Abstract
Objective. To investigate the effects of two differently styled self-care health books in general practice on the frequency and duration of patients’ consultations and their views of the books. Design. Random allocation of patients to either a descriptive or a decision-tree based self-care health book, or a no-book control condition. Three- and 12-months follow-up by postal questionnaire and monitoring of consultations.Setting. A large general practice in the South East of England.Subjects. A total of 1967 volunteer, adult patients who attended the practice in 2001 participated.Main outcome measures. Demographics; health problems; use of health services; use and perceptions of the trial book; frequency and duration of consultations.Results. Response rates to postal questionnaires at 3 and 12 months were 80% and 74%. In all, 48% consulted their allocated book, compared with 25% who consulted any healthcare book in the Control group. Those reporting health problems were more likely to have consulted their allocated book; 60% reported that the allocated book made them more likely to deal with a problem themselves and 40% reported themselves less likely to consult the practice. However, there were no differences in consultation rates or durations of consultations between the three groups.Conclusions. Handing out of self-care health books may provide qualitative benefits for patients but is unlikely to reduce attendance at the GP practice.
An increasing annual consultation rate leading to increased workload in primary care, and the interest in increasing patient self-care, mean that new ways to promote self-management of illness would be welcome Citation[1]. Of 93 patients sampled and interviewed at four GP practices in Denmark, 30% had used books and 20% the Internet as sources for health information although the Internet was not used by older patients Citation[2]. Studies of the effects of leaflets and books on consultation rates and their usefulness to patients have found mixed results. In particular, disease-specific patient information leaflets have been found to increase self-management of illness in the UK and could reduce attendance Citation[3], Citation[4]; general booklets covering a range of common health problems have also been found to reduce attendance in randomized controlled trials (RCTs) in the USA Citation[5] and in Denmark Citation[6]. However, two large, recent RCTs in the UK of general healthcare booklets on common minor illnesses had no effect on attendance Citation[7], Citation[8]. The authors of these studies believed that this might have been due to sending information to registered patients by post and when they were not necessarily ill.
We hypothesize that targeting patients with a comprehensive self-care health book given out at a consultation with implied endorsement, and reinforced subsequently, could successfully encourage patients to self-care and manage their own illnesses. The trial reported in this paper was designed to test changes in duration or frequency of patients’ consultations due to the effects of being given one of these books. This, at the same time, deals with the concern that consultations may take longer if patients use information books. The effects of two differently styled self-care books and a no-book control were compared. Outcomes included the number and duration of consultations with GPs and nurses, all other contacts with the primary health care team and the NHS Direct telephone line over 12 months as well as patients’ perceptions of the usefulness and value of the books.
Material and methods
Setting
The setting was a large general practice in St Albans, UK, which is a prosperous area with a well-educated population and low rates of unemployment.
Sample
All patients attending an appointment with either a doctor or practice nurse over the nine-week period commencing 21 March 2001 were invited to enter the study. Only one member from each household was accepted into the study. Children under 16 were excluded but accompanying adults were invited if registered at the practice. Also excluded were patients who were unable to read or write English, patients with dementia and patients who were visiting the practice without seeing a doctor or nurse.
Sample size was determined as the minimum required to detect a difference between intervention groups of an average of one consultation per annum to give a power of 80% at a significance level of 0.05. This required at least 650 participants in each arm of the study.
Intervention
The books used were the United Kingdom edition of the Healthwise Handbook (HW), a self-care guide developed in the USA and used by Kaiser Permanente and other managed healthcare organizations in North America to enhance people's ability to take charge of their health, and the NHS Direct Healthcare guide (NHSd) designed to work alongside the NHS Direct telephone service. HW has 350 indexed pages of illustrated descriptive text, covering first aid and emergencies, health problems and staying healthy and how best to use the doctor and nurse. It describes over 180 conditions organized in chapters by body areas and functions, together with home treatment and when to see a doctor. It has been found effective in encouraging self-care in the US Citation[9] as part of a self-care encouragement programme. NHSd has 128 indexed pages containing photographs and is organized by main presenting symptom in colour-coded body areas. It provides decision support flow charts to help decide when it is safe to self-treat, with tips on what to do, and when to seek medical attention; the introduction includes simple advice on emergencies and healthy living.
Procedure
Consenting patients were block-randomized to three equal-sized groups for which the allocation was in a numbered, sealed envelope generated independently. Each block of 30 envelopes provided for the randomization of 10 patients to each group. At the consultation the practitioner, as directed by the contents of the patient's envelope, issued the patient with either a Healthwise book, an NHSd book, or a letter about the Control group. An on-screen ‘reminder’ was automatically generated at subsequent consultations that informed the practitioner which book, if any, the patient had been given. Practitioners were asked to encourage and reinforce the use of whichever book had been allocated. To avoid the possibility of bias due to the lack of blindness, all practitioners were asked to reinforce the books impartially.
Measures
During enrolment patients completed a baseline demographic questionnaire including education and occupation. Follow-up questionnaires that asked about health problems in the previous 3 or 9 months, health services used, and health information materials read were sent to all participants at 3 and 12 months. Participants who had been allocated a book were asked about their views and use of the book in general and in relation to their most recent illness or health problem. After four weeks a reminder with replacement questionnaire was sent to non-responding participants. The questionnaires were developed from model questionnaires that had been successful in other studies and refined after piloting on a small number of volunteer patients. Face validity was established by the views of a panel of experts in the field. No statistical evaluation of reliability was obtained.
Consultation data were collected for the 12 months following enrolment using computer system searches (In Practice Systems Ltd: Vision). These included the routine, emergency, and out-of-hours contacts with a doctor or practice nurse, and the duration of consultations. Practice consultations greater than 40 minutes were excluded from the analyses, as many were the result of a recording failure. NHS Direct provided information on participants telephoning their service during the study 12 months.
Analysis
Analysis used an intention-to-treat approach except where stated and consisted of comparison of proportions and means, with 95% confidence intervals, between the three arms of the study with tests of statistical significance by chi-square, t-test, and non-parametric tests where appropriate. A multivariable logistic regression model was also used.
Results
Sample and participant characteristics
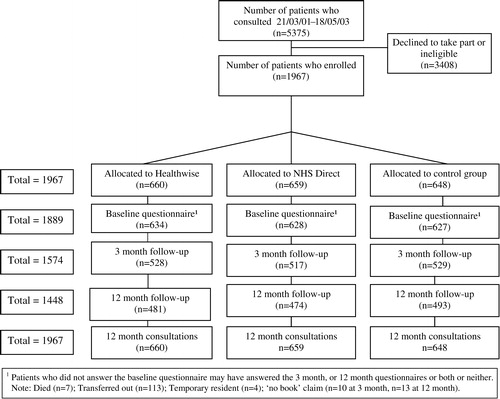
A total of 1967 patients were enrolled. This represents 44% of the 4507 patients aged 16+ who attended during the enrolment period and shows a small excess of females aged 30 to 49. Baseline questionnaires were completed by 1889 participants. Follow-up questionnaires were returned by 1574 and 1448 participants at three and 12 months respectively. Consultation records were analysed for all 1967 participants (see ).
The age and sex distributions of the participants are given in . These distributions and the male-to-female ratio were representative of the population of attenders at the practice and show that the randomization was successful in creating comparable groups at baseline. Some 86% of participants were from non-manual rather than manual social class and 73% had educational qualifications at or beyond ‘A’ Level. In total, 18% of males and 12% of females did not respond to questionnaires beyond the baseline. The dropout rate was higher in the manual (26%) than in the non-manual group (17%) (p < 0.001).
Table I. Age and sex distribution of participating patients by treatment arm.
Use of allocated books
Those allocated a book were likely to have consulted it. In the first three months 55% of those given the HW book and 42% of those given the NHSd book responded that they had consulted it at least once. Similar proportions were found over the remaining nine months. Among those who completed both 3- and 12-month questionnaires, some 50% of those who did not consult their book in the first 3 months did so during the following 9 months. Among those given either the HW or the NHSd book, those aged 60+ were more likely to have consulted it.
Those allocated to the control group were asked how many times they had consulted ‘any healthcare book’. Around 25% of those allocated to the control group had consulted a healthcare book at least once at 3 and 12 months.
At three months, 80% of the controls that reported that they had consulted a book and 72% of the HW and 57% of the NHSd groups that reported that they had consulted their allocated book had also taken advice from the book. The corresponding figures for the next nine months were 68%, 82%, and 59% respectively. After three months, 69% of those reporting a health problem had consulted their allocated book compared with 49% of those reporting no health problem (p < 0.001). A very similar result was found after the next nine months.
Participants’ perceptions of allocated books
Participants who had been allocated a book and had consulted it at least once were asked whether the book provided all of the information required. Responses were requested on a scale from 1 (all provided) through to 5 (none provided). Those allocated the HW book gave a mean response of 2.42 (SD = 1.09) compared with 2.85 (SD = 1.30) for those allocated the NHSd book (p < 0.001). Similarly, although both books were found to be easy to understand by most participants, the HW book was seen as better for understanding (p < 0.001), and better for knowing what to do (p < 0.001); the advice from the HW book was followed more often (p = 0.002), and using the HW book was more often likely to lead to a change of mind on what to do (p = 0.003).
Participants whose educational qualifications were below ‘A’ level were more likely to report that they found the information in the HW book ‘harder to understand’ than did those whose qualifications were at or above ‘A’ level, at both 3 months (p = 0.004) and 12 months (p = 0.006). Similarly, at 3 months, those whose educational qualifications were below ‘A’ level were more likely to report that they found the information in the NHSd book ‘useful for knowing what to do’ than did those whose qualifications were at or above ‘A’ level (3 months, p = 0.012; 12 months, p = 0.009).
In both book groups, in response to the question ‘did using the book make you more or less likely to try to deal with the problem yourself?’ around 57%, at both 3 and 12 months, responded ‘more likely’. This compares with only around 13% responding ‘less likely’ (p < 0.001). The question ‘Did using the book make you more or less likely to contact the practice?’ resulted in a response of ‘less likely’ in some 40% of study participants compared with around 20% who responded ‘more likely’ (p < 0.001) (see ).
Table II. Distribution (%) of reported likelihood of self-care and use of GP service at 3 and 12 months by book group.
Consultation rates
Mean annual consultation rates, including routine GP consultations and emergency consultations with a GP or nurse practitioner, for the 12-month period of the study, classified by age group, sex, and book group, did not, in general, differ between the three arms of the study and are given in . Differences between the groups in visits to accident and emergency facilities at hospitals and in telephone calls, home visits, and nurse clinics were small and not statistically significant.
Table III. Annual consultation rates by age and sex and study arm.
Duration of consultations
The mean lengths of consultations in the three arms of the study were 9.9 (9.6 to 10.1), 9.7 (9.4 to 9.9), and 10.0 (9.8 to 10.3) minutes in the Control, Healthwise, and NHS Direct book groups respectively. The differences between these values were not statistically significant.
Use of NHS Direct telephone service
A total of 160 participants made an average of 1.19 calls to the NHS Direct telephone service. In a multivariable logistic regression model the odds for calling NHS Direct were nearly doubled for being allocated to NHSd group rather than to Control or to HW group (p < 0.01).
Discussion
A strength of this study, by comparison with previous studies Citation[7], Citation[8] is that self-care information books were endorsed through being handed to participating patients by the practitioner at a consultation and referred to at any subsequent consultations. This is in contrast to some previous studies that used much smaller booklets and some that distributed them by post to all registered patients.
The study shows that approximately half of patients given either self-care book consulted it compared with only a quarter of those in the control group who consulted any healthcare book. This shows a considerable potential benefit of the giving out of such books, although an element of ‘social desirability’ must be allowed for in patients’ responses to the questionnaires. The books did not, however, reduce the number of visits to the GP. This is surprising given that around 57% reported that the book made them more likely to try to deal with their health problem themselves and around 40% reported that the book make them less likely to contact the practice. An answer to this apparent contradiction may be found in the qualitative research in Canada by Mullett Citation[9] who found (p. 114) that many patients who dealt with their health problem with the help of the Healthwise book later visited the GP to obtain reassurance and confirmation about what they had done. Using the approach we adopted it seems unlikely that either of these books can reduce consultation rates or workload. We can, however, speculate as to whether the books may benefit the appropriateness or quality of patients’ consultations with the GP. Mullett Citation[9] found that patients given the Healthwise book felt better able to talk with their doctor about health issues. Further research with a qualitative component should be carried out to elucidate this.
Calls to the NHS Direct telephone advice service were more frequent among those given the NHSd book. We assume this is due to the recommendation of the service in the book. This dual book–telephone approach to supporting self-care would appear useful, especially in view of the trend to increased telephone use in younger age groups. It may be that books will become less relevant as sources of information for this age group.
At a recent UK conference on learning from Kaiser Permanente, a Californian healthcare provider that uses the Healthwise book, recommendations were made about the importance of supporting self-care and shared care Citation[10], Citation[11]. Comparison of the two books showed that significantly more patients appeared to value the Healthwise book over the NHS Direct book in relation to information, understanding, advice followed, knowing what to do, and change of mind about what to do. Neither book increased the time spent during consultations. This should inform policy for the future use and design of self-care books.
The practice in which the study was carried out was, in most respects, typical of large GP practices in the UK, and there had been no special encouragement of self-care prior to the study reported here. Nonetheless, generalization of the findings of this study is limited by the relative affluence of the area in which it was carried out. Taken together with the lower dropout rate in the non-manual compared with the manual social classes, this means that the findings are more representative of the responses of patients in non-manual occupations. The design power made the study insensitive to differences smaller than 1.0 in the mean annual consultation rate. Thus an effect of the interventions that is smaller than this remains a possibility.
Key Points
Previous studies of the effects of self-care health books on consultation rates have found mixed results.
Self-care health books given to patients at a consultation were read and valued.
Patients given a self-care health book reported that it made them more likely to self-manage illness.
Frequency and duration of consultations with practitioners were not substantially affected by giving patients a self-care health book.
The authors would like to thank all those who worked at Parkbury House Surgery during the recruitment period, and all the GPs and nurses who were involved during the study period. Thanks also to Hertnet and CRIPACC (Centre for Research in Primary and Community Care, University of Hertfordshire, Hatfield, Herts, AL10 9AB, UK) for support and to NHS Direct for telephone use data. The study was funded by Hertnet: the Hertfordshire Primary Care Research Network. A Platts was one of the UK editors of the Healthwise book and was given 500 copies of the book for use in the study.
References
- Department of Health. The NHS Plan. A plan for investment: a plan for reform. Norwich: Stationery Office; 2000.
- Budtz S, Witt K. Consulting the Internet before visit to general practice. Patients' use of the Internet and other sources of health information. Scand J Prim Health Care 2002; 20: 174–6
- MacFarlane J, Holmes W, MacFarlane R. Reducing reconsultations for an acute lower respiratory tract illness with an information leaflet: a randomised controlled study of patients in primary care. Brit J Gen Pract 1997; 47: 719–22
- Roland M, Dixon M. Randomised controlled trial of an educational booklet for patients presenting with back pain in general practice. J Roy Coll Gen Pract 1989; 39: 244–6
- Vickery D, Kalmer H, Lowry D, Constantine M, Wright E, Loren W. Effect of a self-care program on medical visits. JAMA 1983; 250: 2952–6
- Hansen B. A randomised controlled trial on the effect of an information booklet for young families in Denmark. Patient Educ Couns 1990; 16: 147–50
- Little P, Somerville J, Williamson I, Warner G, Moore M, Wiles R, et al. Randomised controlled trial of self-management leaflets and booklets for minor illness provided by post. BMJ 2001; 322: 1214–7
- Heaney D, Wyke S, Wilson P, Elton R, Rutledge P. Assessment of impact of information booklets on use of healthcare services: randomised control trial. BMJ 2001; 322: 1218–21
- Mullett J, Hills M. What information and support do people seek to help them make decisions about self-care?. Int J Health Promotion Educ 2002; 40: 111–19
- NHS: NatPaCT conference 4 November, 2003.
- The Times. Learn from US health system, Reid tells NHS. The Times 2003, 5 November.