpatient facility, some weeks to months after onset of brain injury (Citation43). Blake and colleagues (Citation1) reviewed national stroke data and reported that while 94% of individuals were diagnosed with a cognitive or communication deficit, only 45% were referred for SLP services and more often those referrals were to address swallowing difficulties (52%), rather than communication deficits in expression (22%), comprehension (23%), or pragmatics (5%) (Citation43). In a Canadian stroke study, Salter and colleagues (Citation44) noted that while 77.5% of those screened met the threshold for possible cognitive-communication impairment, only 3.7% were referred for a full SLP evaluation. An international survey by Morgan and Skeat (Citation45) determined that only 12% of centres had routine procedures for referral to SLP and few had set referral criteria or established referral protocols. Edwards and colleagues (Citation42) reported the following percentage of missed communication and cognitive deficits when formal screening procedures were not employed: anomia (97%), hearing impairment (86%), aphasia (79%), and memory impairments (31%). Several reasons for lack of referral to SLP services have been postulated including lack of awareness of the full range of possible communication deficits (Citation13); lack of understanding of available SLP treatments (Citation1); unclear identification, screening, and referral systems (Citation42,Citation45); lack of physician awareness of SLP services (Citation46); and a generalized underutilization of allied health expertise (Citation47). Frequently, the more obvious communication impairments in motor speech, aphasia, fluency, or voice prompt referral for SLP intervention while the more prevalent, subtle, but equally debilitating cognitive-communication disorders are overlooked, thus depriving individuals of access to evidence-based interventions (Citation1,Citation36). Although social communication deficits have been noted in the majority of severely injured adults with ABI (Citation48,Citation49), referral rates to SLP for social or pragmatic treatment are as low as 3–5% in large US national data collection samples (Citation43).
Fair and timely access to communication interventions requires evaluation methods that consider the multiple cognitive, emotional, and physical influences on real-world communication performance, and that incorporate measures with sufficient sensitivity and ecological validity to detect these deficits (Citation50–Citation53). Communication deficits are underidentified due to use of screening and assessment measures that lack the sensitivity to detect subtle but functionally significant communication deficits (Citation7,Citation14,Citation54,Citation55). Also, referral processes and care pathways tend to focus disproportionately on swallowing or motor speech deficits to the exclusion of other equally pressing communication concerns (Citation36,Citation40,Citation56). In addition, clinicians require guidance in selecting the most accurate, comprehensive, relevant, and ecologically valid assessment tools from a growing range of standardized tests, (Citation7,Citation51,Citation57), activity, and participation measures (Citation7,Citation10,Citation50,Citation52,Citation53,Citation58–Citation61).
Significant gaps in treatment service also have been noted including premature discharge from treatment or inadequate treatment to realize functional goals in social, academic, or workplace communications (Citation14,Citation19,Citation31,Citation43,Citation62). Current practice guidelines recommend interventions be contextualized by including the communication demands of the individual’s life, involving communication partners, and promoting self-coaching, self-regulatory, or metacognitive strategy instruction and providing tailored supports for return to work, school, or social participation (Citation23,Citation24). Yet speech-language pathologists cite significant barriers to implementation of evidence guidelines such as lack of time (92.3%), lack of resources (81.7%), or lack of interest from others (58.2%) (Citation63). The analysis, interpretation, and application of evidence relevant to communication interventions after ABI are increasingly onerous, requiring clinicians to synthesize over 8000 articles with more than 49 key search terms, and more than 70 clinical practice recommendations (Citation22–Citation24,Citation64,Citation65). Finally, use of outcome measures that do not reflect the full range of communication functioning, or the complex demands of real-world communication activities or participation lead to under-reporting of communication problems, untimely discharge, and false indications of resolution of problems (Citation32,Citation52).
Rationale for a new model of cognitive-communication competence
Evidence-based intervention for individuals with ABI-related communication disorders could be improved through the development of a comprehensive and unifying model of communication competence. Models provide a guide or map for selection and evaluation of published data, integration of findings, clinical decision–making, and delineation of knowledge gaps and areas for future research. (Citation66). A model of communication competence could provide some structure for evidence selection, synthesis, and application of the vast and varied evidence relevant to communication disorders. This is evidence that spans the fields of SLP, psychology, neuroscience, rehabilitation, and education and concerns the complex interplay between cognitive, communicative, emotional, and physical factors (Citation1,Citation13,Citation18,Citation24,Citation40). Currently communication disorders that occur due to underlying cognitive impairment are well defined within the field of SLP (Citation24,Citation67,Citation68) but less well understood by the wider healthcare systems responsible for policy development, funding, and outcome measurement (Citation5,Citation13,Citation36). A unified model could create a shared vision of the communication needs of those with ABI to improve their access to disability supports, community-based rehabilitation services, educational accommodations, and insurance or healthcare funding to address communication challenges. In summary, a model of cognitive-communication competence could promote greater consistency in referral and assessment practices; guide treatment and application of evidence-based practice; and promote greater understanding of the full range of communication impairment for improved data collection, and planning of service needs.
The model of cognitive-communication competence
The goal in developing the model of cognitive-communication competence was to develop an integrated, consistent, and unifying conceptual model of communication that allows us to map the key variables, synthesize findings of multiple lines of inquiry, and promote clinical application as well as continued growth of meaningful evidence for optimal communication intervention. This model was designed to meet the following objectives:
To highlight the central role of communication skills and processes in all interactions including community integration and societal participation, and to stimulate consideration of the importance of communication sampling characteristics, communication complexity, and communication task demands in all research, rehabilitation, and real-world evaluations.
To depict communication as a complex, multifaceted construct with a range of individual, cognitive, communicative, emotional, physical, self-regulatory, and contextual influences.
To synthesize existing evidence (i.e. practice standards, guidelines, evidence reviews) relevant to communication disorders including International Guidelines for Cognitive-Communication Intervention (Citation24) and evidence for cognitive-communication interventions gleaned from systematic reviews and meta-analyses (Citation10,Citation22,Citation23,Citation26,Citation28,Citation29,Citation51,Citation52,Citation69,Citation70).
To integrate interdisciplinary fields of inquiry in SLP, psychology, rehabilitation, and education, from a range of perspectives including instructional practices (Citation71), metacognitive strategy instruction (Citation31), social communication, pragmatics, discourse, communication partner training (Citation10,Citation72,Citation73), gist reasoning, social cognition, and executive functioning (Citation13,Citation21,Citation58,Citation70,Citation74–Citation79). A model could help to interpret and integrate an array of published facts and map them onto a conceptual framework that gives them greater meaning and applicability (Citation80).
To denote the importance of context in communication competence, including situational, and communication partner demands, by incorporating the tenets of the World Health Organization’s International Classification of Functioning (Citation81) which expands the scope beyond communication impairments to the activity limitation and participation restrictions they entail (Citation82).
To promote communication competence in real-world settings as the desired outcome of communication intervention. Communication competence is a complex construct that has been variously defined within the linguistics, SLP and education literature (Citation83–Citation85). Communication competence involves multiple skills including the strategic selection of both perceptive and expressive communication behaviours from a diverse repertoire of possibilities, effective and appropriate employment of communication skills and strategies (i.e. content, form, and use of language), consideration of the communication partner’s perspective, and strategic and dynamic adaptation of communication to varied contexts in order to achieve personal goals while considering those of others. (Citation85–Citation87). Ylvisaker and colleagues (Citation88) stressed that the goal of communication competence beyond ‘appropriateness’ is communication ‘success’ which includes the ability to affect the behaviour of others, gain acceptance by peers and family members, establish friendships, and meet the demands of school, work, and community. Finally, an updated definition of communication competence must integrate the tenets of the World Health Organization (Citation81) by referring to activity and participation levels of communication health (Citation87). Communication competence then is defined as the strategic and effective employment of communication perception and production skills, influenced by a multifaceted set of cognitive, linguistic, emotional, and self-regulatory abilities, within daily activities and dynamic interpersonal exchanges, to meet the individual’s participation goals within family, community, social, work, academic, and problem-solving contexts.
It is proposed that a comprehensive model could convey the full range of communication impairments after ABI, provide a map for integrating disparate findings, and provide a structure for ongoing development of best practices for communication interventions.
Method
The steps followed in developing the model of cognitive-communication competence are presented in .
Define, review, and quantify the full range of communication impairments after ABI
This model was developed for those with ABIs that occur after birth and are non-progressive, including such diagnoses as stroke, traumatic brain injury (TBI), concussion, encephalitis, Lyme disease, meningitis, hypoxia, aneurysm, seizure disorder, aneurysm, tumour, and right hemisphere disorder. It excludes progressive neurological disorders such as communication disorders arising from dementia, multiple sclerosis, Parkinson`s disease, or Huntington`s disease. It excludes aetiologies that arise prior to or at birth such as cerebral palsy, autism spectrum disorder, or foetal alcohol syndrome.
Communication deficits have been reported after most forms of ABI including TBI (Citation21), right hemisphere disorder (Citation1,Citation2,Citation40), concussion and mild brain injury (Citation7,Citation39,Citation54), blast injury (Citation25), stroke and aphasia (Citation36,Citation63), penetrating brain injury (Citation89), hypoxic ischaemic brain injury (Citation42,Citation90), and encephalitis (Citation29,Citation91,Citation92).
The first step in developing the model was to review evidence regarding the incidence of the full range of communication impairments after ABI. In order to obtain the most current and comprehensive estimates of communication impairment after ABI, a literature search was conducted using terms ‘communication impairment’ and ‘brain injury’ and ‘incidence’ limited to the years 2000–2016 utilizing the following databases: MEDLINE, PsycINFO, and Embase and yielding 152 articles. Seminal textbooks in the field of cognitive-communication disorders were also searched for incidence and prevalence data. Estimates to follow are based on the best determination that can be made from the available literature.
After ABI the most prevalent communication impairments are cognitive-communication disorders with incidence rates as high as 75–100% depending on sampling characteristics (Citation3,Citation4,Citation36,Citation40,Citation93–Citation96). Cognitive-communication disorders are difficulties in communicative competence (listening, speaking, reading, writing, conversation, and social interaction) that result from underlying cognitive impairments (attention, memory, organization, information processing, problem solving, and executive functions) (Citation24,Citation67,Citation68). Cognitive-communication disorders are now widely accepted as a diagnostic intervention category (Citation24) . They have been established within the scope of SLP practice, guidelines, and standards internationally including in the USA (Citation67), Canada (Citation68), Scotland (Citation97), and New Zealand (Citation98). They are recognized as unique disorders which require individually tailored programmes, and consideration of multiple influences on communication, and speech-language pathologists are uniquely trained to detect and remediate these disorders (Citation24).
Dysarthria and apraxia are motor speech disorders which occur in less than 35% of individuals with ABI, again, depending on population and sampling characteristics (Citation97,Citation99,Citation100). Aphasia is a disturbance in specific language functioning that is characterized primarily by errors at the word and sentence level. It is common after stroke, but occurs in only 1–2.5% of individuals with TBI (Citation5,Citation23,Citation96), although it has been reported as high as 32%, again, depending on sampling characteristics (Citation3) . Stuttering or difficulties with speech fluency occur after ABI at a rate of less than 1% (Citation5). Finally, voice disorders or changes in vocal quality, loudness, or pitch also occur at a rate of 0.6% (Citation5). Referral, screening, and tracking systems should therefore prioritize the more prevalent and subtle cognitive-communication disorders (Citation13,Citation24).
Review existing models of communication
Various models of communication were examined following a search of MEDLINE, PsycINFO, and Embase using the key words ‘communication’, ‘social communication’, or ‘discourse’ and ‘model’ and ‘brain injury’. These models were reviewed to delineate the primary domains of influence on communication functioning. These included global models of cognitive-communication functioning (Citation84,Citation101), pragmatics and social communication (Citation73,Citation102–Citation105), and social cognition (Citation106). There are also specific models that detail the theoretical bases of one specific type of communication impairment including models for narrative discourse production (Citation89), motor speech (Citation107), reading comprehension (Citation17), and auditory comprehension (Citation40,Citation108). There are also models relevant to aspects of cognitive functioning that affect communication such as models of working memory (Citation109) and executive functioning (Citation110). These models provide an important foundation for the multiple contributing factors to communication performance. Review of these models underscored the need to consider all components of communication, cognition, emotional influences, physical functioning, and individual and contextual influences in communication. It also indicated that while there are models of various aspects of communication there appears to be no overarching model that integrates all factors for consideration in communication competence. There remains a need for a model with a central focus on communication that includes all aspects of communication (comprehension and expression; spoken and written, verbal and non-verbal, impairment and participation), that indicates the multifaceted influences on communication (i.e. cognitive, physical, emotional), and that can apply to all communication interventions by speech-language pathologists along the post-injury continuum.
Select domains and factors relevant to communication competence
The domains and factors within the model were selected from classifications presented in existing models, published standards and guidelines, and systematic reviews. An initial set of domains and factors were derived from the Cognitive-Communication Intervention Review Framework presented in a knowledge translation paper that synthesized 20 systematic reviews (Citation23). Next, guidelines for cognitive-communication intervention were reviewed including guidelines from the USA (Citation67), Canada (Citation68), Scotland (Citation97), New Zealand (Citation98), and the international guidelines called the INCOG guidelines (Citation24) . The 7 domains and 47 factors are presented in the results section.
Research of factors within the model
The first author and a research assistant then conducted multiple literature searches from April 2016 to April 2017 to provide an overview of the evidence base for each factor and its relationship to communication competence. Search terms were developed for each factor within the model by reviewing previous models, guidelines, and professional databases (Citation111–Citation113) These search terms were applied to the following databases: MEDLINE, PsycINFO, and Embase using the key term within the model and ‘communication’ and ‘brain injury’ . The searches were limited to human studies in the English language in the years 2000–2016. Studies were excluded if they did not refer to acquired, non-progressive brain injury (i.e. Parkinson’s disease, multiple sclerosis, HIV, schizophrenia), did not relate to communication intervention, or did not relate to clinical practice (i.e. administrative practice). Initial searches in the cognitive domain yielded hundreds of studies by using the search formula ‘cognition’ or ‘communication’ and ‘brain injury’. These searches were then further limited by using the more communication focused search term ‘cognitive-communication’. Using this method, the number of studies for the attention factor for example reduced from 842 to 18. Seminal textbooks in the field were also searched. This synthesis, construction, and refinement of the model was an iterative, cyclical process. Studies produced were then reviewed to answer the following three guiding questions relevant to the factor’s inclusion in the model:
Has this factor been shown to significantly affect communication competence?
Has this factor been shown to be an essential component of assessment of communication deficits after ABI?
Is there evidence that treatment for this factor can improve communication competence?
The goal was to provide a rationale for inclusion of each factor in the model rather than to list or evaluate all possible research within each domain. The resulting model of cognitive-communication competence and search findings are summarized in the next section.
Expert consultation
The model was then reviewed by an expert panel of six researchers in SLP who are members of the TBI research writing team of the Academy of Neurological Communication Disorders (ANCDS). All members of the ANCDS group conduct research specific to evidence-based practice in cognitive-communication disorders after ABI. The names of each member and their fields of research are summarized in . We discussed each of the model components in the context of its relevance to cognitive-communication competence in four conference calls from April 2016 to April 2017. Feedback on the factors of the model and suggested revisions were provided via email throughout this period. While consensus was reached quickly on most aspects of the model, much discussion ensued regarding the placement of items relating to executive functioning, self-regulation, and metacognition. Resolution was reached by placing these items on the top of the model in a section called ‘control functions’ to illustrate their supervisory or regulatory function while also noting they are part of the cognitive domain. Three additional leading research scientists in cognitive-communication disorders were invited to review the model. Their names and areas of expertise are also listed in . These researchers provided additional guidance with respect to inclusion of factors relating to social cognition and provided seminal articles in the field for review. Six clinicians with 18–36 years of experience in cognitive-communication disorders from acute care to community also reviewed the model. The names of these individuals are presented in . These consultations occurred in email and telephone discussions from April 2016 to April 2017. The clinicians expressed that the model was clear and comprehensive and reflected the multiple influences on communication in their clinical practice. Their input led to an expansion of the list of cognitive-communication competencies and the individual factors to be considered in intervention.
Table 1. Expert Consultation: Research reviewers.
Table 2. Expert Consultation: Clinician reviewers.
The model was then shared with a group of 10 adults with mild to moderate ABI who were part of a social communication group led by the author. These individuals stated that the model was a useful education tool and would help them to convey the multiple factors that affected their communication performance. They also indicated that the terminology within the model was comprehensible.
The model of cognitive-communication competence
The model of communication competence incorporates seven domains of functioning that contribute to communication success in seven key areas of communication competence. Within each domain are several factors for consideration based on current evidence. The model is presented in . The rationale for inclusion of each domain and its component factors is presented below.
Components of the model of cognitive-communication competence
Individual domain
International standards for cognitive-communication intervention recommend that rehabilitation of individuals with cognitive-communication disorders be grounded in analysis of an individual’s unique characteristics, needs, life contexts, goals, and skills (Citation24). Pre-injury factors that have been found to influence communication outcome include age and stage of neurological and cognitive development (Citation114–Citation117); education, learning skills, learning disability (Citation118), sex (Citation118–Citation120); mental health concerns, previous brain injury, or substance abuse (Citation118,Citation121–Citation124). Injury-related factors that influence communication include aetiology, severity, and location or extent of neurological impairment, and time since injury or onset of condition (Citation114,Citation125–Citation127). Individual differences in psychological response to trauma that warrant consideration include resilience, motivation, or adjustment (Citation128,Citation129). Communication outcomes can be influenced by a complex interaction between these pre- and post-injury individual characteristics as well as contextual and environmental factors (Citation130).
Contextual or environmental domain
The contextual domain is placed in an arc at the top of the model to emphasize the overarching need to consider the communication demands of the individual’s life, to involve communication partners, and to evaluate, support, and stimulate communication in communication contexts that are as similar as possible to the contexts of the individual’s life (Citation24). Many aspects of communication context have been found to influence communication competence including communication partner characteristics (relationship, familiarity, age, roles, authority differential, cues, and skills) (Citation131–Citation137) and communication tasks demands (i.e. environment, interruptions, predictability, load on working memory, response requirements, stimulus characteristics, etc.) (Citation94,Citation132,Citation137,Citation138). Communication partners (family, peers, etc.) can contribute critical screening and assessment information (Citation18,Citation52,Citation139) and training of communication partners has been found to improve communication competence in paid carers (Citation134,Citation136,Citation140), community members (Citation12), and family members (Citation135,Citation141). Communication interventions must incorporate the tenets of the World Health Organization’s International Classification of Functioning, Disability and Health, by considering the interaction between an individual’s health condition, life contexts (roles, activities, participation), and their goals and preferences (Citation87,Citation142).
Cognitive domain
There are multiple cognitive processes that influence communication competence. Communication and cognition are highly interdependent constructs and there are multiple cognitive processes that influence communication competence (Citation28,Citation143). Cognitive factors selected for inclusion in the model were based on the analysis of previously described practice guidelines (Citation24,Citation68,Citation144) models of cognitive-communication functioning and systematic reviews of cognitive interventions to improve communication functioning (Citation23) .
Control functions
Control functions refer to a set of cognitive processes that regulate thinking, behaviour, and communication (Citation75,Citation110,Citation145). These functions are part of the cognitive domain but are illustrated separately at the top of the model to highlight their superordinate role in coordinating, integrating, or regulating cognitive and communication processes (Citation29,Citation75,Citation103,Citation110,Citation145,Citation146). Converging evidence indicates that these higher-order functions are frequently impaired after ABI and can influence communication competence with respect to energization (initiation of conversation or social interaction); behavioural and emotional self-regulation (inhibition of undesired responses, profanity, personal disclosure; modulation of emotion, impulse control; flexibility, adaptation); executive functions (goal-directed communication, topic maintenance, task monitoring); and metacognition (self-appraisal, awareness, conversational repair, strategy application, adaptation to the needs of the conversational partner) (Citation75,Citation103,Citation110,Citation145–Citation149). The separate depiction of these control functions at the top of the model is justified by evidence of their overarching influence on communication and social participation (Citation16,Citation21,Citation22,Citation31,Citation34,Citation40,Citation65,Citation75,Citation150). Metacognitive strategy instruction and self-regulatory or self-coaching approaches to communication interventions are well supported by the evidence (Citation29,Citation75,Citation151). Therefore control functions, though part of the cognitive domain, are depicted separately at the top of the model to highlight the supervisory or regulatory functions that work in concert to direct functional communication.
Speed of processing
Speed of processing is frequently impaired following ABI and has been found to adversely affect many aspects of communication including social communication (Citation103,Citation152,Citation153), reading comprehension (Citation154), and discourse (Citation18). Speed of processing is critical to the ability to process complex social interaction, facial expressions, conversational hints, interjections, and contextual influences, not only to keep pace with the complex processing of social situations (Citation103,Citation154,Citation155) but also to inhibit unwanted behaviours in a timely fashion (Citation152). Slower processing after ABI has also been well documented during completion of complex communication tasks that simulate the tasks of work, school, or community interaction (Citation19,Citation32,Citation33). Speed of processing is included in the model to convey the need to evaluate cognitive-communication performance using timed tests, to evaluate real-world communication demands in terms of speed and efficiency in addition to accuracy, and to address efficiency of communication through provision of supports and accommodations when required.
Attention and working memory
The ability to direct, sustain, shift, suppress, and regulate attention underlies many aspects of communication (Citation2,Citation26,Citation103,Citation156). Challenges with attention after brain injury have been implicated in communication impairments in auditory comprehension (Citation157,Citation158), discourse production (Citation147,Citation159), social communication (Citation103), reading comprehension (Citation16,Citation154), and written expression (Citation16). Assessment of communication after ABI requires evaluation of the potential influences of sustained attention, selective attention, divided attention, and working memory (Citation7,Citation13,Citation28,Citation39,Citation158,Citation160). Evidence supports attention interventions to promote functional gains in communication, with direct attention training and metacognitive strategy instruction garnering the most evidence to date (Citation26,Citation39,Citation160–Citation164).
Working memory is a limited capacity system for storage and manipulation of information (Citation109) that helps us to maintain and update information held in mind (Citation79). It is closely linked to attentional control and executive functioning in that it involves inhibition or suppression of interfering distractions, mental set shifting, self-monitoring, and updating. (Citation165,Citation166). Working memory plays an important role in communication for such things as tracking what has been said, what we are about to say, what we read, or what we are planning to write. Working memory deficits after ABI have been implicated in communication impairments including problems with auditory comprehension of inferential or ambiguous material (Citation94,Citation167,Citation168), discourse comprehension (Citation78,Citation169), discourse production (Citation170), social communication (Citation103), reading comprehension (Citation17), and written expression (Citation16).
Memory
Memory functions have a place in the model because memory is critical to language processing and production (Citation171). Memory impairments are common after ABI with reported incidence rates from 20% to 79% depending on aetiology, severity, and time post injury (Citation172). They may involve episodic, declarative, or prospective memory and have been found to affect communication functions such as auditory comprehension, reading comprehension, verbal expression and discourse, written expression, or social communication (Citation76,Citation78,Citation89,Citation154,Citation170,Citation173,Citation174). Evidence supports the use of the following memory intervention approaches for speech-language pathologists: use of external memory aids (Citation22,Citation28), internal memory strategies (Citation27), spaced retrieval (Citation175), instructional practices such as systematic instruction and errorless learning (Citation92,Citation176), and prospective memory training (Citation177). Therefore memory is depicted in the model to prompt consideration of its contribution to communication competence and the development of optimal therapeutic instruction.
Social cognition
Social communication is a dynamic process in which one makes decisions based on social knowledge, perceptions of emotional and situational cues, and inferences about the conversational partner’s perspective while adapting their communication to the situation (Citation79). These abilities are frequently disrupted after ABI due to social cognition impairments in Theory of Mind (understanding of others’ mental states, thoughts, beliefs, desires, intentions), perspective taking and cognitive empathy, emotional perception (interpretation of non-verbal, facial, or vocal cues), and social inference (interpretation of sarcasm, lies, irony, certain types of humour) (Citation77,Citation79,Citation103,Citation106,Citation178). Individuals with brain injury may be unable to understand or describe their own emotions (i.e. alexithymia), or to empathize or to respond adequately to another’s display of emotion (Citation106,Citation179,Citation180). Social cognition’s inclusion in the model reflects the need to evaluate these skills and to include participation in dynamic, interactive, and even emotive conversational contexts in both intervention and research.
Reasoning and problem solving
Reasoning involves the analysis or synthesis of facts in order to draw a conclusion or make a decision. It is involved in communication acts such as explaining, discussing, listening to a lecture, providing a comparison, reading for new information, expository or essay writing, persuading or negotiating, summarizing, expressing a preference, or participating in a social debate (Citation9,Citation181–Citation185). Verbal reasoning is mediated by specific areas of the prefrontal cortex (Citation183) and involves contributions from other cognitive processes such as working memory, attention and inhibitory control. Reported reasoning deficits after ABI include reduced ability to do the following: extract the ‘gist’ or the pertinent information, eliminate irrelevant information, weigh the facts, flexibly revise based on new information, generate alternatives, or predict consequences (Citation19,Citation20,Citation32,Citation33,Citation74). Problem solving incorporates reasoning and decision-making and also includes the ability to identify the problem, to plan and implement solutions, and to monitor, evaluate, refine, and revise. During problem solving individuals with ABI may have difficulties with efficiency, inferential thinking, analogous thinking, interpretation of abstract ideas, flexibility, generation of options, interpretation or anticipation of multiple perspectives, organization, persistence, self-monitoring, and self-regulation (Citation9,Citation32,Citation33,Citation94,Citation182). Clinically those with ABI may present with difficulty following discussions, understanding team meetings, expressing a choice, or interpreting education or counselling sessions. Deficits in verbal reasoning and decision-making have been shown to compromise communication competence in academic (Citation181), workplace (Citation20), and family contexts (Citation9). There is evidence to support interventions for verbal reasoning and problem solving to improve communication competence (Citation31,Citation186,Citation187).
Communication domain
Communication is our most complex human function and warrants specific examination in research, clinical practice, and outcome measurement after brain injury (Citation21,Citation23). In the model of cognitive-communication competence communication is viewed as the primary domain of focus within a complex interplay of cognitive, linguistic, emotional, physical, personal, and contextual factors. Communication is the interpersonal exchange of ideas, information, needs, and perspectives that can be intentional or unintentional. Brain injury can impair any modality of communication (e.g. listening, speaking, reading, written expression, non-verbal expression), any aspect of the language system within that modality (e.g. phonology, semantics, syntax, pragmatics), or any aspect of non-verbal communication (i.e. facial expression, tone of voice) (Citation21,Citation40). The model is intended to demonstrate the full range of communication functions and the complex interplay of factors that form an individual’s constellation of strengths and weaknesses (Citation21).
Auditory comprehension
Auditory comprehension is included in the model as a key component of communication competence and a complex area of functioning requiring close examination of contributing linguistic, cognitive, and perceptual demands of a given listening task or context. Comprehension after ABI can be affected at a variety of levels including the lexical, syntactic, semantic, supralinguistic, or pragmatic levels (Citation188) as well as the literal, interpretive, critical, and metacognitive levels (Citation84). Reported auditory comprehension deficits after ABI include difficulties with accurate or efficient processing of complex vocabulary (Citation14), sarcasm and irony (Citation189), implied information or inference (Citation94,Citation190), hints (Citation155); non-literal or figurative language (metaphor, proverbs, idioms) (Citation14,Citation94,Citation168,Citation191), indirect requests (Citation158), ambiguous sentences (Citation167), and complex semantic or syntactic relationships (Citation14,Citation51,Citation54,Citation78,Citation145,Citation192). Cognitive factors have been shown to play a key role in comprehension deficits including impairments in working memory, attention, speed of processing, organization, reasoning, social cognition or theory of mind, and executive functioning and self-regulation (Citation77,Citation94,Citation114,Citation167,Citation169,Citation190,Citation191,Citation193). A variety of task demands can affect comprehension including syntactic complexity, predictability of stimulus material, amount of contextual support, and the speaking rate of the conversation partner (Citation158,Citation190,Citation193). Both verbal and non-verbal aspects of comprehension need to be incorporated in screening tools, referral criteria, and outcome measures (Citation84,Citation194). Several approaches to auditory comprehension intervention are supported in the literature including gist reasoning training (Citation78,Citation187), metaphor training (Citation168), inference training (Citation40), and metacognitive strategy instruction (Citation150).
Verbal expression and discourse
Difficulties with expressive communication after ABI include errors and delays in word retrieval and disruption of verbal fluency (Citation6,Citation54,Citation194,Citation195) and problems with production of timely, meaningful, and organized discourse with sufficient regulation of quality, topic selection, or listener-oriented behaviours (Le et al, 2011; (Citation14,Citation50,Citation52,Citation79,Citation102,Citation196). Discourse may be sparse, vague, or impoverished or excessively detailed, and tangential (Citation21,Citation50,Citation170). Difficulties after ABI may occur in procedural discourse such as providing instructions or directions (Citation197), in narrative discourse or story telling (Citation198,Citation199), in persuasive discourse or the ability to persuade, sell, negotiate, or argue (Citation200,Citation201), in expository discourse or the ability to explain or provide a rationale (Citation32,Citation33); or in conversational discourse (Citation52,Citation53,Citation147,Citation202). These difficulties may arise from underlying problems with working memory, organization, executive functions, or self-regulation (Citation50,Citation78,Citation89,Citation105,Citation143,Citation145,Citation196,Citation198,Citation203,Citation204). The model depicts these interactions with arrows between the communication and cognitive domains and the control or self-regulatory domains.
The model illustrates the interaction between the communication and context domains because facility with discourse can vary as a function of task, sampling technique, discourse analysis, conversation partner characteristics, or amount of contextual support (Citation52,Citation53,Citation132,Citation137). Research supports assessment and treatment using a range of discourse tasks, contexts, communication partners, and opportunities for practice and feedback in communication contexts that are similar to the individual's daily life (Citation52,Citation205,Citation206). Discourse measures that have been found to differentiate performance of those with and without brain injury include measures related to story completeness, productivity, efficiency, content accuracy, coherence, and organization or story grammar (Citation89,Citation207). Evidence-based interventions for discourse include communication groups, organizational strategies, communication coping strategies and communication partner training (Citation12,Citation141,Citation208–Citation210).
Pragmatics and social interaction
In developing the model, consideration was given to varied terms used to categorize aspects of social communication competence. Pragmatics refers to the ability to use language in context (Citation73). The term ‘pragmatics’ has historically been used in SLP (Citation211,Citation212) to refer to aspects of communication competence such as the ability to use language to accomplish social goals, to manage turns and topics in conversation, and to express appropriate degrees of politeness, awareness of social roles, and recognition of others’ conversational needs (Citation213). Prutting and Kirchener’s (Citation214) taxonomy of pragmatic behaviours includes such verbal behaviours as topic selection, maintenance and change, turn taking, lexical selection, cohesion; vocal intensity, prosody, fluency, and non-verbal aspects such as facial expression, eye gaze, and body movements. Turkstra and colleagues’ review of pragmatic theory, development, and interventions indicates that pragmatic communication is a multifaceted construct that incorporates aspects of communication development, social cognition, and context (Citation73).
Social communication is an overlapping term that refers to the ability to express meanings and intents and understand those conveyed by others through use of verbal and non-verbal skills and knowledge of social conventions within varied environments, and with varied communication partners (Citation10). Whereas the term pragmatics is often used to refer to the skills of the individual, social communication is used as a broader term that includes the effectiveness of the exchange between communication partners in context. Both terms, pragmatics and social communication, are used interchangeably in the SLP literature (Citation10). After some discussion with members of the consultation team it was decided to include both the terms ‘pragmatics’ and ‘social interaction’ in the list of factors within the communication domain to delineate the communication skill set an individual possesses. The term ‘social communication’ was placed on the right of the model as one of the target communication competence outcomes, the effective use of social communication in context.
Social communication success is determined by the goals, conventions, boundaries, or expectations of that particular context and can be enhanced or inhibited by the skills of the communication partner (Citation72,Citation133). Social communication impairments after ABI include difficulties with such skills as conversational initiation, fluency (speed, efficiency, revisions, mazes, false starts, repetitions), topic management (maintenance, turn taking, shift), listener-oriented behaviours or perspective taking, self-regulation (of topics, comments, tone, interjections), and adaptation to changing circumstances or distractions in the environment (visual, auditory, interruptions) (Citation29,Citation50,Citation72,Citation114,Citation215–Citation217). These deficits can arise as a result of cognitive, communication, emotional, and physical factors including deficient attention, organization, working memory, or executive functions (Citation114,Citation143,Citation159). They can place individuals at increased risk of social isolation, marital breakdown, and limitations in academic and vocational success (Citation209,Citation218,Citation219). Social communication is dynamic and interactive and should be evaluated and treated within the targeted context to whatever extent possible (Citation10). Evidence supports SLP treatment for social communication deficits (Citation10) including context-sensitive approaches (Citation10,Citation22,Citation23,Citation216), communication partner training (Citation12,Citation134,Citation136), group interventions (Citation8,Citation209,Citation220,Citation221) peer mentoring (Citation11), social cognition approaches (Citation222), and behavioural interventions (Citation88).
Reading comprehension
Reading comprehension is included in the model because deficits are prevalent after ABI and have implications for community independence, social, academic, and vocational competence (Citation16,Citation69). Reading comprehension involves a complex array of visual, perceptual, and cognitive skills (attention, memory, working memory, executive functions) as well as linguistic or communication skills (word comprehension, sentence processing, discourse comprehension) (Citation16,Citation69). Reading difficulties after ABI are varied and may include problems with oral reading, decoding, tracking, speed, or stamina for reading over time (Citation16,Citation17,Citation69). Most commonly individuals with ABI have difficulties at the level of text or discourse comprehension (Citation16,Citation69) including problems understanding inference or implied information (Citation94); understanding the inherent organization of a text or story grammar (Citation223), recalling details (Citation14,Citation187); or difficulty understanding the main point or gist or moral of a story (Citation224). Evidence supports reading assessment of text length materials with sufficient cognitive and linguistic challenge and ecological validity to simulate the individual’s academic, vocational, or daily life reading requirements (Citation14,Citation16,Citation223). Reading for academic or vocational purposes involves goal-directed processes that place demands on executive functioning including the ability to understand task demands, attend selectively to important materials, ignore less relevant details, monitor, and make corrections while reading (Citation16).
Assessment should consider the characteristics of reading materials such as degree of predictability, analysis and synthesis, amount of organizational structure, amount of inference, speed and stamina over time, and requirements to analyse, synthesize, and summarize materials (Citation16,Citation30). Assessment should also consider the cognitive demands placed on the reader such as to determine the goal or purpose of the reading task; maintain or shift goals fluidly across task requirements; make inferences about task expectations (e.g. what the teacher or employer wants or needs); read large volumes of material efficiently; make connections among the ideas presented in the text, make predications, develop coherent interpretations, or provide explanations and summaries (Citation16). There is evidence to support SLP intervention for reading comprehension (Citation22,Citation43,Citation69) including the use of gist reasoning training, organizational training, compensatory strategies, and metacognitive strategies, and oral reading approaches (Citation16,Citation17,Citation69,Citation187).
Written expression
Individuals with ABI may have written expression difficulties due to problems with motor control, word retrieval, sentence formulation, generation or discourse planning. Written expression difficulties are frequently related to underlying cognitive deficits in attention, working memory, organization, social cognition, executive function and self-regulation (Citation14,Citation16,Citation225). Many standardized tests assess writing skills that have matured by adolescents and there is a need to evaluate higher-level written expression skills (Citation14). Sufficiently sensitive written expression tasks are those that require the individual to analyse, synthesize, and formulate written communications that are similar to their academic, social, or vocational demands in writing activities such as homework assignments, peer conversations, daily scheduling, letters, summaries, and written explanations (Citation14,Citation16,Citation19,Citation20,Citation32,Citation33,Citation226). Difficulties with written expository and persuasive discourse have been noted in complex assessment tasks that simulate the writing requirements of work or school (Citation19,Citation32). Intervention research to date favours use of individualized approaches, compensatory strategies, technology (i.e. voice to text), organizational frameworks, graphic organizers, self-regulated strategy development, explicit instruction of specific writing conventions and genres, and metacognitive strategy instruction embedded in functional academic or vocational contexts (Citation16,Citation225–Citation227). It is hoped that the inclusion of written expression in the communication domain of the model could draw attention to its importance as a functional communication skill for future intervention research.
Physical/sensory domain
Communication is affected by a range of co-occurring or comorbid physical factors that must be considered in assessment and treatment planning. Sleep disorders are common after ABI and have been shown to adversely affect cognitive-communication performance (Citation156,Citation228). Persisting fatigue is the hallmark of ABI and can affect communication performance as well as the individual’s ability to participate in communication interventions (Citation229,Citation230). Education regarding pacing and fatigue has become an integral part of SLP intervention. Hearing difficulties after ABI are also common and consultation with an audiologist is important not only in ruling out hearing impairment but also in developing intervention plans for tinnitus and other neurologically induced hearing sensitivities (Citation231). The presence of motor speech disorders such as dysarthria and apraxia may require SLP evaluation of articulation, respiration, phonation, resonance, strength, coordination, and speed of movements (Citation232,Citation233). Voice disorders which are less common in ABI (Citation5) involve changes in the vocal quality, loudness, or pitch of voice due to changes in vocal cord movement or respiratory support for voice. Prosody disorders are also possible, particularly after right hemisphere brain damage (Citation1,Citation40,Citation94). Stuttering or difficulties with speech fluency can occur due to neurological impairment after ABI (Citation234) with reported incidence of less than 1% in a large sample (Citation5).
Comorbid physical impairments must be considered by speech-language pathologists and require informed collaboration with colleagues in the disciplines responsible for managing them. Deficits in balance, dizziness, or vestibular disorders are common even after mild TBI and can impede participation in conversation, rehabilitation, social, vocational, or academic activities due to resulting problems with driving, tolerance for transportation, fatigue, cognitive drain, or social withdrawal (Citation235). Visual perceptual impairments may occur in 54–74% of individuals with ABI (Citation236) and include problems with visual acuity, visual fields, peripheral vision, diplopia, photophobia, visual perception, and a range of binocular vision impairments relating to accommodation and convergence (Citation236–Citation238). Overall, the physical domain in the model highlights the importance not only of communication deficits that have a physical basis, but also of additional physical factors that can influence communication performance and require SLP collaboration with other disciplines (i.e. physicians, physiotherapists, optometrists, audiologists, occupational therapists).
Emotional/psychosocial domain
The emotional domain in the model represents the dynamic and complex relationship among emotional, physical, cognitive, and communication factors in determining communication competence for full life participation. ABI can result in a number of emotional or psychological challenges that are important considerations for cognitive-communication competence and require SLP collaboration with psychologists and physicians. These include anxiety, (Citation239,Citation240), depression (Citation241–Citation244), and post-traumatic stress disorder (Citation240,Citation245,Citation246). They have been associated with cognitive impairments in attention, working memory, information processing, executive functions, and processing speed and can have implications for communication competence (Citation240,Citation247,Citation248) and can also have cognitive-communication competence. In addition to these psychological diagnoses, individuals may endure problems with emotional regulation leading to excesses in irritability, aggression or quick temperedness, or emotional reductions in arousal, motivation, or drive (Citation249). Brain injury itself leads to increased stress related to the emotional consequences of trauma, loss and mourning, change in life circumstances, restrictions on activities and individual freedoms (i.e. inability to drive or work); difficulties with decision-making, reduced choice and autonomy, changes in identity and self-confidence, and a host of stressors related to marital, legal, and financial changes (Citation9,Citation219). An individual’s emotional regulation may also be affected by physical changes in sleep hygiene, medications, and pain (Citation9,Citation219). Individuals with ABI are at high risk for significant decrease in friendships and social supports and have reduced opportunity to engage in vocational and avocational or leisure activities in order to establish new friendships and this can lead to a downward spiral into stress and depression (Citation142).
The integral nature of cognitive, communication, and emotional skills in the model underscores the clinical imperative to prioritize, streamline, and stage interventions according to the individual’s specific needs. While such conditions may require a primary focus of mental health intervention from mental health professionals, speech-language pathologists may collaborate to provide cognitive-communication strategies that ease communication distress and increase overall sense of well-being (Citation208,Citation247). Communication interventions have been shown to increase measures of well-being and decrease indications of post-traumatic stress, anxiety, and depression. (Citation39,Citation208,Citation209,Citation247). Douglas (Citation208) demonstrated that speech-language pathologists can train more positive communication-specific coping skills to ease immediate distress in instances of communication breakdown. It is within the speech pathology scope of practice to evaluate and develop an optimal plan of intervention for individuals with communication impairment of any origin, including those related to emotional, behavioural, or mental health conditions or those at risk of mental health conditions due to their injuries (Citation68,Citation250). Speech-language pathologists assess and diagnose communication deficits and collaborate with those with mental health expertise on such issues as intervention, stressors, priorities, substance abuse, and behavioural dysregulation. Clinically there has been some controversy regarding the order of interventions with some clinicians advocating the need to address psychological diagnoses first before engaging in cognitive or communication therapies. However, evidence is building for combined approaches addressing emotional/psychological therapies and cognitive/communicative approaches simultaneously and warrants further study (Citation247,Citation251–Citation253). Finally, cognitive-communication skills need to be considered and supported by health professionals in the context of counselling or other psychological interventions (Citation254)
The speech-language pathologist must weigh the operating factors in collaboration with other service providers in order to determine current priorities, the individual’s ability to participate in cognitive-communication intervention, their tolerance for participation in multiple interventions, optimal methods of pacing and prioritizing therapy, positive influences on emotions and behaviours, and methods of maximizing communication success within their rehabilitation and community reintegration settings.
Communication competence is the goal
The model of cognitive-communication competence illustrates that the goal of communication intervention is competence in the following areas of outcome: family communications, community communications, social communications, workplace communications, academic communications and information management, and problem-solving communications. The impact of cognitive-communication impairments on family functioning is well documented including increased communication burden for family members, decreased meaningful engagement in conversation, increased conflict and expression of anger, decreased empathy and consideration for others, and increased reliance on others for decision-making (Citation9,Citation208). These difficulties can undermine the individual’s ability to communicate in their roles as a parent (e.g. provision of advice, encouragement, play, discipline), as a sibling (e.g. perspective taking, conversation, making plans, using tact and diplomacy), or as a spouse (e.g. sharing, discussing, expressing feelings, problem solving, expressing calmly) leading to family stress, marital breakdown, and disintegration of family relationships (Citation9,Citation208,Citation218,Citation250). Communication deficits have also been shown to produce barriers to community independence in areas such as interactive with stores, services, landlords, neighbours, and support personnel (Citation12). In the model these are illustrated as “community communications”. Social communication competence is vital to establishing and maintaining relationships in all contexts and pivotal to successful reintegration at home, community, work, and school (Citation11). Social isolation has also been reported as a frequent consequence of social communication impairments (Citation11,Citation29,Citation142).
Challenges with academically related cognitive-communication functions include problems with understanding course instruction, memory and new learning, reading, integrating, summarizing, completing written assignments, participation in class discussions and presentations, engagement in social communication for group work, peer problem solving, and extracurricular activities, and organization, task management, time management, and self-regulation (Citation15,Citation226,Citation227,Citation255). The needs of students with persisting cognitive-communication difficulties subsequent to ABI are often not identified or accounted for across the developmental and academic continuum where students may be challenged to keep pace with increasing cognitive-communication demands (Citation14,Citation24,Citation227,Citation255). Therefore the term ‘academic communications’ is incorporated in the model of cognitive-communication competence as a key outcome indicator to promote awareness of academic support and achievement as a determining factor in competence.
Communication impairments subsequent to ABI have been shown to be a significant barrier to workplace re-entry and job maintenance (Citation18–Citation20,Citation209,Citation256). Research has identified key communication skills associated with employment success (Citation139,Citation257). Cognitive-communication assessment measures with sufficient sensitivity and ecological validity are able to differentiate individuals with ABI who did and did not successfully return to competitive employment (Citation18–Citation20).
Information management refers to the ability to organize process, recall, and convey information relevant to one’s daily life and includes independent management of health, financial, legal, and household information. Problem-solving communications are depicted as a separate outcome target for cognitive-communication competence in the model. Many individuals with mild or resolving cognitive-communication deficits have persisting difficulties with higher-level reasoning and problem solving despite strengths in other areas of communication functioning. These cognitive-communication challenges in reasoning and problem solving have been demonstrated in a number of studies (Citation19,Citation20,Citation32,Citation33). These deficits often go undetected in clinical settings yet can have significant impact on the individual’s autonomy and family functioning (Citation9).
Focusing on outcomes in these seven key areas of communication competence highlights the importance of using context sensitive, ecologically valid, activity and participation level techniques for assessment, treatment planning, and outcome measurement (Citation11,Citation18,Citation31,Citation216,Citation226). Communication competence relies on the integration, coordination, and regulation of multiple skills for successful participation in multiple contexts (Citation31). It is at this level of dynamic integration of skills within real-life contexts that communication is most likely to be compromised (Citation103,Citation258). Thus the model conveys that the goal of communication intervention is to improve an individual’s success in communicating in the contexts of their daily lives; the goal is communication competence.
How the model of cognitive-communication competence could be applied
Fair and timely access to communication intervention services
The model could be used to promote fair and timely access to communication interventions while reducing barriers that individuals currently face (Citation1,Citation13,Citation36). Fair access to communication interventions requires clear navigation to services in the form of consistent referral criteria, sensitive screening protocols, care pathways, guidelines, and education of referral sources (Citation1,Citation6,Citation13,Citation45). It is hoped that the model could be used to guide development of evidence-based referral tools and pathways and to educate others (i.e. administrators, policymakers, funding sources, referral sources, the general public) to be mindful of the full range of communication impairments and needs.
Evidence-based assessment
The model could promote evidence-based assessment by conveying the multifactorial nature of communication impairment and the need to consider the broad range of cognitive, emotional, physical, and contextual influences on communication. It could guide clinicians to think beyond the employment of a single communication test towards a broader assessment process that includes self-evaluation, clinical observation, real-world evaluation, communication partner evaluation, hypothesis testing, behavioural sampling under a range of conditions, and contributing information from multidisciplinary colleagues (Citation51,Citation52). The model may encourage evaluation beyond impairment level testing to include dynamic interaction with communication partners, analysis of communication demands and environments, and goal setting in the seven areas of communication competence: family, social, community, workplace, academic, information management, and problem solving communications (Citation12,Citation52,Citation139).
Evidence-based treatment
The model of cognitive-communication competence can serve as a coherent framework to guide evidence searches through a range of treatment options while integrating findings from multiple fields of study. It may broaden understanding of the range of interventions available and inspire clinicians to turn to guidelines relevant to a wider range of cognitive and communication interventions. For example, if targeting social communication, the clinician may consider interventions in the domains of communication (discourse planning), cognition (executive functions), context (communication partner training, social networking, peer mentoring), control factors (metacognitive strategy instruction), as well as emotional influences (communication specific coping).
Education, interprofessional collaboration, and research
The model of communication competence could assist in creating shared perspectives across interprofessional and international boundaries. It could promote the importance of communication as an integral part of health service provision and serve as an educational tool for interprofessional collaboration. The model’s central focus on communication could encourage healthcare professionals to consider their role as key communication partners who can support and enhance communication competence in healthcare interactions including those related to goal setting, counselling, discharge planning, decision-making, and academic and vocational re-integration (Citation24,Citation103,Citation134,Citation136,Citation208,Citation250,Citation259). The model could promote an increased focus on measurement of communication health and outcomes which are rarely measured separately, and usually not at the level of activity and participation (Citation1,Citation10,Citation69).
Classification, identification, and tracking of communication deficits
It is hoped that the model of cognitive-communication competence could provide a platform for development of identification and tracking systems to better evaluate the full scope of communication problems across the continuum of care. Currently there is a lack of system-wide understanding of the need for communication intervention and lack of data to drive attention to the problem. Greater specificity of communication impairment is required in large-scale tracking of health outcomes (Citation260–Citation263). The largest incidence study to date examined records of 44 000 US military service members with TBI following blast injury but the national data collection system did not allow for collection of information regarding cognitive-communication disorders (Citation5). Data collection systems should be based on evidence of the full range of communication disorders possible (Citation1,Citation13,Citation36) such as the American Speech and Hearing Association’s National Outcome Measure System (Citation43). Use of such system-wide methods of identifying, classifying, and tracking communication impairments is required in order to determine the range of needs, entry points to the system, staffing allocation, and evaluation of outcomes. The model of cognitive-communication competence could be one such tool to convey the need for data to quantify the vast range of communication impairments, the multifaceted influences on communication competence, and the functional impact of even subtle communication challenges on the quality of life of individuals who experience them.
Limitations
This paper presents initial steps in development of a comprehensive model of communication competence to guide interventions for individuals with ABI. It included expert review with researchers, clinicians, and individuals with brain injury as well as literature search and syntheses. More comprehensive analysis within each of these steps is required with larger samples of clinicians and researchers on the expert teams and more steps to ensure objectivity, diversity, and international input. Additional analysis is required to determine the level of reliability in assigning evidence to each of the categories within the model. Future research will also be necessary to examine the model’s utility in achieving the proposed goals and its effectiveness as an educational tool
Conclusion
The model of cognitive-communication competence was developed to convey the full range of communication impairments, influences on communication, and related interventions, in a comprehensive but accessible manner. It is hoped that the model could have some utility in illustrating the critical role of communication as a determinant of full life participation. The model is proposed as a means of promoting a shared understanding of communication impairment, and defining the ultimate goal of communication competence in real-world functioning. The intervention of cognitive-communication disorders is particularly complex and requires analysis of multiple domains of functioning and multiple influences on performance, in multiple communication contexts. As a result, implementation of evidence-based guidelines has been challenged by the following: inconsistent referral and access to SLP services, assessment measures with insufficient sensitivity and ecological validity, and service constraints to provision of empirically recommended client-centred, contextual, community-based interventions that include communication partners and real-world practice. System-wide organizational change is needed to better serve those with debilitating communication challenges. It will require that we quantify the full range of communication needs, allocate resources accordingly, and seek to apply available practice guidelines for communication intervention. The model of cognitive-communication competence may be one means of structuring evidence synthesis, analyzing communication needs, guiding clinical decision making, and promoting ongoing collaborative research in the field of communication functioning after ABI.
Declaration of interest
The author has financial interest in the company that publishes the Functional Assessment of Verbal Reasoning and Executive Strategies. This measure is referred to in two references and is not the focus of the paper.
Acknowledgments
I would like to thank the members of the Academy of Neurological Communication Disorders Scientific Writing Group for Traumatic Brain Injury for inspired discussion and insightful suggestions for the model: McKay Moore Sohlberg, Therese O’Neil Pirozzi, Bryan Ness, Peter Meulenbroek, Rik Lemoncello, and Lyndsey Byom. I am also grateful to Leanne Togher and Lyn Turkstra whose contributions to the field laid the foundation for the model and whose encouragement inspired further development. Gratitude is also extended to Catherine Wiseman-Hakes who provided additional insights into sleep, fatigue, and social cognition. Great appreciation is also extended to Elyse Shumway, Michelle Cohen, Deirdre Sperry, Leah Davidson, Brenda D’Allessandro, Lisa Jadd, and Joanne Ruediger whose many years of clinical expertise also improved elements of the model. A great debt of gratitude is owed to Arlene Margosian for critical review, edits, and improvements to the paper in preparation. Finally, thanks is extended to the members of Acquired Brain Injury Survivor Solutions who drew on their personal experiences to comment on the model’s utility in conveying the full range of communication challenges and avenues for intervention to improve individual lives.
References
- Blake ML, Frymark T, Venedictov R. An evidence-based systematic review on communication treatments for individuals with right hemisphere brain damage. Am J Speech-Language Pathol. 2013;22(1):146–60. doi:10.1044/1058-0360(2012/12-0021).
- Ferré P, Joanette Y. Communication abilities following right hemisphere damage : prevalence, evaluation, and profiles communication abilities and disabilities : from lateralization to cooperation. Perspectives of the ASHA Special Interest Groups. 2016;1(Part 2):106–15. doi:10.1044/persp1.SIG2.106.
- Sarno MT. The nature of verbal impairment after closed head injury. J Nerv Ment Dis. 1980;166(11):685–92. doi:10.1097/00005053-198011000-00008.
- Halper AS, Cherney LR, Miller TK. Clinical management of communication problems in adults with traumatic brain injury. Gaithersberg, Maryland, USA: Rehabilitation Institute of Chicago publication series. Aspen Publishers; 1991.
- Norman RS, Jaramillo CA, Amuan M, Ma W, Bc E, Mj P. Traumatic brain injury in veterans of the wars in Iraq and Afghanistan: communication disorders stratified by severity of brain injury. Brain Inj. 2013;27(13–14):1623–30. doi:10.3109/02699052.2013.834380.
- King KA, Hough MS, Walker MM, Rastatter M, Holbert D. Mild traumatic brain injury: effects on naming in word retrieval and discourse. Brain Inj. 2006;20(7):725–32. doi:10.1080/02699050600743824.
- Krug H, Turkstra LS. Assessment of cognitive-communication disorders in adults with mild traumatic brain injury. SIG 2 Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders. 2015;25(1):17–35. doi:10.1044/nnsld25.1.17.
- Togher L, Power E, Rietdijk R, McDonald S, Tate R. An exploration of participant experience of a communication training program for people with traumatic brain injury and their communication partners. Disabil Rehabil. 2012;34(18):1562–74. doi:10.3109/09638288.2012.656788.
- Knox L, Douglas JM, Bigby C. “The biggest thing is trying to live for two people”: spousal experiences of supporting decision-making participation for partners with TBI. Brain Inj. 2015;29(6):745–57. doi:10.3109/02699052.2015.1004753.
- Finch E, Copley A, Cornwell P, Kelly C. Systematic review of behavioral interventions targeting social communication difficulties after traumatic brain injury. Arch Phys Med Rehabil. 2016;97(8):1352–65. doi:10.1016/j.apmr.2015.11.005.
- Struchen MA, Pappadis MR, Sander AM, Burrows CS, Myszka KA. Examining the contribution of social communication abilities and affective/behavioral functioning to social integration outcomes for adults with traumatic brain injury. J Head Trauma Rehabil. 2011;26(1):30–42. doi:10.1097/HTR.0b013e3182048f7c.
- Togher L, McDonald S, Code C, Grant S. Training communication partners of people with traumatic brain injury: A randomised controlled trial. Aphasiology. 2004;18(4):313–35. doi:10.1080/02687030344000535.
- Turkstra LS, Politis AM, Forsyth R. Cognitive-communication disorders in children with traumatic brain injury. Dev Med Child Neurol. 2015;57(3):217–22. doi:10.1111/dmcn.12600.
- Ciccia AH, Meulenbroek P, Turkstra LS. Adolescent brain and cognitive developments. Top Lang Disord. 2009;29(3):249–65. doi:10.1097/TLD.0b013e3181b53211.
- Kennedy MRT, Krause MO, Turkstra LS. An electronic survey about college experiences after traumatic brain injury. Neurorehabilitation. 2008;23(6):511–20.
- Krause M, Byom L, Meulenbroek P, Richards S, O’Brien K. Supporting the literacy skills of adolescents with traumatic brain injury. Semin Speech Lang. 2015;36(1):60–73. doi:10.1055/s-0034-1396447.
- Griffiths GG, Sohlberg MM, Kirk C, Fickas S, Biancarosa G. Evaluation of use of reading comprehension strategies to improve reading comprehension of adult college students with acquired brain injury. Neuropsychol Rehabil. 2016;26(2):161–90. doi:10.1080/09602011.2015.1007878.
- Douglas JM, Bracy CA, Snow PC. Return to work and social communication ability following severe traumatic brain injury. J Speech Lang Hearing Res. 2016;59(3):511. doi:10.1044/2015_JSLHR-L-15-0025.
- Rietdijk R, Simpson G, Togher L, Power E, Gillett L. An exploratory prospective study of the association between communication skills and employment outcomes after severe traumatic brain injury. Brain Inj. 2013;27(7–8):812–18. doi:10.3109/02699052.2013.775491.
- Meulenbroek P, Turkstra LS. Job stability in skilled work and communication ability after moderate–severe traumatic brain injury. Disabil Rehabil. 2015;38(5):452–61. doi:10.3109/09638288.2015.1044621.
- Togher L, McDonald S, Code C. Social communication disorders after TBI. In: McDonald S, Togher L, Code C, editor. Social communication disorders following traumatic brain injury. Psychology Press, 2nd ed, Taylor &Francis Group, Hove, East Sussex, UK; 2014. p. 1–25.
- Cicerone KD, Langenbahn DM, Braden C, Malec JF, Kalmar K, Fraas M, Felicetti T, Laatsch L, Harley JP, Bergquist T, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch Phys Med Rehabil. 2011;92(4):519–30. doi:10.1016/j.apmr.2010.11.015.
- MacDonald S, Wiseman-Hakes C. Knowledge translation in ABI rehabilitation: A model for consolidating and applying the evidence for cognitive-communication interventions. Brain Inj. 2010;24(3):486–508. doi:10.3109/02699050903518118.
- Togher L, Wiseman-Hakes C, Douglas J, Stergiou-Kita M, Ponsford J, Teasell R, Bayley M, Turkstra LS. INCOG recommendations for management of cognition following traumatic brain injury, part IV: cognitive communication. J Head Trauma Rehabil. 2014;29(4):353–68. doi:10.1097/HTR.0000000000000071.
- Cherney LR, Gardner P, Logemann JA, Newman LA, Neil-Pirozzi TO, Roth CR, Solomon NP. The role of speech-language pathology and audiology in the optimal management of the service member returning From Iraq or Afghanistan with a blast-related head injury : position of the communication sciences and disorders clinical trials research group. J Head Trauma Rehabil. 2010;25(3):219–24. doi:10.1097/HTR.0b013e3181dc82c1.
- Sohlberg MM, Avery J, Kennedy M, Ylvisaker M, Coelho C, Turkstra L, Yorkston K. Practice guidelines for direct attention training. J Med Speech Lang Pathol. 2003;11(3):xix–xxxix.
- OʼNeil-Pirozzi TM, Kennedy M, Sohlberg MM. Evidence based practice for the use of internal strategies as a memory compensation technique after brain injury: A systematic review. J Head Trauma Rehabil. 2015;31(4):E1–E11. doi:10.1097/HTR.0000000000000181.
- Sohlberg MM, Kennedy M, Avery J, Coelho C, Turkstra L, Ylvisaker M, Yorkston K. Evidence-based practice for the use of external aids as a memory compensation technique. J Med Speech Lang Pathol. 2007;15(1):xv–li.
- Ylvisaker M, Turkstra L, Coehlo C, Yorkston K, Kennedy M, Sohlberg MM, Avery J. Behavioural interventions for children and adults with behaviour disorders after TBI: a systematic review of the evidence. Brain Inj. 2007;21(8):769–805. doi:10.1080/02699050701482470.
- Watter K, Copley A, Finch E. Treating reading comprehension deficits in sub-acute brain injury rehabilitation: identifying clinical practice and management. J Commun Disord. 2016;64:110–32. doi:10.1016/j.jcomdis.2016.07.006.
- Kennedy MRT, Coelho C, Turkstra L, Ylvisaker M, Moore Sohlberg M, Yorkston K, Chiou -H-H, Kan P-F. Intervention for executive functions after traumatic brain injury: A systematic review, meta-analysis and clinical recommendations. Neuropsychol Rehabil. 2008;18(3):257–99. doi:10.1080/09602010701748644.
- MacDonald S, Johnson CJ. Assessment of subtle cognitive-communication deficits following acquired brain injury: A normative study of the Functional Assessment of Verbal Reasoning and Executive Strategies (FAVRES). Brain Inj. 2005;19(11):895–902. doi:10.1080/02699050400004294.
- MacDonald S. Assessment of higher level cognitive-communication functions in adolescents with ABI: standardization of the student version of the functional assessment of verbal reasoning and executive strategies (S-FAVRES). Brain Inj. 2016;30(3):295–310. doi:10.3109/02699052.2015.1091947.
- Kennedy MRT, O’Brien KH, Krause MO. Bridging person-centred outcomes and therapeutic processes for college students with traumatic brain injury. Perspect Neurophysiol Neurogenic Speech Lang Disord. 2012:143–51. doi:10.1044/nnsld22.4.143.
- Steel J, Ferguson A, Spencer E, Togher L. Language and cognitive communication during post-traumatic amnesia: A critical synthesis. NeuroRehabilitation. 2015;37(2):221–34. doi:10.3233/NRE-151255.
- Hinckley JJ. A case for the implementation of cognitive-communication screenings in acute stroke. Am J Speech-Language Pathol. 2014;23(1):4–14. doi:10.1044/1058-0360(2013/11-0064).
- Leblanc J, De Guise E, Feyz M, Lamourreux J. Early prediction of language impairment following traumatic brain injury. Brain Inj. 2006;20(13–14):1391–401. doi:10.1080/02699050601081927.
- Brunner M, Skeat J, Morris ME. Outcomes of speech-language pathology following stroke: investigation of inpatient rehabilitation and rehabilitation in the home programs. Int J Speech Lang Pathol. 2008;10(5):305–13. doi:10.1080/17549500802027392.
- Parrish C, Roth C, Roberts B, Davie G. Assessment of cognitive-communicative disorders of mild traumatic brain injury sustained in combat. Perspect Neurophysiol Neurogenic Speech Lang Disord. 2009;19(2):47–57. doi:10.1044/nnsld19.2.47.
- Tompkins CA. Rehabilitation for cognitive-communication disorders in right hemisphere brain damage. Arch Phys Med Rehabil. 2012;93(1 SUPPL.):S61–S69. doi:10.1016/j.apmr.2011.10.015.
- Dahlberg CA, Cusick CP, Hawley LA, Newman JK, Morey CE, Harrison-Felix CL, Whiteneck GG. Treatment efficacy of social communication skills training after traumatic brain injury: a randomized treatment and deferred treatment controlled trial. Arch Phys Med Rehabil. 2007;88(12):1561–73. doi:10.1016/j.apmr.2007.07.033.
- Edwards DF, Hahn MG, Baum CM, Perlmutter MS, Sheedy C, Dromerick AW. Screening patients with stroke for rehabilitation needs: validation of the post-stroke rehabilitation guidelines. Neurorehabil Neural Repair. 2006;20(1):42–48. doi:10.1177/1545968305283038.
- American Speech-Language-Hearing Association. Adults in Healthcare Outpatient National Data Report. 2011 [accessed 2016 Oct 6]. www.asha.org › NOMS.
- Salter K, McClure JA, Mahon H, Foley N, Teasell R. Adherence to Canadian best practice recommendations for stroke care: assessment and management of poststroke depression in an Ontario rehabilitation facility. Top Stroke Rehabil. 2012;19(2):132–40. doi:10.1310/tsr1902-132.
- Morgan AT, Skeat J. Evaluating service delivery for speech and swallowing problems following paediatric brain injury: an international survey. J Eval Clin Pract. 2011;17(2):275–81. doi:10.1111/jep.2011.17.issue-2.
- Sullivan A, Cleave PL. Knowledge of the roles of speech-language pathologists by students in other health care programs. J Speech Lang Pathol Audiol. 2003;27(2):98–107.
- Sl S, Cn W, Kothari A, Amb D. Knowledge flow and exchange in interdisciplinary primary health care teams (PHCTs): an exploratory study. J Med Lib Assoc. 2013;101(2):128–37. doi:10.3163/1536-5050.101.2.008.
- Sainson C, Barat M, Aguert M. Communication disorders and executive function impairment after severe traumatic brain injury: an exploratory study using the GALI (a grid for linguistic analysis of free conversational interchange). Ann Phys Rehabil Med. 2014;57(9–10):664–83. doi:10.1016/j.rehab.2014.08.011.
- Rousseaux M, Vérigneaux C, Kozlowski O. An analysis of communication in conversation after severe traumatic brain injury. Eur J Neurol. 2010;17(7):922–29. doi:10.1111/j.1468-1331.2009.02945.x.
- Douglas JM. Using the La Trobe communication questionnaire to measure perceived social communication ability in adolescents with traumatic brain injury. Brain Imp. 2010;11(2):171–82. doi:10.1375/brim.11.2.171.
- Turkstra LS, Coelho C, Ylvisaker M. The use of standardized tests for individuals with cognitive-communication disorders. Semin Speech Lang. 2005;26(4):215–22. doi:10.1055/s-2005-922101.
- Coelho C, Ylvisaker M, Turkstra LS. Nonstandardized assessment approaches for individuals with traumatic brain injuries. Semin Speech Lang. 2005;26(4):223–41. doi:10.1055/s-2005-922102.
- Togher L. Discourse sampling in the 21st century. J Commun Disord. 2001;34:131–50. doi:10.1016/S0021-9924(00)00045-9.
- Barwood CHS, Murdoch BE. Unravelling the influence of mild traumatic brain injury (MTBI) on cognitive-linguistic processing: A comparative group analysis. Brain Inj. 2013;27(6):671–76. doi:10.3109/02699052.2013.775500.
- Blyth T, Scott A, Bond A, Paul E. A comparison of two assessments of high level cognitive communication disorders in mild traumatic brain injury. Brain Inj. 2012;26(3):234–40. doi:10.3109/02699052.2012.654587.
- Foster A, Worrall L, Rose M, O’Halloran R. “That doesn”t translate’: the role of evidence-based practice in disempowering speech pathologists in acute aphasia management. I J Lang Communication disorders/Royal College Speech Language Therapists. 2015:1–17.
- Frith M, Togher L, Ferguson A, Levick W, Docking K. Assessment practices of speech-language pathologists for cognitive communication disorders following traumatic brain injury in adults: an international survey. Brain Inj. 2014;28(May 2016):1362–301. doi:10.3109/02699052.2014.947619.
- Coelho C, Lê K, Mozeiko J, Krueger F, Grafman J. Discourse production following injury to the dorsolateral prefrontal cortex. Neuropsychologia. 2012;50(14):3564–72. doi:10.1016/j.neuropsychologia.2012.09.005.
- LeBlanc J, De Guise E, Champoux M-C, Couturier C, Lamoureux J, Marcoux J, Maleki M, Feyz M. Acute evaluation of conversational discourse skills in traumatic brain injury. Int J Speech Lang Pathol. 2014;16(6):582–93. doi:10.3109/17549507.2013.871335.
- Tse T, Douglas J, Lentin P, Carey L. Measuring participation after stroke: A review of frequently used tools. Arch Phys Med Rehabil. 2013;94(1):177–92. doi:10.1016/j.apmr.2012.09.002.
- Hughes J, Orange JB. Mapping functional communication measurements for traumatic brain injury to the WHO-ICF. Can J Speech-Language Pathol Audiol. 2007;31(3):134–43.
- Avrimovik P, Togher L, Kenny B, Power E, McDonald S, Tate R, Hunt L, Macdonald S, Heard R. Exploring relationships between cognition and functional verbal reasoning in adults with severe traumatic brain injury at six months post injury. Brain Inj. 2017;31(4):502–16. doi:10.1080/02699052.2017.1280854.
- Hadely KA, Power E, O’Halloran R. Speech pathologists’ experiences with stroke clinical practice guidelines and the barriers and facilitators influencing their use: a national descriptive study. BMC Health Serv Res. 2014;14(1):110. doi:10.1186/1472-6963-14-110.
- Elbourn E, Togher L, Kenny B, Power E. Strengthening the quality of longitudinal research into cognitive-communication recovery after traumatic brain injury: A systematic review. Int J Speech Lang Pathol. 2017;19(1):1–16. doi:10.1080/17549507.2016.1193896.
- Tate R, Kennedy M, Ponsford J, Douglas J, Velikonja D, Bayley M, Stergiou-Kita M. INCOG recommendations for management of cognition following traumatic brain injury, part III: executive function and self-awareness. J Head Trauma Rehabil. 2014;29(4):338–52. doi:10.1097/HTR.0000000000000068.
- Kleinow J. Theory-based practice : a case study of the multifactorial model of stuttering multifactorial model. SIG 4 Perspectives on Fluency and Fluency Disorders. 2016;25(May 2015):33–38. doi:10.1044/ffd25.1.33.
- American, Speech-, Language-Hearing, Association. Roles of speech-language pathologists in the identification, diagnosis, and treatment of individuals with cognitive-communication disorders: position statement. 2005. Available from www.asha.org/policy.
- CASLPO. Practice standards and guidelines for acquired cognitive communication disorders. 2015 Available from http://www.caslpo.com/sites/default/uploads/files/PSG_EN_Acquired_Cognitive_Communication_Disorders.pdf.
- Watter K, Copley A, Finch E. Discourse level reading comprehension interventions following acquired brain injury: a systematic review. Disabil Rehabil. 2016;8288(February).
- Kennedy MRT, Coelho C, Turkstra L, Ylviasker M, Sohlberg MM, Yorkston K, Chiou HH, Kan P-F. Intervention for executive functions after traumatic brain injury: A systematic review, meta-analysis and clinical recommendations. Neuropsychol Rehabil. 2008;18(3):257–99. doi:10.1080/09602010701748644.
- Ehlhardt LA, Sohlberg MM, Kennedy M, Coelho C, Ylvisaker M, Turkstra L, Yorkston K. Evidence-based practice guidelines for instructing individuals with neurogenic memory impairments: what have we learned in the past 20 years? Neuropsychol Rehabil. 2008;18(March 2015):300–42. doi:10.1080/09602010701733190.
- Togher L, Power E, Tate R, McDonald S, Rietdijk R. Measuring the social interactions of people with traumatic brain injury and their communication partners: the adapted Kagan scales. Aphasiology. 2010;24(6–8):914–27. doi:10.1080/02687030903422478.
- Turkstra L, Clark A, Burgess S, Hengst J. Pragmatic communication abilities in children and adults: implications for rehabilitation professionals. Disabil Rehabil. 2016;0(0):1464–5165.
- Cook LG, Chapman SB, Elliott AC, Evenson NN, Vinton K. Cognitive gains from gist reasoning training in adolescents with chronic-stage traumatic brain injury. Front Neurol. 2014;5(June):1–9. doi:10.3389/fneur.2014.00087.
- Kennedy MRT, Coelho C. Self-regulation after traumatic brain injury: a framework for intervention of memory and problem solving. Semin Speech Lang. 2005;26(4):242–55. doi:10.1055/s-2005-922103.
- McDonald S., Gowland A., Randall R., Fisher, A., Osborne-Crowley, K., & Honan, C. (2014). Cognitive factors underpinning poor expressive communication skills after traumatic brain injury: Theory of mind or executive function? Neuropsychology, 28(5)801–811.
- McDonald S, Gowland A, Randall R, Fisher A, Osborne-Crowley K, Honan C. Cognitive factors underpinning poor expressive communication skills after traumatic brain injury: theory of mind or executive function?. Neuropsychology. 2014;(5):No–Specified. online ahe.
- Chapman SB, Gamino JF, Cook LG, Hanten G, Li X, Levin HS. Impaired discourse gist and working memory in children after brain injury. Brain Lang. 2006;97(2):178–88. doi:10.1016/j.bandl.2005.10.002.
- Turkstra LS. Conversation-based assessment of social cognition in adults with traumatic brain injury. Brain Inj. 2008;22(5):397–409. doi:10.1080/02699050802027059.
- Henriques GR. Evolving from methodological to conceptual unification. Rev Gen Psychol. 2013;17(2):168–73. doi:10.1037/a0032929.
- WHO. The International Classification of Functioning, Disability and Health. World Health Organization. 2001;18:237.
- Larkins B, Worrall L, Hickson L. Developing a traumatic brain injury index for social and vocational communication outcomes (SAVCO). Brain Imp. 2008;9(3):247–66. doi:10.1375/brim.9.3.247.
- Galajda D. Communicative competence. In: Communicative behaviour of a language learner, second language learning and teaching. Champlain, MI: Springer International Publishing AG, Champlain, Michigan, USA; 2017. p. 19–26.
- Hartley LL. Cognitive-communicative abilities following brain injury: A functional approach. San Diego: Singular Publishing; 1995.
- Tsai M-J. Rethinking communicative competence for typical speakers: an integrated approach to its nature and assessment. Pragmatics Cogn. 2013;21(1):158–77. doi:10.1075/pc.21.1.
- Light J. Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augmentative Altern Commun. 2009;5(2):137–44. doi:10.1080/07434618912331275126.
- Larkins B. The application of the ICF in cognitive-communication disorders following traumatic brain injury. Semin Speech Lang. 2007;28(212):334–42. doi:10.1055/s-2007-986530.
- Ylvisaker M, Turkstra LS, Coelho C. Behavioral and social interventions for individuals with traumatic brain injury: A summary of the research with clinical implications. Semin Speech Lang. 2005;26(4):256–67. doi:10.1055/s-2005-922104.
- Coelho C, Lê K, Mozeiko J, Hamilton M, Tyler E, Krueger F, Grafman J. Characterizing discourse deficits following penetrating head injury: A preliminary model. Am J Speech-Language Pathol. 2013;22(May):438–49. doi:10.1044/1058-0360(2013/12-0076).
- Fitzgerald A, Aditya H, Prior A, McNeill E, Pentland B. Anoxic brain injury: clinical patterns and functional outcomes. A study of 93 cases. Brain Inj. 2010;24(11):1311–23. doi:10.3109/02699052.2010.506864.
- Langenbahn DM, Ashman T, Cantor J, Trott C. An evidence-based review of cognitive rehabilitation in medical conditions affecting cognitive function. Arch Phys Med Rehabil. 2013;94(2):271–86. doi:10.1016/j.apmr.2012.09.011.
- Cohen M, Ylvisaker M, Hamilton J, Kemp L, Claiman B. Errorless learning of functional life skills in an individual with three aetiologies of severe memory and executive function impairment. Neuropsychol Rehabil. 2010;20(3):355–76. doi:10.1080/09602010903309401.
- Ferré P, Ska B, Lajoie C, Bleau A, Joanette Y. Clinical focus on prosodic, discursive and pragmatic treatment for right hemisphere damaged adults: what’s right? Rehabilitation Research and Practice; 2011. p. 1–10. http://www.hindawi.com/journals/rerp/2011/131820/.
- Blake ML. Inferencing processes after right hemisphere brain damage: maintenance of inferences. J Speech Lang Hear Res. 2009;52(2):359–72. doi:10.1044/1092-4388(2009/07-0012).
- Lehman Blake M. Clinical relevance of discourse characteristics after right hemisphere brain damage. A J Speech-Lang Pathol. 2006;15(3):255–67. doi:10.1044/1058-0360(2006/024).
- Côté H, Payer M, Giroux F, Joanette Y. Towards a description of clinical communication impairment profiles following right‐hemisphere damage. Aphasiology. 2007;21(6–8):739–49. doi:10.1080/02687030701192331.
- Scottish Intercollegiate Guidelines Network. Brain injury rehabilitation in adults. Scottish Intercollegiate Guidelines network. 2013 March; 1–75. Available from http://www.sign.ac.uk/assets/sign130.pdf.
- New Zealand, Guidelines, Group. Traumatic brain injury: diagnosis, acute management and rehabilitation. 2007. Available from http://www.nzgg.org.nz.
- Olver JH, Ponsford JL, Curran CA. Outcome following traumatic brain injury: A comparison between 2 and 5 years after injury. Brain Inj. 1996;10(11):841–48. doi:10.1080/026990596123945.
- McKinlay WW, Brooks DN, Bond MR, Martinage DP, Marshall MM. The short-term outcome of severe blunt head injury as reported by relatives of the injured persons. J Neurol Neurosurg Psychiatry. 1981;44(6):527–33. doi:10.1136/jnnp.44.6.527.
- Snow P. Communication competence following TBI: assessment and management. In: Ponsford J, Sloan S, Snow P, editor. Traumatic brain injury rehabilitation for everyday adaptive living. 2nd ed. New York: Psychology press, Taylor Francis Group; 2013.
- Chapman SB, McKinnon L, Levin HS, Song J, Meier MC, Chiu S. Longitudinal outcome of verbal discourse in children with traumatic brain injury: three-year follow-up. 2001:16(5);441–55.
- Beauchamp MH, Anderson V. SOCIAL: an integrative framework for the development of social skills. Psychol Bull. 2010;136(1):39–64. doi:10.1037/a0017768.
- Yeates KO, Bigler ED, Dennis M, Gerhardt CA, Kh R, Stancin T, Hg T. Social oucomes in childhood brain disorder: a heuristic integration of social neuroscience and developmental psychology. Psychol Bull. 2007;133(3):535–56. doi:10.1037/0033-2909.133.3.535.
- Martin I, McDonald S. Weak coherence, no theory of mind, or executive dysfunction? Solving the puzzle of pragmatic language disorders. Brain Lang. 2003;85(3):451–66. doi:10.1016/S0093-934X(03)00070-1.
- Cassel A, McDonald S, Kelly M, Togher L. Learning from the minds of others: A review of social cognition treatments and their relevance to traumatic brain injury. Neuropsychol Rehabil. 2016;1–34. doi:10.1080/09602011.2016.1257435. Published.
- Lundgren K., Helm-Estabrooks N., & Klein R. (2010). Stuttering following acquired brain damage: A review of the literature. Journal of Neurolinguistics, 23(5), 447–454. http://doi.org/10.1016/j.jneuroling.2009.08.008.
- Johnson-Laird PN, Byrne RMJ. Conditionals: A theory of meaning, pragmatics, and inference. Psychol Rev. 2002;109(4):646–78. doi:10.1037/0033-295X.109.4.646.
- Baddeley A. The fractionation of working memory. Proc Natl Acad Sci U S A. 1996;93(24):13468–72. doi:10.1073/pnas.93.24.13468.
- Stuss DT. Functions of the frontal lobes: relation to executive functions. J Int Neuropsychological Soc. 2011;17(5):759–65. doi:10.1017/S1355617711000695.
- American Speech-Language Hearing Association (ASHA). Evidence maps. Available from http://www.asha.org/Evidence-Maps/
- SpeechBITE. Available from Http://www.speechbite.com.
- PsycBITE. Available from Http://www.psycbite.com.
- Ryan NP, Catroppa C, Beare R, Coleman L, Ditchfield M, Crossley L, Beauchamp MH, Anderson VA. Predictors of longitudinal outcome and recovery of pragmatic language and its relation to externalizing behaviour after pediatric traumatic brain injury. Brain Lang. 2015;142:86–95. doi:10.1016/j.bandl.2015.01.007.
- Chapman SB, McKinnon L. Discussion of developmental plasticity: factors affecting cognitive outcome after pediatric traumatic brain injury. J Commun Disord. 2000;33(4):333–44. doi:10.1016/S0021-9924(00)00029-0.
- Crowe LM, Catroppa C, Babl FE, Rosenfeld JV, Anderson V. Timing of traumatic brain injury in childhood and intellectual outcome. J Pediatr Psychol. 2012;37(7):745–54. doi:10.1093/jpepsy/jss070.
- Kolb B, Pellis S, Robinson TE. Plasticity and functions of the orbital frontal cortex. Brain Cogn. 2004;55(1):104–15. doi:10.1016/S0278-2626(03)00278-1.
- Carman A. J., Ferguson R., Cantu R., Comstock R. D., Dacks P. A, DeKosky S. T., … Fillit H. M. (2015). Expert consensus document: Mind the gaps-advancing research into short-term and long-term neuropsychological outcomes of youth sports-related concussions. Nature Reviews. Neurology, 11(4), 230–244. http://doi.org/10.1038/nrneurol.2015.30
- Rigon A, Turkstra L, Mutlu B, Duff M. The female advantage: sex as a possible protective factor against emotion recognition impairment following traumatic brain injury. Cognitive, Affective, Behav Neurosci. 2016;16(5):866–75. doi:10.3758/s13415-016-0437-0.
- Despins EH, Turkstra LS, Struchen MA, Clark AN. Sex-based differences in perceived pragmatic communication ability of adults with traumatic brain injury. Arch Phys Med Rehabil. 2016;97(2):S26–S32. doi:10.1016/j.apmr.2014.06.023.
- Ruff RM, Iverson GL, Barth JT, Bush SS, Broshek DK. Recommendations for diagnosing a mild traumatic brain injury: a national academy of neuropsychology education paper. Arch Clin Neuropsychol. 2009;24(1):3–10. doi:10.1093/arclin/acp006. [accessed 2013 Apr 12].
- Iverson GL, Schatz P. Advanced topics in neuropsychological assessment following sport-related concussion. Brain Inj. 2014;29(2):263–75. doi:10.3109/02699052.2014.965214.
- McCrory P, Meeuwisse WH, Aubry M, Cantu RC, Dvorák J, Echemendia RJ, Engebretsen L, Johnston KM, Kutcher JS, Raftery M, et al. Consensus statement on concussin in sport: the 4th international conference on concussion in sport. PM and R. 2013;5(4):255–79. doi:10.1016/j.pmrj.2013.02.012. Zurich, Switzerland.
- De Guise E, LeBlanc J, Dagher J, Tinawi S, Lamoureux J, Marcoux J, Maleki M, Feyz M. Characteristics of patients with acute traumatic brain injury discharged against medical advice in a Level 1 urban trauma centre. Brain Inj. 2014;28(10):1288–94. doi:10.3109/02699052.2014.916820.
- Cooper JM, Catroppa C, Beauchamp MH, Eren S, Godfrey C, Ditchfield M, Anderson VA. Attentional control ten years post childhood traumatic brain injury: the impact of lesion presence, location, and severity in adolescence and early adulthood. J Neurotrauma. 2014;31(8):713–21. doi:10.1089/neu.2013.3101.
- Rosema S, Crowe L, Anderson V. Social function in children and adolescents after traumatic brain injury: a systematic review 1989-2011. J Neurotrauma. 2012;29(7):1277–91. doi:10.1089/neu.2011.2144.
- Mollayeva T, Shapiro CM, Mollayeva S, Cassidy JD, Colantonio A. Modeling community integration in workers with delayed recovery from mild traumatic brain injury. BMC Neurol. 2015;15(1):194. doi:10.1186/s12883-015-0432-z.
- Belanger HG, Curtiss G, Demery JA, Bk L, Rd V. Factors moderating neuropsychological outcomes following mild traumatic brain injury: a meta-analysis. J Int Neuropsychological Soc. 2005;11(3):215–27. doi:10.1017/S1355617705050277.
- Luis CA, Vanderploeg RD, Curtiss G. Predictors of postconcussion symptom complex in community dwelling male veterans. J Int Neuropsychological Soc. 2003;9(7):1001–15. doi:10.1017/S1355617703970044.
- Shames J, Treger I, Ring H, Giaquinto S. Return to work following traumatic brain injury: trends and challenges. Disabil Rehabil. 2007;29(17):1387–95. doi:10.1080/09638280701315011.
- Tu LV, Togher L, Power E. The impact of communication partner and discourse task on a person with traumatic brain injury: the use of multiple perspectives. Brain Inj. 2011;25(6):560–80. doi:10.3109/02699052.2011.571655.
- Jorgensen M, Togher L. Narrative after traumatic brain injury: a comparison of monologic and jointly-produced discourse. Brain Inj. 2009;23(9):727–40. doi:10.1080/02699050903133954.
- Mann K, Power E, Barnes S, McDonald S, Tate R, Togher L. “Questioning in conversations before and after communication partner training for individuals with traumatic brain injury”: corrigendum. Aphasiology. 2015;29(7):1082–109. doi:10.1080/02687038.2015.1035226.
- Behn N, Togher L, Power E, Heard R. Evaluating communication training for paid carers of people with traumatic brain injury. Brain Inj. 2012;26(13–14):1702–15. doi:10.3109/02699052.2012.722258.
- Eriksson K, Hartelius L, Saldert C. Participant characteristics and observed support in conversations involving people with communication disorders. Int J Speech Lang Pathol. 2016;18(5):439–49. doi:10.3109/17549507.2015.1126642.
- Shelton C, Shryock M. Effectiveness of communication/interaction strategies with patients who have neurological injuries in a rehabilitation setting. Brain Inj. 2007;21(12):1259–66. doi:10.1080/02699050701716935.
- Byom LJ, Turkstra L. Effects of social cognitive demand on Theory of Mind in conversations of adults with traumatic brain injury. Int J Lang Commun Disord. 2012;47(3):310–21. doi:10.1111/j.1460-6984.2011.00102.x.
- Honan CA, McDonald S, Gowland A, Fisher A, Randall RK. Deficits in comprehension of speech acts after TBI: the role of theory of mind and executive function. Brain Lang. 2015;150(SEPTEMBER):69–79. doi:10.1016/j.bandl.2015.08.007.
- Larkins BM, Worrall LE, Hickson LM. Stakeholder opinion of functional communication activities following traumatic brain injury. Brain Inj. 2004;18(7):691–706. doi:10.1080/02699050310001617389.
- Shelton C., & Shryock M. (2007) Effectiveness of communication/ interaction strategies with patients who have neurological injuries in a rehabilitation setting. Brain Injury, 21(12):1259–66. http://doi.org/10.1080/02699050701716935.
- McDonald S, Tate R, Togher L, Bornhofen C, Long E, Gertler P, Bowen R. Social skills treatment for people with severe, chronic acquired brain injuries: a multicenter trial. Arch Phys Med Rehabil. 2008;89(9):1648–59. doi:10.1016/j.apmr.2008.02.029.
- Douglas J. Elizabeth Usher Memorial Lecture: placing therapy in the context of the self and social connection. Int J Speech Lang Pathol. 2015;17(3):199–210. doi:10.3109/17549507.2015.1016113.
- Struchen MA, Clark AN, Sander AM, Mills MR, Evans G, Kurtz D. Relation of executive functioning and social communication measures to functional outcomes following traumatic brain injury. NeuroRehabilitation. 2008;23(2):185–98.
- Association of Speech-Language Pathology and Audiology ASHA. Rehabilitation of children and adults with cognitive-communication disorders after brain injury. 2003;1–31. Available from http://www.asha.org/policy/TR2003-00146/.
- Levin HS, Hanten G. Executive functions after traumatic brain injury in children. Pediatr Neurol. 2005;33(2):79–93. doi:10.1016/j.pediatrneurol.2005.02.002.
- Cicerone K, Levin H, Malec J, Stuss D, Whyte J. Cognitive rehabilitation interventions for executive function: moving from bench to bedside in patients with traumatic brain injury. J Cogn Neurosci. 2006;18(7):1212–22. doi:10.1162/jocn.2006.18.7.1212.
- Douglas JM, Bracy CA, Snow PC. Measuring perceived communicative ability after traumatic brain injury: reliability and validity of the La Trobe Communication Questionnaire. J Head Trauma Rehabil. 2007;22(1):31–38. doi:10.1097/00001199-200701000-00004.
- Levine B, Schweizer TA, O’Connor C, Turner G, Gillingham S, Stuss DT, Manly T, Robertson IH. Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Front Hum Neurosci. 2011;5(February):1–9. doi:10.3389/fnhum.2011.00009.
- Anderson VA, Anderson P, Northam E, Jacobs R, Catroppa C. Development of executive functions through late childhood and adolescence in an Australian sample. Dev Neuropsychol. 2001;20(1):385–406. doi:10.1207/S15326942DN2001_5.
- Copley A, Smith K, Savill K, Finch E. Does metacognitive strategy instruction improve impaired receptive cognitive-communication skills following acquired brain injury? Brain Inj. 2015;29(11):1309–16. doi:10.3109/02699052.2015.1043343.
- Kennedy MRT, Coelho C, Turkstra L, Sohlberg MM, Yorkston K, Chiou -H-H, Kan P-F. Intervention for executive functions after traumatic brain injury : A systematic review, meta-analysis and clinical recommendations. Neuropsychol Rehabil. 2008;18(3):257–99. doi:10.1080/09602010701748644.
- Pearce B, Cartwright J, Cocks N, Whitworth A. Inhibitory control and traumatic brain injury: the association between executive control processes and social communication deficits. Brain Inj. 2016;30(13–14):1708–17. doi:10.1080/02699052.2016.1202450.
- Rassovsky Y, Satz P, Alfano MS, Light RK, Zaucha K, McArthur DL, Hovda D. Functional Outcome in TBI II: verbal memory and information processing speed mediators. J Clin Exp Neuropsychol. 2006;28(4):581–91. doi:10.1080/13803390500434474.
- Sohlberg MM, Griffiths GG, Fickas S. Reading comprehension of expository text in adults with traumatic brain injury. Am J Speech-Language Pathol. 2014;23(2):160–75. doi:10.1044/2013_AJSLP-12-0005.
- McDonald S, Fisher A, Flanagan S. When diplomacy fails: difficulty understanding hints following severe traumatic brain injury. Aphasiology. 2016;30(7):801–14. doi:10.1080/02687038.2015.1070948.
- Wiseman-Hakes C, Murray B, Moineddin R, Rochon E, Cullen N, Gargaro J, Colantonio A. Evaluating the impact of treatment for sleep/wake disorders on recovery of cognition and communication in adults with chronic TBI. Brain Inj. 2013;27(12):1364–76. doi:10.3109/02699052.2013.823663.
- Nicholas LE, Brookshire RH. Comprehension of spoken narrative discourse by adults with aphasia, right-hemisphere brain damage, or traumatic brain injury. Am J Speech-Language Pathol. 1995;4(3):69–81. doi:10.1044/1058-0360.0403.69.
- Evans K, Hux K. Comprehension of indirect requests by adults with severe traumatic brain injury: contributions of gestural and verbal information. Brain Inj. 2011;25(7–8):767–76. doi:10.3109/02699052.2011.576307.
- Peach RK. The cognitive basis for sentence planning difficulties in discourse after traumatic brain injury. Brain Inj. 2013;22(May):285–98.
- Galbiati S, Recla M, Pastore V, Liscio M, Bardoni A, Castelli E, Strazzer S. Attention remediation following traumatic brain injury in childhood and adolescence. Neuropsychology. 2009;23(1):40–49. doi:10.1037/a0013409.
- Butler RW, Copeland DR, Fairclough DL, Mulhern RK, Katz ER, Kazak AE, Noll RB, Patel SK, Sahler OJZ. A multicenter, randomized clinical trial of a cognitive remediation program for childhood survivors of a pediatric malignancy. J Consult Clin Psychol. 2008;76(3):367–78. doi:10.1037/0022-006X.76.3.367.
- Jaime L, Beth H, McKay Moore S, Sl W. An overview of the Attention Improvement Management (aim) program with outcomes for three pilot participants. Perspect Neurophysiol Neurogenic Speech Lang Disord. 2012;22(3):90–105. doi:10.1044/nnsld22.3.90.
- Chen AJW, Novakovic-Agopian T, Nycum TJ, Song S, Turner GR, Hills NK, Rome S, Abrams GM, D’Esposito M. Training of goal-directed attention regulation enhances control over neural processing for individuals with brain injury. Brain. 2011;134(5):1541–54. doi:10.1093/brain/awr067.
- Ponsford J, Bayley M, Wiseman-Hakes C, Togher L, Velikonja D, McIntyre A, Janzen S, Tate R. INCOG recommendations for management of cognition following traumatic brain Injury, Part II: attention and speed of information processing. J Head Trauma Rehabil. 2014;29(4):321–37. doi:10.1097/HTR.0000000000000072.
- Gorman S, Barnes MA, Swank PR, Prasad M, Ewing-Cobbs L. The effects of pediatric traumatic brain injury on verbal and visual-spatial working memory. J Int Neuropsychological Soc. 2012;18:29–38. doi:10.1017/S1355617711001251.
- Berninger VW, Abbott RD, Swanson HL, Lovitt D, Trivedi P, Lin S-JC, Gould L, Youngstrom M, Shimada S, Amtmann D. Relationship of word- and sentence-level working memory to reading and writing in second, fourth, and sixth grade. Lang Speech Hear Serv Sch. 2010;41(2):179–93. doi:10.1044/0161-1461(2009/08-0002).
- Pompon, Hunting R, McNeil MR, Spencer KA, Kendall D. Intentional and reactive inhibition during spoken-word stroop task performance in people with Aphasia. J Speech, Lang, and Hearing Res. 2015;24(2):1–14.
- Brownell H, Lundgren K, Cayer-Meade C, Milione J, Katz DI, Kearns K. Treatment of metaphor interpretation deficits subsequent to traumatic brain injury. J Head Trauma Rehabil. 2013;28(6):446–52. doi:10.1097/HTR.0b013e31825b5e85.
- Honan CA, Mcdonald S, Gowland A, Fisher A, Randall RK. Brain & language deficits in comprehension of speech acts after TBI : the role of theory of mind and executive function. Brain Lang. 2015;150(SEPTEMBER):69–79. doi:10.1016/j.bandl.2015.08.007.
- Hay E, Moran C. Discourse formulation in children with closed head injury. A J Speech-Lang Pathol. 2005;14(4):324–36. doi:10.1044/1058-0360(2005/031).
- Kurczek J, Vanderveen N, Duff M. Multiple memory systems and their support of language. SIG 2 Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders. 2014;24(2):64–73. doi:10.1044/nnsld24.2.64.
- Spreij LA, Visser-Meily JMA, Van Heugten CM, Nijboer TCW. Novel insights into the rehabilitation of memory post acquired brain injury: a systematic review. Front Hum Neurosci. 2014;8(December):1–19. doi:10.3389/fnhum.2014.00993.
- Dwk M, Fleming J, Hohaus L, Shum D. Development of the Brief Assessment of Prospective Memory (BAPM) for use with traumatic brain injury populations. Neuropsychol Rehabil. 2011;21(6):884–98. doi:10.1080/09602011.2011.627270.
- Baillargeon A, Lassonde M, Leclerc S, Ellemberg D. Neuropsychological and neurophysiological assessment of sport concussion in children, adolescents and adults. Brain Inj. 2012;26(3):211–20. doi:10.3109/02699052.2012.654590.
- Bourgeois MS, Lenius K, Turkstra L, Camp C. The effects of cognitive teletherapy on reported everyday memory behaviours of persons with chronic traumatic brain injury. Brain Inj. 2007;21(12):1245–57. doi:10.1080/02699050701727452.
- Powell LE, Glang A, Ettel D, Todis B, Sohlberg MM, Albin R. Systematic instruction for individuals with acquired brain injury: results of a randomised controlled trial. Neuropsychol Rehabil. 2012;22(1):85–112. doi:10.1080/09602011.2011.640466.
- Velikonja D, Tate R, Ponsford J, McIntyre A, Janzen S, Bayley M. INCOG Recommendations for management of cognition following traumatic brain injury, Part V: memory. J Head Trauma Rehabil. 2014;29(4):369–86. doi:10.1097/HTR.0000000000000069.
- McDonald S. New frontiers in neuropsychological assessment: assessing social perception using a standardised instrument, the awarenes of social inference test. Aust Psychol. 2012;47(1):39–48. doi:10.1111/j.1742-9544.2011.00054.x.
- De Sousa A, McDonald S, Rushby J, Li S, Dimoska A, James C. Understanding deficits in empathy after traumatic brain injury: the role of affective responsivity. Cortex. 2011;47(5):526–35. doi:10.1016/j.cortex.2010.02.004.
- McDonald S. Impairments in social cognition following severe traumatic brain injury. J Int Neuropsychological Soc. 2013;19(3):231–46. doi:10.1017/S1355617712001506.
- Gamino JF, Chapman SB, Cook LG. Strategic learning in youth with traumatic brain injury: evidence for stall in higher-order cognition. Top Lang Disord. 2009;29(3):224–35. doi:10.1097/TLD.0b013e3181b531da.
- Krawczyk DC, Hanten G, Wilde EA, Li X, Schnelle KP, Merkley TL, Vasquez AC, Cook LG, McClelland M, Chapman SB, et al. Deficits in analogical reasoning in adolescents with traumatic brain injury. Front Hum Neurosci. 2010;4(62):1–13.
- Krawczyk DC. The cognition and neuroscience of relational reasoning. Brain Res. 2012;1428:13–23. doi:10.1016/j.brainres.2010.11.080.
- Nippold MA. Ward-Lonergan JM. Argumentative writing in pre-adolescents: the role of verbal reasoning. Child Lang Teach Ther. 2010;26:238–48. doi:10.1177/0265659009349979.
- Krumnack A, Bucher L, Nejasmic J, Nebel B, Knauff M. A model for relational reasoning as verbal reasoning. Cogn Syst Res. 2011;12:377–92. doi:10.1016/j.cogsys.2010.11.001.
- Gamino JF, Chapman SB, Cook LG. Strategic learning in youth with traumatic Brain Injury. Top Lang Disord. 2009;29(3):224–35. doi:10.1097/TLD.0b013e3181b531da.
- Vas A, Chapman S, Aslan S, Spence J, Keebler M, Rodriguez-Larraina G, Rodgers B, Jantz T, Martinez D, Rakica J, et al. Reasoning training in veteran and civilian traumatic brain injury with persistent mild impairment. Neuropsychol Rehabil. 2016;26(4):502–31. doi:10.1080/09602011.2015.1044013.
- Carrow-Woolfolk E. Comprehensive Assessment of Spoken Language. Los Angeles: American Guidance Service; 2008.
- Dennis M, Purvis K, Barnes MA, Wilkinson M, Winner E. Understanding of literal truth, ironic criticism, and deceptive praise following childhood head injury. Brain Lang. 2001;78:1–16. doi:10.1006/brln.2000.2431.
- Bibby H, McDonald S. Theory of mind after traumatic brain injury. Neuropsychologia. 2005;43(1):99–114. doi:10.1016/j.neuropsychologia.2004.04.027. [accessed 2011 Sep 6].
- Turkstra LS, McDonald S, DePompei R. Social information processing in adolescents: data from normally developing adolescents and preliminary data from their peers with traumatic brain injury. J Head Trauma Rehabil. 2001;16(5):469–83. doi:10.1097/00001199-200110000-00006.
- Babikian T, Asarnow R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology. 2009;23(3):283–96. doi:10.1037/a0015268.
- Leikin M, Ibrahim R, Aharon-Peretz J. Sentence comprehension following moderate closed head injury in adults. J Integr Neurosci. 2012;11(3):225–42. doi:10.1142/S0219635212500197.
- Drummond SS, Boss MR. Functional communication screening in individuals with traumatic brain injury. Brain Inj. 2004;18(1):41–56. doi:10.1080/0269905031000149461.
- Barrow IM, Hough M, Rastatter MP, Walker M, Holbert D, Rotondo MF. The effects of mild traumatic brain injury on confrontation naming in adults. Brain Inj. 2006;20(8):845–55. doi:10.1080/02699050600832445.
- Turkstra L. S., & Byom L. J. (2010) Executive functions and communication in adolescents. ASHA Leader, 15(15). https://doi.org/10.1044/leader.FTR1.15152010.8
- -Snow P, Douglas J, Ponsford J. Procedural discourse following traumatic brain injury. Aphasiology. 1997;11(10):947–67. doi:10.1080/02687039708249421.
- Mozeiko J, Le K, Coelho C, Krueger F, Grafman J. The relationship of story grammar and executive function following TBI. Aphasiology. 2011;25(December):6–7. doi:10.1080/02687038.2010.543983.
- Jones CA, Turkstra LS. Selling the story: narratives and charisma in adults with TBI. Brain Inj. 2011;25(9):844–57. doi:10.3109/02699052.2011.585507.
- Ghayoumi Z, Yadegari F, Mahmoodi-Bakhtiari B, Fakharian E, Rahgozar M, Rasouli M. Persuasive discourse impairments in traumatic brain injury. Archives of Trauma Res. 2015;4(1):e21473. doi:10.5812/atr.21473.
- Moran LM, Taylor HG, Rusin J, Bangert B, Dietrich A, Nuss KE, Wright M, Minich N, Yeates KO. Quality of life in pediatric mild traumatic brain injury and its relationship to postconcussive symptoms. J Pediatr Psychol. 2012;37(7):736–44. doi:10.1093/jpepsy/jsr087.
- Turkstra LS, Brehm SE, Montgomery EB. Analysing conversational discourse after traumatic brain injury: isn’t it about time? Brain Imp. 2006;7:234–45. doi:10.1375/brim.7.3.234.
- Lê K, Coelho C, Mozeiko J, Grafman J. Measuring goodness of story narratives. J Speech, Lang, Hearing Res. 2011;54(1):118–26. doi:10.1044/1092-4388(2010/09-0022).
- Cannizzaro MS, Coelho CA. Analysis of narrative discourse structure as an ecologically relevant measure of executive function in adults. J Psycholinguist Res. 2013;42(6):527–49. doi:10.1007/s10936-012-9231-5.
- Schipper K, Jm A V-M, Hendrikx A, Abma TA. Participation of people with acquired brain injury: insiders perspectives. Brain Inj. 2011;25(August):832–43. doi:10.3109/02699052.2011.589796.
- Turkstra LS. Should my shirt be tucked in or left out? The communication context of adolescence. Aphasiology. 2000;14(4):349–64. doi:10.1080/026870300401405.
- Coelho CA. Discourse production deficits following traumatic brain injury: A critical review of the recent literature. Aphasiology. 2007;9(5):409–29. doi:10.1080/02687039508248707.
- Douglas JM, Knox L, De Maio C, Bridge H. Improving communication-specific coping after traumatic brain injury: evaluation of a new treatment using single-case experimental design. Brain Imp. 2014;15(3):190–201. doi:10.1017/BrImp.2014.25.
- Braden C, Hawley L, Newman J, Morey C, Gerber D, Harrison-Felix C. Social communication skills group treatment: a feasibility study for persons with traumatic brain injury and comorbid conditions. Brain Inj. 2010;24(11):1298–310. doi:10.3109/02699052.2010.506859.
- Cicerone KD, Dahlberg C, Malec JF, Langenbahn DM, Felicetti T, Kneipp S, Ellmo W, Kalmar K, Giacino JT, Harley JP, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehabil. 2005;86(8):1681–92. doi:10.1016/j.apmr.2005.03.024.
- Bloom, M Lahey L. Language development and language disorders.New York: John Wiley and Sons; 1978.
- Halliday MAK. Learning how to mean–explorations in the development of language. London England: Edward Arnold; 1975.
- American, American Speech-Language-Hearing Association. Pragmatic language. 2014. available from http://www.asha.org/slp/PragLangDis/.
- Prutting CA, Kirchner DM. A clinical appraisal of the pragmatic aspects of language. J Speech Hear Disord. 1987;52(2):105–19. doi:10.1044/jshd.5202.105.
- Dahlberg C, Hawley L, Morey C, Newman J, Cusick CP, Harrison-Felix C. Social communication skills in persons with post-acute traumatic brain injury: three perspectives. Brain Inj. 2006;20(4):425–35. doi:10.1080/02699050600664574.
- Ylvisaker M. Person-centred approach to social communication after traumatic brain injury. Brain Imp. 2006;246(3):246–58. doi:10.1375/brim.7.3.246.
- Fyrberg A, Marchioni M, Emanuelson I. Severe acquired brain injury: rehabilitation of communicative skills in children and adolescents. Int J Rehabil Res. 2007;30(2):153–57. doi:10.1097/MRR.0b013e32813a2ee7.
- Hawley LA, Newman JK. Group interactive structured treatment (GIST): a social competence intervention for individuals with brain injury. Brain Inj. 2010;24(11):1292–97. doi:10.3109/02699052.2010.506866.
- Blais MC, Boisvert JM. Psychological and marital adjustment in couples following a traumatic brain injury (TBI): a critical review. Brain Inj. 2005;19(14):1223–35. doi:10.1080/02699050500309387.
- Wiseman-Hakes C, Stewart M, Wassertnan R, Schuller R. Peer group training of pragmatic skills in adolescents with acquired brain injury. J Head Trauma Rehabil. 1998;13(6):23–38. doi:10.1097/00001199-199812000-00005.
- Snow P, Douglas J, Ponsford J. Conversational discourse abilities following severe traumatic brain injury: a follow-up study. Brain Inj. 1998;12(11):911–35. doi:10.1080/026990598121981.
- Bornhofen C, McDonald S. Emotion perception deficits following traumatic brain injury: a review of the evidence and rationale for intervention. J Int Neuropsychological Soc. 2008;14(4):511–25. doi:10.1017/S1355617708080703.
- Cannizzaro MS, Dumas J, Prelock P, Newhouse P. Organizational structue reduces processing load in the prefrontal cortex during discourse processing of written text: implications for high-level reading issues after TBI. Perspect Neurophysiol Neurogenic Speech Lang Disord. 2012;22(2):67–78. doi:10.1044/nnsld22.2.67.
- Vas AK, Spence J, Chapman SB. Abstracting meaning from complex information (gist reasoning) in adult traumatic brain injury. J Clin Exp Neuropsychol. 2015;37(February 2015):152–61. doi:10.1080/13803395.2014.994478.
- Manasse NJ, Hux K, Rankin-Erickson JL. Speech recognition training for enhancing written language generation by a traumatic brain injury survivor. Brain Inj. 2000;14(11):1015–34. doi:10.1080/02699050050191959.
- Kennedy MRT, Krause MO. Self-regulated learning in a dynamic coaching model for supporting college students with traumatic brain injury: two case reports. J Head Trauma Rehabil. 2011;26(3):212–23. doi:10.1097/HTR.0b013e318218dd0e.
- Glang A, Ylvisaker M, Stein M, Ehlhardt L, Todis B, Tyler J. Validated instructional practices: application to students with traumatic brain injury. J Head Trauma Rehabil. 2008;23(4):243–51. doi:10.1097/01.HTR.0000327256.46504.9f.
- Dean PJ, A, Sterr A. Long-term effects of mild traumatic brain injury on cognitive performance. Front Hum Neurosci. 2013; 7(February):30.1–11. Available from https://www.frontiersin.org.
- Mollayeva T, Kendzerska T, Mollayeva S, Shapiro CM, Colantonio A, Cassidy JD. A systematic review of fatigue in patients with traumatic brain injury: the course, predictors and consequences. Neurosci Biobehavioral Rev. 2014;47:684–716. doi:10.1016/j.neubiorev.2014.10.024.
- Belmont A, Agar N, Hugeron C, Gallais B, Azouvi P. Fatigue and traumatic brain injury. Annales De Readaptation Et De Medecine Physique Revue Scientifique De La Societe Francaise De Reeducation Fonctionnelle De Readaptation Et De Medecine Physique. 2006;49(6):283–288, 370–374.
- Henry JA, Griest S, Austin D, Helt W, Gordon J, Thielman E, Theodoroff SM, Lewis MS, Blankenship C, Zaugg TL. Tinnitus screener: results from the first 100 participants in an epidemiology study. Am J Audiol. 2016;25(2):153. doi:10.1044/2016_AJA-15-0076.
- Yorkston KM. Treatment efficacy: dysarthria. J Speech Hear Res. 1996;39:46–57. doi:10.1044/jshr.3905.s46.
- Wambaugh JL. Treatment guidelines for apraxia of speech : lessons for future research. J Med Speech Lang Pathol. 2006;14(4):317–21.
- Lundgren K, Helm-Estabrooks N, Klein R. Stuttering following acquired brain damage: A review of the literature. J Neurolinguistics. 2010;23(5):447–54. doi:10.1016/j.jneuroling.2009.08.008.
- Doettl SM. Sports Concussions (TBI), Imbalance, and dizziness. Perspectives on neurophysiology and neurogenic. Speech Lang Disord. 2015;25(1):36.
- Bowen A, Knapp P, Gillespie D, Dj N, Vail A. Non-pharmacological interventions for perceptual disorders following stroke and other adult-acquired, non-progressive brain injury (Review). Summary of findings for the main comparison. Cochrane Database Syst Rev. 2011;(4). Available from http://www.cochranelibrary.com.
- Green W, Ciuffreda KJ, Thiagarajan P, Szymanowicz D, Ludlam DP, Kapoor N. Accommodation in mild traumatic brain injury. J Rehabil Res Dev. 2010;47(3):183–99. doi:10.1682/JRRD.2009.04.0041.
- Szymanowicz D, Ciuffreda KJ, Thiagarajan P, Optom B, Ludlam DP, Green W, Kapoor N. Vergence in mild traumatic brain injury: A pilot study. J Rehabil Res Dev. 2012;49(7):1083–100. doi:10.1682/JRRD.2010.07.0129.
- Bertisch HC, Long C, Langenbahn DM, Rath JF, Diller L, Ashman T. Anxiety as a primary predictor of functional impairment after acquired brain injury: a brief report. Rehabil Psychol. 2013;58(4):429–35. doi:10.1037/a0034554.
- Gould KR, Ponsford JL, Spitz G. Association between cognitive impairments and anxiety disorders following traumatic brain injury. J Clin Exp Neuropsychol. 2014;36(1):1–14. doi:10.1080/13803395.2013.863832.
- Kreutzer JS, Seel RT, Gourley E, Jeffrey S, Kreutzer RTS. The prevalence and symptom rates of depression after traumatic brain injury: a comprehensive examination. Brain Inj. 2001;15(7):563–76. doi:10.1080/02699050010009108.
- Fleminger S, Oliver DL, Williams WH, Evans J. The neuropsychiatry of depression after brain injury. Neuropsychol Rehabil. 2003;13(1–2):65–87. doi:10.1080/09602010244000354.
- Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: A systematic review of observational studies. Stroke. 2005;36(6):1330–40. doi:10.1161/01.STR.0000165928.19135.35.
- Kneebone II, Dunmore E. Psychological management of post-stroke depression. Br J Clin Psychol. 2000;39:53–65. doi:10.1348/014466500163103.
- Hibbard MR, Uysal S, Kepler K, Bogdany J, Silver J. Axis I psychopathology in individuals with traumatic brain injury. J Head Trauma Rehabil. 1998;13(2):24–39. doi:10.1097/00001199-199808000-00003.
- McDonald S, Fisher A, Togher L, Tate R, Rushby J, English T, Kelly M, Mathersul D, Froreich F, Francis H. Adolescent performance on The Awareness of Social Inference Test: TASIT. Brain Imp. 2015;16(1):3–18. doi:10.1017/BrImp.2015.7.
- Sullivan MP, Griffiths GG, Sohlberg MM. Effect of posttraumatic stress on study time in a task measuring four component proesses underlying text-level reading. J Speech Lang Hearing Res. 2014;57(October):1731–39. doi:10.1044/2014_JSLHR-L-13-0238.
- Waldron B, Casserly L, O’Sullivan C. Cognitive behavioural therapy for depression and anxiety in adults with acquired brain injury. What Works Whom? Brain Inj. 2012;26(4–5):334–35.
- McDonald S, Rushby J, Li S, De Sousa A, Dimoska A, James C, Tate R, Togher L. The influence of attention and arousal on emotion perception in adults with severe traumatic brain injury. I J Psychophysiol. 2011;82(1):124–31. doi:10.1016/j.ijpsycho.2011.01.014.
- Novak JM, Kapolnek KM. Serving clients with mental illness : a collaborative treatment approach. Contemporary Issues in Communication Science and Disorders. 2001;28:111–22.
- Cantor J, Ashman T, Dams-O’Connor K, Dijkers MP, Gordon W, Spielman L, Tsaousides T, Allen H, Nguyen M, Oswald J. Evaluation of the short-term executive plus intervention for executive dysfunction after traumatic brain injury: A randomized controlled trial with minimization. Arch Phys Med Rehabil. 2014;95(1):1–9.e3. doi:10.1016/j.apmr.2013.08.005.
- Riegler LJ, Neils-Strunjas J, Boyce S, Wade SL, Scheifele PM. Cognitive intervention results in web-based videophone treatment adherence and improved cognitive scores. Medical Science Monitor. 2013;19:269–75. doi:10.12659/MSM.883885.
- Schneider S, Haack L, Owens J, Herrington D, Zelek A. An interdisciplinary treatment approach for soldiers with TBI/PTSD: issues and outcomes. SIG 2 Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders. 2009;19(2):36–46. doi:10.1044/nnsld19.2.36.
- Kangas M, McDonald S. Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychol Rehabil. 2011;21(2):250–76. doi:10.1080/09602011.2010.540920.
- Haarbauer-Krupa J Taking care of children after traumatic brain injury. ASHA Perspectives on School Based Issues. 2004;79–86. Available from http://www.asha.org.
- Wehman P, Targett P, West M, Kregel J. Productive work and employment for persons with traumatic brain injury. J Head Trauma Rehabil. 2005;20(2):115–27. doi:10.1097/00001199-200503000-00001.
- Meulenbroek P, Bowers B, Turkstra LS. Characterizing common workplace communication skills for disorders associated with traumatic brain injury: A qualitative study. J Vocat Rehabil. 2016;44(1):15–31. doi:10.3233/JVR-150777.
- Struchen MA, Pappadis MR, Mazzei DK, Clark AN, Davis LC, Sander AM. Perceptions of communication abilities for persons with traumatic brain injury: validity of the La Trobe Communication Questionnaire. Brain Inj. 2008;22(12):940–51. doi:10.1080/02699050802425410.
- Stergiou-Kita M, Dawson DR, Rappolt SG. An integrated review of the processes and factors relevant to vocational evaluation following traumatic brain injury. J Occup Rehabil. 2011;21(3):374–94. doi:10.1007/s10926-010-9282-0.
- McCarty J, Swanson N. Diving into new icd-10 new codes address difficulties reporting some hearing, social communication and cognitive deficit conditions. ASHA Leader. 2016;21:28–30. doi:10.1044/leader.BML.21112016.28.
- Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A. Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J Neurotrauma. 2011;28(June):937–46. doi:10.1089/neu.2010.1516.
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, et al. Initial adult health item banks and first wave testing of the patient-reported outcome measurement information system (PROMISTM) Network: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. doi:10.1016/j.jclinepi.2010.04.011.
- Andelic N, Stevens LF, Sigurdardottir S, Arango-Lasprilla JC, Roe C. Associations between disability and employment 1 year after traumatic brain injury in a working age population. Brain Inj. 2012;26(3):261–69. doi:10.3109/02699052.2012.654589.