Abstract
Objective: To investigate how cancer patients in Norway use primary care out-of-hours (OOH) services and describe different contact types and procedures.
Design: A retrospective cross-sectional registry study using a billing registry data source.
Setting: Norwegian primary care OOH services in 2014.
Subjects: All patients’ contacts in OOH services in 2014. Cancer patients were identified by ICPC-2 diagnosis.
Main outcome measures: Frequency of cancer patients’ contacts with OOH services, contact types, diagnoses, procedures, and socio-demographic characteristics.
Results: In total, 5752 cancer patients had 20,220 contacts (1% of all) in OOH services. Half of the contacts were cancer related. Cancer in the digestive (22.9%) and respiratory (18.0%) systems were most frequent; and infection/fever (21.8%) and pain (13.6%) most frequent additional diagnoses. A total of 4170 patients had at least one cancer-related direct contact; of these, 64.5% had only one contact during the year. Cancer patients had more home visits and more physicians’ contact with municipal nursing services than other patients, but fewer consultations (p < 0.001). Patients in the least central municipalities had significantly more contacts than more central municipalities (p < 0.001).
Conclusion: There was no indication of overuse of OOH services by cancer patients in Norway, which could indicate good quality of cancer care in general.
Many are concerned about unnecessary use of emergency medical services for non-urgent conditions.
• There was no indication of overuse of out-of-hours services by cancer patients in Norway.
• Cancer patients had relatively more home visits, physician’s contact with the municipal nursing service, and weekend contacts than other patients.
• Cancer patients in the least central municipalities had relatively more contacts with out-of-hours services than those in more central municipalities.
KEY POINTS
Introduction
Many countries are concerned about unnecessary use of emergency medical services for non-urgent conditions, as this contributes to inefficient use of care resources.[Citation1–4] Several factors such as clinical, socio-demographic, and organisational are found to influence how the population use primary care out-of-hours (OOH) services. More frequent use of OOH services is associated with frailty, psychiatric disease, cardiovascular disease, and cancer, as well as female sex, very young or very old age, low-income level, and receiving homecare nursing.[Citation5,Citation6] It has also been shown that patients with chronic disease contact OOH services due to exacerbation of already diagnosed chronic disease,[Citation7] and that frequent use of daytime general practice is associated with OOH contacts due to exacerbation.[Citation8] Additionally, organisational factors, such as short distance to the location of the OOH service, higher degree of urbanisation, and low accessibility to daytime primary care, are associated with more frequent use.[Citation1,Citation9,Citation10]
Several studies have investigated cancer patients’ use of emergency medical services. A German study found palliative care in advanced cancer accounted for 2.5% of all emergency medical services, and uncontrolled symptoms were the most frequent reason for contact.[Citation11] In a British longitudinal observational study, Richards et al. observed that around 2% of calls to primary care OOH services were from cancer patients, of whom 56% had advanced cancer needs.[Citation12] Adam et al. found that the most frequent reason for cancer patients contacting OOH services in Scotland was poor pain management, although 53.8% were already prescribed strong opiate analgesics.[Citation13] In an Italian study, Buja et al. also showed that cancer was associated with a higher relative risk of being referred to an emergency department consultation as opposed to a telephone consultation, but cancer patients had a lower relative risk of being referred to the GP’s office for consultation.[Citation14] To ensure continuity of care, OOH services should optimally be used for acute health problems, while treatment of non-urgent conditions and regular care for patients, including cancer patients, should be accomplished during daytime.
Norway has a high OOH contact rate compared to other countries with available data, and 75% of contacts are classified as non-urgent.[Citation15] One reason for this is that Norway has a strict gatekeeper system; patients cannot go directly to hospitals. Another reason could be low accessibility to the general practitioner during daytime.[Citation15] However, we know little about how Norwegian cancer patients use OOH services. The aim of this study was to investigate how cancer patients in Norway use OOH services and describe different contact types and procedures, using a billing registry data source. Our hypothesis was that cancer patients constitute a relatively large proportion of OOH contacts.
Material and methods
Data source
The material in this study was based on all electronic billing claims from physicians working in primary care OOH services in Norway in 2014. OOH services are organised by the municipalities, may differ in organisation, but all send electronic billing claims to the Norwegian Health Economics Administration (HELFO), which is responsible for remuneration. For every patient contact, a billing claim is made to HELFO. A claim identifies the physician and contains personal details about the patient, diagnosis and fee codes for different types of contacts, procedures, time use, and special qualifications of the physician (approved specialist or PhD degree).[Citation16] All patients were de-identified and given a pseudonymous identification number (pseudo ID). The data file was delivered by HELFO to the National Centre for Emergency Primary Health Care, as part of a contract to produce an annual report about the OOH services.[Citation16]
Subjects
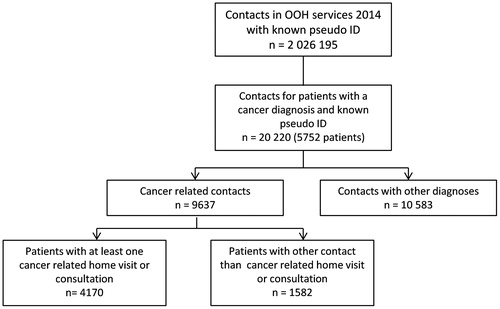
All contacts identified by electronic billing claims in OOH services in 2014 were included (). Paper-based claims, < 1%, were not included. We identified cancer patients with at least one OOH contact during 2014 by identifying billing claims holding a cancer diagnosis, according to the International Classification of Primary Care (ICPC-2).[Citation17] One billing claim was defined as one contact. We also included ‘contacts with other diagnoses’ for these patients, identified by pseudo ID. These contacts did not hold a cancer diagnosis and thus could not be identified as cancer related with certainty. Contacts with missing pseudo ID (n = 36) and without one of the below classified contact types (n = 36) were excluded.
Variables
The following variables were used: age, sex, time and type of contact, diagnosis, procedures, municipality centrality, physician sex, and physician age.
Age for patients was divided into four strata: 0–40, 41–60, 61–80, and >80 years, and time of contact into three strata: Monday–Friday, hours 08-15; Monday–Friday, hours 16-07; and Saturday–Sunday, hours 0–24. Physician age was divided into five strata: 20–29, 30–39, 40–49, 50–59, and ≥60 years.
Type of contact was classified as consultation, home visit, simple contact, telephone, and physician’s contact with the municipal nursing service. The variable “home visit” also includes physicians’ call outs to other destinations than the patientś home (e.g., traffic accident).
Cancer diagnoses according to ICPC-2 were categorised according to main site of malignancy: A: General and unspecified; B: Blood, blood-forming organs, immune mechanism; D: Digestive; R: Respiratory; U: Urological; X: Female genital; Y: Male genital; and Other: cancer diagnosis with frequency of less than 5% of cancer-related contacts.
Non-cancer diagnoses according to ICPC-2 were categorised as pain; infection/fever; respiratory; genitourinary; neurological; gastrointestinal; haematological; cardiovascular; musculoskeletal; psychiatric; death; and other. Symptom diagnoses were given precedence over organ-specific diagnosis, for example, pain is reported as a frequent symptom in cancer. As an example, pneumonia was coded as “infection/fever” and abdominal pain as “pain”. Fear of a diagnosis, for example, “fear of cancer” was coded as “psychiatric”.
Procedures with a frequency of at least 2% of cancer-related contacts were included: laboratory total, C-reactive protein (CRP), cell count, electrocardiogram (ECG), glucose and surgical procedures. Additionally, sick leave, fees for long consultations, and consulting with next of kin were included. Procedures are not mutually exclusive, and several can be coded into one contact. Centrality was defined as a municipality’s geographical location in relation to a centre where there are important central functions, and measured on a scale from 0 to 3, where 0 is least central (rural) and 3 is most central (urban).[Citation18]
Cancer patients’ contacts were compared with contacts of all other patients visiting OOH services during 2014. Cancer patients’ contacts with other diagnoses were compared with their cancer-related contacts. Cancer-related direct contacts (consultations or home visits) were analysed according to age, main cancer diagnosis, and additional diagnoses noted during the same contact.
Statistics
The data were analysed with IBM SPSS Statistics 22.0® (IBM Corp, Armonk, NY). Comparisons were done by frequency tables and Pearson Chi-square analyses. In the procedures category, Chi-square analyses were done on each category separately, as procedures are not mutually exclusive in one contact. Finally, we performed multiple logistic regression analyses, using home visits or consultations as dependent variable. Independent variables were patient sex, patient age, cancer-related contacts or contacts with other diagnoses, municipality centrality, physician sex, and physician age. A similar regression analysis also included diagnoses, but did not alter the main findings, and is not presented. Unadjusted and adjusted odds ratios (OR) were presented with 95% confidence intervals (CI) and p value. For all analyses, significance was accepted at the 5% level (p < 0.05).
Ethical approvals and data protection
Since the data were anonymised, the Norwegian Social Science Data Services assessed the project as not subject to obligatory notification. For the same reason, the Norwegian Labour and Welfare Administration concluded that there was no need to apply for dispensation from professional secrecy requirements.
Results
Patients
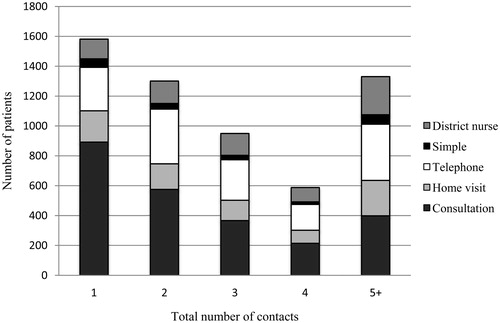
There were 5752 patients with a cancer-related contact in the material. About 55.1% of the patients were male (mean age 70.1 years) and 44.9% female (mean age 67.5 years). A total of 4170 patients had at least one cancer-related direct contact (home visit or consultation). Out of these, 64.6% had only one contact with the OOH services, while 5.2% had five or more cancer-related contacts during the year. Additionally, 63.2% of the cancer patients also had contacts with other diagnoses, nearly half of these with at least one home visit or consultation. When looking at cancer-related contacts and contacts with other diagnoses together, about a quarter of the patients had only one contact with OOH services during the year, while another quarter had five or more contacts (). As number of contacts increases, the relative share of consultations decreases.
Contacts
There were 20,220 contacts for patients identified with a cancer diagnosis, constituting 1.0% of all contacts in OOH services in 2014. Roughly, half of the contacts from cancer patients were cancer related. Cancer in the digestive system (22.9%) was the most frequent ICPC-2 diagnosis in cancer-related contacts, followed by cancer in the respiratory system (18.0%). The most common additional diagnoses were infection/fever (21.8%) and pain (13.6%).
Comparing cancer patients with other patients
Distribution of contact types were significantly different for patients with a cancer diagnosis, compared with patients with other diagnoses (). Relative distribution of contact types showed that cancer patients had more home visits and that physicians more often had contact with the municipal nursing services, but there were fewer consultations. There were also more contacts on weekends for cancer patients. Moreover, there were significantly more contacts for cancer patients in the least central municipalities, but fewer contacts in central and somewhat central municipalities than for patients with other diagnoses. For procedures, although statistically significant, there were only small differences. The most important differences were almost four times more consulting with next of kin, as well as three times more haematological cell count for cancer patients, but less sick leave.
Table 1. Contacts for cancer patients (cancer related and contacts with other diagnoses) and other patients in out-of-hours services 2014 by contact type, time, municipality centrality, and procedures.
Comparing cancer patients’, cancer-related contacts, and contacts with other diagnoses
There were significantly more home visits, but less telephone consultations for cancer-related contacts compared to contacts with other diagnoses (). Also, there were more cancer-related contacts in the least central municipalities. In general, there was a pattern with more contacts in the least central municipalities, then fewest in less central and somewhat central municipalities, before an increase again in the central municipalities. Procedures for cancer-related contacts and contacts with other diagnoses were only marginally different, but statistically significant. Relevant differences were five times more consulting with next of kin for cancer-related contacts, and twice as many ECGs for contacts with other diagnoses.
Comparing home visits and consultations
There were 5764 direct contacts (home visit or consultation) in cancer-related contacts. A significant association was found between age and type of direct contact (). Patients aged 80 years or older had more home visits, while patients younger than 60 years had more consultations. Most frequent diagnoses did not differ from cancer-related contacts in total, but death was a frequent reason for home visits.
Table 2. Home visits and consultations in cancer-related contacts for out-of-hours services 2014, by age (n = 5764), main cancer diagnosis (n = 5764) and additional diagnoses noted in the same contact (n = 2533).
Multiple regression analyses showed that there were significantly more home visits for cancer-related contacts than contacts with other diagnoses, adjusted OR 1.51 (95% CI: 1.37, 1.66) (). There was also a clear trend with higher OR for home visits with an increasing age. A trend with most home visits in the least central municipalities, followed by fewest home visits in less central municipalities and then an increase by municipality centrality was also found. Male physician was associated with higher OR of home visits, as were the oldest and youngest physicians.
Table 3. Odds ratio (OR) for home visit compared with consultation in contacts for cancer patients in out-of-hours services in 2014.
Discussion
Principal findings
There was no indication of overuse of OOH services by cancer patients in this study. Only 1% of all contacts in OOH services were from cancer patients; half of them cancer related. The majority had only one direct cancer-related contact. Cancer in the digestive or respiratory system was most frequent, while the most common additional diagnoses were infection/fever and pain. Cancer patients had more home visits and physicians’ contact with the municipal nursing services, and more weekend contacts than patients without cancer. There was a trend of more home visits with increasing age. Also, cancer patients living in the least central municipalities had relatively more contacts with the OOH services.
Findings in relation to other studies
In our study, we identified 5752 cancer patients in contact with OOH services during one year, only 1% of contacts in the OOH service. Meanwhile, 230,000 earlier diagnosed and around 30,000 newly diagnosed patients with cancer of any type and staging were living in Norway in 2013.[Citation19] Thus, few Norwegian cancer patients were in contact with OOH services, and they had few contacts compared with studies in other countries.[Citation11,Citation12] There is a high consistency across countries for diagnostic scope in primary care OOH services,[Citation20] and this could indicate that most cancer patients are adequately followed up by their GP during office hours, directly by an oncological hospital ward, or other specialised or palliative care unit.
In our study, 65% of the cancer patients had only one direct cancer-related contact during the year, close to Mayer et al. who found that 77% of cancer patients visiting emergency departments only had one visit.[Citation21] We found, however, that 5% had five or more, and about 1% (41 different patients) 10 or more cancer-related contacts. This difference could mean inequality in healthcare services offered in Norwegian municipalities, as frequent use of OOH services could be an indicator of poor quality cancer care.[Citation22] Another explanation may be increased symptom burden in some stages of the disease. Patients with cancer in the digestive and respiratory system had most contacts with OOH services, while infection/fever and pain were the most common additional symptoms. A systematic review investigating symptoms in cancer patients visiting emergency departments found infection and pain were frequent reasons for contact.[Citation23] Respiratory distress and digestive symptoms are also common reasons for cancer patients visiting OOH services, emergency departments or being hospitalised.[Citation21,Citation24,Citation25] The very frequent use of OOH for a very small number of patients may be well justified, due to tasks or procedures that need to be performed by a physician during evenings, nights, and weekends. But we cannot rule out the possibility that some of these patients should have been given planned, comprehensive services by other agencies than the OOH. Cancer patients had more home visits than other diagnoses, especially the oldest patients, which could be because of more severe symptoms or frail state, not permitting them to travel to the OOH surgery, or being in a homebound palliative phase.
There was a clear trend of overrepresentation of OOH contacts for cancer patients in less central municipalities. One explanation could be that the GP and OOH physician in the least central municipalities often is the same person. The boundary between ordinary office practice and OOH duty may be blurred, and the physician may prefer to perform home visit OOH, as the work burden during OOH duty may be low in these areas. Another contributing factor could be that smaller municipalities more often have problems recruiting and retaining GPs over time. Rapid turnover of GPs and use of temporary positions could lead to suboptimal care in-hours and force patients to use emergency services.[Citation26] The fact that less central and central municipalities have fewest home visits could be attributed to intermunicipal cooperation for OOH services. Having one OOH physician covering a large geographical area makes it more difficult to leave the OOH surgery and make home visits.
Not only medical and geographical criteria decide whether a patient receives home visits, but also characteristics of the physician. Interestingly, we found that male physicians, as well as the oldest and youngest physicians performed more home visits. Ingram et al. showed the same gender difference in OOH home visits in general, but also that female physicians had more hospital referrals.[Citation27] The age differences with more home visits by older physicians could be due to a former tradition where GPs made more home visits in general, while for the youngest physicians, inexperience may be a contributing factor.
The fact that cancer patients had more contacts on weekends could mean there is need for better anticipatory planning of foreseeable situations that can occur, and how to solve these, for example, a plan for treating exacerbation of pain. A recent randomised controlled trial training GPs in early identification and anticipatory palliative care planning found no difference in contacts with OOH services, but more contacts with the GP, less hospitalisations and more home death.[Citation28] However, only a quarter of the patients who died were identified in the intervention group. In another study, case conferences between GPs and specialist palliative care teams significantly reduced service utilisation, including emergency department admissions.[Citation29]
Strengths and weaknesses
To the best of our knowledge, this is the first study to investigate cancer patients’ use of OOH services in Norway. A major strength is that the data are population based. However, the billing claims are secondary data and not collected for research purpose. Another limitation is that we cannot be sure all cancer patients are identified correctly, as physicians may not have given the cancer diagnosis on the billing claims. For instance, if the reason for contact was pain, it may have been cancer related, although this is not apparent in the billing claim. But as we cannot be certain of the origin of the diagnoses, we have chosen to divide cancer patient´s contacts into two categories for some of the results. Additionally, the billing claims contain no other clinical data than diagnosis, and it is not possible to ascertain the outcome of the contact, e.g. if the patient was hospitalised.
Conclusion
In conclusion, there was no indication of overuse of OOH services by cancer patients in Norway, which could indicate good quality cancer care in general. However, cancer patients were overrepresented in receiving home visits.
Acknowledgements
The study was funded by the National Centre for Emergency Primary Health Care, Uni Research Health. We thank the GC Rieber Foundation for providing financial support for a PhD candidate (CKT), and the Centre for Elderly and Nursing Home Medicine, University of Bergen for providing a scientific environment.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Smits M, Peters Y, Broers S, et al. Association between general practice characteristics and use of out-of-hours GP cooperatives. BMC Fam Pract. 2015;16:52.
- Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19:47–59.
- Ismail SA, Gibbons DC, Gnani S. Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. Br J Gen Pract. 2013;63:e813–e820.
- Christensen MB, Christensen B, Mortensen JT, et al. Intervention among frequent attenders of the out-of-hours service: a stratified cluster randomized controlled trial. Scand J Prim Health Care. 2004;22:180–186.
- Buja A, Toffanin R, Rigon S, et al. What determines frequent attendance at out-of-hours primary care services? Eur J Public Health. 2015;25:563–568.
- Sandvik H, Hunskaar S, Diaz E. Use of emergency medical services by patients encompassed by the regular GP scheme. Tidsskr Nor Laegeforen. 2012;132:2272–2276.
- Flarup L, Moth G, Christensen MB, et al. Chronic-disease patients and their use of out-of-hours primary health care: a cross-sectional study. BMC Fam Pract. 2014;15:114.
- Flarup L, Moth G, Christensen MB, et al. Daytime use of general practice and use of the out-of-hours primary care service for patients with chronic disease: a cohort study. BMC Fam Pract. 2014;15:156.
- Raknes G, Hansen EH, Hunskaar S. Distance and utilisation of out-of-hours services in a Norwegian urban/rural district: an ecological study. BMC Health Serv Res. 2013;13:222.
- Jansen T, Zwaanswijk M, Hek K, et al. To what extent does sociodemographic composition of the neighbourhood explain regional differences in demand of primary out-of-hours care: a multilevel study. BMC Fam Pract. 2015;16:54.
- Wiese C, Bartels U, Ruppert D, et al. Notärztliche Betreuung von Tumorpatienten in der finalen Krankheitsphase [Treatment of oncology patients in the final stadium of disease by prehospital emergency physicians]. Anaesthesist. 2007;56:133–140.
- Richards SH, Winder R, Seamark D, et al. Accessing out-of-hours care following implementation of the GMS contract: an observational study. Br J Gen Pract. 2008;58:331–338.
- Adam R, Wassell P, Murchie P. Why do patients with cancer access out-of-hours primary care? A retrospective study. Br J Gen Pract. 2014;64:e99–104.
- Buja A, Toffanin R, Rigon S, et al. Out-of-hours primary care services: demands and patient referral patterns in a Veneto region (Italy) local health authority. Health Policy. 2015;119:437–446.
- Hansen EH, Zakariassen E, Hunskaar S. Sentinel monitoring of activity of out-of-hours services in Norway in 2007: an observational study. BMC Health Serv Res. 2009;9:123.
- National Centre for Emergency Primary Health Care. Årsstatistikk fra legevakt. 2014. [Statistics out-of-hours services 2014]. Report No. 2-2015. Bergen: National Centre for Emergency Primary Health Care, Uni Research Health; 2015.
- Wonca International Classification Committee (WICC). ICPC-2 – English. International Classification of Primary Care - 2nd ed. 2015. Available from: http://www.kith.no/upload/2705/ICPC-2-English.pdf 2015 [cited 2015 Jun 9].
- Statistics Norway. Variabeldefinisjon: Sentralitet [Variable definition: Municipality centrality]. 1994. Available from: https://www.ssb.no/a/metadata/ conceptvariable/vardok/927/nb1994 [accessed 2016 Jan 19].
- Cancer Registry of Norway. Cancer in Norway 2013: Cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway; 2015.
- Huibers LA, Moth G, Bondevik GT, et al. Diagnostic scope in out-of-hours primary care services in eight European countries: an observational study. BMC Fam Pract. 2011;12:30.
- Mayer DK, Travers D, Wyss A, et al. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol. 2011;29:2683–2688.
- Earle CC, Park ER, Lai B, et al. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003;21:1133–1138.
- Vandyk AD, Harrison MB, Macartney G, et al. Emergency department visits for symptoms experienced by oncology patients: a systematic review. Supp Care Cancer. 2012;20:1589–1599.
- De Korte-Verhoef MC, Pasman HR, Schweitzer BP, et al. Reasons for hospitalisation at the end of life: differences between cancer and non-cancer patients. Supp Care Cancer. 2014;22:645–652.
- De Korte-Verhoef MC, Pasman HR, Schweitzer BP, et al. End-of-life hospital referrals by out-of-hours general practitioners: a retrospective chart study. BMC Fam Pract. 2012;13:89.
- Abelsen B, Gaski M, Brandstorp H. Duration of general practitioner contracts. Tidsskr Nor Laegeforen. 2015;22:2045–2049.
- Ingram JC, Calnan MW, Greenwood RJ, et al. Risk taking in general practice: GP out-of-hours referrals to hospital. Br J Gen Pract. 2009;59:e16–e24.
- Thoonsen B, Vissers K, Verhagen S, et al. Training general practitioners in early identification and anticipatory palliative care planning: a randomized controlled trial. BMC Fam Pract. 2015;16:126.
- Mitchell G, Zhang J, Burridge L, et al. Case conferences between general practitioners and specialist teams to plan end of life care of people with end stage heart failure and lung disease: an exploratory pilot study. BMC Palliat Care. 2014;13:24.