Abstract
Objective: To explore how a student-run clinic (SRC) in primary health care (PHC) was perceived by students, patients and supervisors.
Design: A mixed methods study. Clinical learning environment, supervision and nurse teacher evaluation scale (CLES + T) assessed student satisfaction. Client satisfaction questionnaire-8 (CSQ-8) assessed patient satisfaction. Semi-structured interviews were conducted with supervisors.
Setting: Gustavsberg PHC Center, Stockholm County, Sweden.
Subjects: Students in medicine, nursing, physiotherapy, occupational therapy and psychology and their patients filled in questionnaires. Supervisors in medicine, nursing and physiotherapy were interviewed.
Main outcome measures: Mean values and medians of CLES + T and CSQ-8 were calculated. Interviews were analyzed using content analysis.
Results: A majority of 199 out of 227 student respondents reported satisfaction with the pedagogical atmosphere and the supervisory relationship. Most of the 938 patient respondents reported satisfaction with the care given. Interviews with 35 supervisors showed that the organization of the SRC provided time and support to focus on the tutorial assignment. Also, the pedagogical role became more visible and targeted toward the student’s individual needs. However, balancing the student’s level of autonomy and the own control over care was described as a challenge. Many expressed the need for further pedagogical education.
Conclusions: High student and patient satisfaction reported from five disciplines indicate that a SRC in PHC can be adapted for heterogeneous student groups. Supervisors experienced that the SRC facilitated and clarified their pedagogical role. Simultaneously their need for continuous pedagogical education was highlighted. The SRC model has the potential to enhance student-centered tuition in PHC.
Knowledge of student-run clinics (SRCs) as learning environments within standard primary health care (PHC) is limited.
We report experiences from the perspectives of students, their patients and supervisors, representing five healthcare disciplines.
Students particularly valued the pedagogical atmosphere and the supervisory relationship.
Patients expressed high satisfaction with the care provided.
Supervisors expressed that the structure of the SRC supported the pedagogical assignment and facilitated student-centered tuition – simultaneously the altered learning environment highlighted the need for further pedagogical education.
Student-run clinics in primary health care have great potential for student-regulated learning.
Key Points
Introduction
To meet the demands of present and future health care, students have to understand and be able to navigate and interact with the system in which they will practice [Citation1]. To an increasing extent, this system and context are primary health care (PHC). Most healthcare educations currently include clinical placements in PHC settings.
Student-run clinics (SRCs) are increasingly used in order to provide active learning opportunities in authentic settings [Citation2,Citation3]. The organization of SRCs varies, but one thing they have in common is that the student acts as the main provider of care, with support from the clinical supervisor [Citation2,Citation4]. Students at SRCs report an increased sense of patient ownership, as they take the lead position in terms of systems navigation and problem-solving [Citation1,Citation2]. Previous SRCs in Sweden have mainly focused on inter-professional education and collaboration in hospital-based settings [Citation5–8]. Studies of student-run inter-professional wards show that the students developed professional and collaborative skills [Citation5,Citation6].
SRCs outside hospitals have been operated since the late 1960’s, mainly in the United States, within various settings (e.g. PHC, churches and shelters) [Citation2,Citation9,Citation10]. In PHC, the SRCs are often found in the context of free health care services for populations with limited access to regular health care [Citation2]. Other initiatives have addressed selected populations such as older people [Citation11].
Clinical supervisors sometimes experience tutoring in combination with their own clinical practice as challenging, since the task requires simultaneous responsibility for patient care and facilitation of the student’s learning process [Citation12,Citation13]. SRCs are learning environments where supervisors need to adapt their clinical teaching, striving to achieve an increased level of student-centered tuition [Citation4]. The patient satisfaction and quality of care have been perceived to be comparable to that of regularly provided care [Citation2]. Patient-reported benefits from receiving care within SRCs have been described, such as improved coping strategies [Citation11], a higher degree of shared decision-making and a higher degree of satisfaction with provided information [Citation7].
Few studies have explored the SRC model as a pedagogical learning environment within ordinary PHC. Our aim was to explore how a SRC in PHC was perceived by the students, patients and clinical supervisors.
Material and methods
Context
The study was conducted at Gustavsberg PHC in Stockholm County, Sweden, a PHC providing care for over 30,000 inhabitants. The unit participates in primary health care education for students in medicine, nursing, physiotherapy, occupational therapy and psychology. The rationale for the development of a SRC was to increase the capacity to receive students, to create an active learning environment, and to stimulate inter-professional learning.
The decision to implement the SRC was well anchored in the management of the PHC and a dedicated team of five persons from different healthcare professions developed the routines of the SRC. During this preparatory stage, which lasted about one year, room facilities of the PHC were partly reconstructed to fit the SRC model. The SRC was opened in the autumn of 2013 for public care provided by students in medicine, nursing, physiotherapy and occupational therapy, under supervision. In autumn 2014, psychology students were introduced at the SRC.
At the time of the study, students in physiotherapy and occupational therapy at the SRC were mostly in their second to fifth and first semester, respectively. Students in medicine and nursing had completed at least half of their educational program. The length of the placement varied between the educational programs, from one week for most medical students to 13 weeks for psychology students.
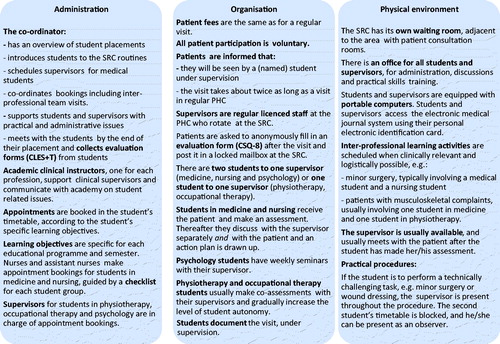
Patients were recruited to the SRC while seeking care through the central booking system at the PHC. The booking routine was standardized by use of a checklist: the patient agreed to receive care from a student under supervision, adequate time was allocated for the appointment (usually twice as long as a regular visit), and the reason for the encounter targeted intended learning outcomes of the educational program for the student. A majority of eligible patients accepted the offer to have their appointment at the SRC. There were variations in routines and supervision models between professions ().
Data collection
Students’ evaluation
In year 2014 and 2015, all students at the SRC were asked to anonymously fill in pre-selected parts of the clinical learning environment, supervision and nurse teacher evaluation scale (CLES + T), by the end of their clinical placement [Citation14,Citation15]. The CLES + T has demonstrated good psychometric properties including high reliability [Citation15,Citation16]. In alignment with the use of the instrument within the primary care section of the medical program, Karolinska Institutet, pre-selected sections focusing on three dimensions of the learning environment were used:
Pedagogical atmosphere (items 1–9: the atmosphere at the workplace, including whether the staff was easy to approach, whether one felt comfortable at the unit, the staff’s interest in student supervision, opportunities for meaningful and multi-dimensional learning). Item 3 (‘During staff meetings I felt comfortable taking part in the discussions.’) was omitted since most students did not participate in staff meetings.
Premises of care at the unit (items 14–17: the clarity of the description of the unit’s care philosophy, provision of individualized care, clarity of communication and documentation).
Supervisory relationship (items 18–25: the supervisor’s attitude to supervising, provision of individual supervision, continuous feedback, general satisfaction with supervision, equality in the supervisor-student relationship, mutual interaction in the supervisory relationship, respect and understanding in the supervisor-student relationship and trust between the supervisor and the student).
Each item included a positive statement about the learning environment. Students responded according to the pre-formulated response options, graded one to five, with five indicating the highest degree of satisfaction. The omitted subscales (regarding leadership style of the ward manager and role of the university teacher) were deemed to be irrelevant for the SRC placement for most students. Students were asked to specify their educational program. Average rating (mean), median and ranges were calculated for each learning environment dimension, for all students and per student category ().
Table 1. The results of the students’ evaluation, using pre-selected sections of the clinical learning environment, supervision and nurse teacher evaluation scale, are shown.
Patients’ evaluation
The Client Satisfaction Questionnaire 8 (CSQ-8) was chosen since it has been shown to have good psychometric properties including high reliability (Cronbach’s α = 0.93), good construct validity [Citation17], and that factor analysis has demonstrated that the eight items of the scale load on a general satisfaction factor [Citation18].
Evaluation forms and brief written information notes were available in the waiting room, and patients were encouraged to fill out the form anonymously and to post it in a locked mailbox at the SRC. The CSQ-8 includes eight questions about satisfaction: perceived quality of care, satisfaction with the form of care provided, whether the care responded to needs, whether one would recommend the unit to a friend with a similar need, satisfaction with the extent of help provided, whether the care led to better coping strategies, general satisfaction with the care given and whether one would seek care at the unit again. A criterion specified grading scale from one to four was used. Four indicated the highest degree of satisfaction. Patients could also add free text comments to each question. If a series of visits for treatment and/or consultation was planned, as was often the case for patients seeing students in physiotherapy, occupational therapy and psychology, the patient was asked to fill in the form when the series was finished.
During the year 2013 and 2014, patient evaluation forms were collected consecutively. Respondents were asked to specify what professional category they had met, and if they were seen by more than one professional category, i.e. an inter-professional student team.
Response rates were calculated from CSQ-8 data and clinic visit numbers for medical students and nursing students. For students in physiotherapy, occupational therapy and psychology, response rates could not be calculated since booking routines differed and specific patient visit data could not be extracted. Moreover, these patients were often seen in a series of visits.
An effort was made to increase the response rate during two predefined time periods, April to May 2015, and during three weeks in October 2015. During these periods, a designated assistant nurse attended the SRC daily and encouraged patients to fill out the CSQ-8.
To further clarify the patients’ experiences, two questions were added in 2015:
What worked well at the student-run clinic?
What could have been done differently and better?
Data analysis
Questionnaire data were analyzed using STATA14® (StataCorp, College Station, TX). There were one or more missing values in 132 (14%) of the QSQ-8 questionnaires and in 26 (13%) of the CLES + T questionnaires. Missing values were replaced by item specific mean values (all responders).
Average ratings of the CLES + T were compared section-wise between student categories (). Highest and lowest rated item per student category were identified. Total scores of the CSQ-8 were compared regarding total score and type of visit (). CSQ-8 results were also compared regarding gender (female, male and unspecified) and age (<18 years, 18–64 years, >65 years and unspecified). To estimate whether patient satisfaction was associated with data loss we compared the time periods with the highest and lowest response rates for visits to medical and nursing student, respectively. Differences were tested for statistical significance using Kruskal–Wallis rank test if more than two groups were compared. Pairwise comparisons were made using Wilcoxon rank-sum test. Differences were considered to be statistically significant at a confidence level of 95%.
Table 2. The results of the patients’ evaluation using the client satisfaction scale 8 are shown.
The two additional questions (see the end of section Patients’ evaluation) were given to 209 out of 300 patients during the limited time frame in 2015 (91 patients accidentally received the old questionnaire). The analysis of free text comments from CSQ-8 and answers to question 1) and 2) was made according to content analysis [Citation19].
All free text answers and comments were read repeatedly for global understanding.
The comments were organized according to questions 1) and 2).
Meaning units were identified.
Categories were established.
An effort was made to establish categories that included all aspects in relation to question 1) and 2), and not only those that were frequently expressed.
Supervisors’ views
Interviews with clinical supervisors were conducted in 2014 to capture supervisors’ views regarding their role as a supervisor at the SRC, in comparison with their tuition in ordinary practice. Thirty-five clinical supervisors (23 physicians, seven nurses and five physiotherapists) participated in the study. No supervisor declined to participate in the study. Psychologists were not interviewed for this study since the first psychology students started their placements after the interviewing period had ended. For logistical reasons, four supervisors including two physicians, one occupational therapist and one nurse were not interviewed. All interviewees received written and oral information about interviews and all provided written informed consent.
The interviews were conducted by an inter-professional group of team members (TS, CL, MF and BF). Interviews were organized to avoid dependence or other disturbing relationships between interviewer and interviewee. Physicians were interviewed by TS and CL, nurses by MF and physiotherapists by BF. All interviews were held face-to-face and recorded, at Gustavsberg PHC. A semi-structured interview guide was used. Interviews were transcribed and analyzed according to content analysis [Citation19]. All transcripts were read by CL and KB whereas the other interviewers read several transcripts from interviews with supervisors from each discipline (medicine, nursing and physiotherapy). CL and KB performed the analysis, and all interviewers participated in discussions along the process.
The process of analysis can be described as follows:
Interviews were listened to and read repeatedly for global understanding.
Meaning units were identified.
The meaning units were condensed, coded and sorted into categories.
The categories were interpreted into themes.
Consensus on main themes was reached within the group through repeated discussions.
Member checking was conducted as findings were presented to the participants at morning meetings with each profession, as an opportunity for interviewees to reflect and provide feedback. Generally, participants agreed with the outcome of the analysis and their feedback did not alter the result.
Results
Students’ evaluations
From January 2014 to June 2015, 229 students performed clinical placements at the SRC. The survey response rate was 87% overall and was highest for nursing students and lowest for medical students ().
There were some small but statistically significant differences between groups (). For the dimension Pedagogical atmosphere, the nursing students and unspecified students had somewhat lower results than the other groups. Regarding the dimension relationship student-supervisor medical students scored somewhat higher than other student categories.
Patients’ evaluations
A total of 938 questionnaires were collected ().
The mean age of responders in the questionnaire was 54 years (range 5–94 years); 52% were women, 37% men and 11% did not specify their gender. Evaluations reflected a high level of satisfaction (). CSQ-8 scores were similar between caregiver professions, and also between genders. Patients >65 years of age scored slightly higher than others (mean CSQ-8 scores for patients: <18 years, 29.99; 18–64 years, 30.04; >65 years, 30.59 and unspecified, 29.95, p = .01).
The response rate for patients who were seen by medical students varied between 14% (in 2014) and 61% (autumn 2015). For patients who had seen nursing students, response rates were generally low (from 3% in 2014 to 30% in spring 2015). There was no significant difference in mean CSQ-8 score between the time period with the highest and lowest response rates (p = .11 for visit to medical student and p = .33 for visit to nursing student), indicating that the impact of data loss on patient satisfaction estimates was limited.
Free text comments from patients
One hundred and ninety patients provided comments on the original CSQ-8 form, and an additional 209 patients received questions 1 and 2 attached to the CSQ-8 form, of whom 196 answered question 1 and 155 answered question 2.
1. What worked well at the student-run clinic?
Well received. Patients described that they were listened to and addressed in a respectful, friendly and calm way. Patients pointed out that they felt they were paid interest to, taken seriously and felt understood.
Perceived high quality of care. Patients felt that they were given enough time, were well examined and received answers to their questions. Many perceived that the level of knowledge and professionalism was high among students and supervisors. Several patients pointed out that they were invited to discuss treatment options and plan of actions. Some expressed that they perceived that the clinical assessment was improved by being seen by both the student and the clinical supervisor.
Adequate organization. Many appreciated the extra time given for the consultation and felt less stressed. Some also expressed that they appreciated a short waiting time for an appointment and the punctuality during their visit.
2. What could have been done differently and better?
Many expressed a high level of satisfaction and had no suggestions for improvements. Two areas for improvement were, however, identified:
Need of information. Some patients felt insufficiently informed about how the SRC was organized regarding the provided care, and experienced that the process took too much time, since they were to see both the student and the supervisor. A few patients expressed dissatisfaction and lacked information regarding prolonged visit, since they had to wait in between seeing the student and the supervisor.
Insecurity among students. Some patients found that the student seemed to feel insecure in the caregiver role.
Supervisors’ experiences
All supervisors had previous experience of tuition in clinical education and had received at least brief formal pedagogical education.
Supervisors perceived that there were differences in supervising at the SRC compared with supervision in their ordinary practice. Four overarching themes (1–4) were identified:
Organization, structure and administration
Tuition as a pedagogical entity
Control over provided care
Reflection on professional and pedagogical competence
1. Organization, structure and administration
The respondents stated that the organization, the structure for provided care and the educational perspective within the administration of the SRC () facilitated the pedagogical assignment. It gave practical support and time for supervisors to focus on clinical supervision and workplace-based assessment including student feedback. The organization, structure and administration were also thought to facilitate student-centered supervision and clarified the differences between different supervisory models among the clinical supervisors.
The extra space, with one room per student and one room for supervisors, made it possible for students to manage the patient encounter at a level of autonomy that was suitable according to the situation and the student’s knowledge, with support from the supervisor:
At the SRC there are prerequisites to be a good supervisor, there is time. There are good conditions for the student to be independent. (Nurse)
I have to say that there is much less stress at the SRC…one gets to focus on the supervisor role. (Physician)
Many felt that the organization, structure and administration improved the possibilities for inter-professional meetings and collaboration between students and supervisors:
It opens up the possibility for the student to meet with other students… with other professions and how you can cooperate, and work with inter-professional education. (Physiotherapist)
2. Tuition as a pedagogical entity
Respondents described that the pedagogical content of the tutorial assignment was highlighted by supervising in a setting separated from the everyday practice. Some thought the pedagogical role became more visible when supervising at the SRC than in the supervisor’s regular consultation room, and the tendency to use a more traditional master-apprentice approach became weaker. Interviewees suggested that there was an increased focus on student’s learning at the SRC.
The supervisor’s responsibility for the care given, as a part of the pedagogical assignment, was often clarified when supervising at the SRC, and emphasized the need to balance the role of being a supervisor with the caregiver role. Supervisors felt they had to meet new requirements in their role as a supervisor to adapt to the new supervisory style.
The longer time allotted for the student-led consultation was described as a prerequisite to create a student-centered learning opportunity. Supervisors suggested that the student was given the opportunity to practice to perform the entire or parts of the patient consultation, based on their own level of knowledge and the specific learning objectives and that the student’s own needs guided both the content and the level of interaction in supervision:
Yes, I believe that I have more time to engage in my role… even if you always try to but it is… it is different. It is quieter and I have more time to engage in the subject, I have time to look things up before so that I know what they are studying and what they are supposed to focus on and so forth. (Physician)
I step back and let the students do most of the work then I join them as a consultant. (Nurse)
I let the students reason, reflect, what do you learn from this, see different perspectives. (Physician)
I have had to learn to step back and practice restraint. (Physiotherapist)
3. Control over provided care
Respondents expressed that their perceived need for clarity and visibility of the students’ knowledge, attitudes and skills became more marked in the setting. Previous experience from working in health care and other healthcare educations were assigned varying degrees of importance in different supervisory professions:
I want to know if they have worked within care before, what they have done. What semester they are studying, what they want to learn. What they feel they are less good at… is good to know. Then you can help them with these things that they want to practise. But above all it says a lot if they have worked within care before. If they have not, then they might need more supervision too. And that you are with them a lot more… (Nurse)
The student leads the work, collects the patient and talks with the patient… Then I come in and the student summarizes what they have discussed, and then I want the patient to have a say. (Physician)
Supervisors experienced that they needed to find a balance between the student’s level of autonomy and their own need for control. They said that it was sometimes difficult to stand back and not take over the patient encounter:
Then again it’s about control… And I guess that you are different about that and I believe that me as a person, I like to be in control. So you really need to challenge yourself, and at the same time you need to find that balance. So that it is still patient safe and, well. That is it, the difficult part. And sometimes you are in a good flow and sometimes it is more difficult… (Nurse)
It is important that you dare to leave the patient with the student…That you feel that you have confidence in the student. (Physiotherapist)
In order to ensure medical quality and patient safety, supervisors in the SRC setting more often had introductory conversations with the students. Previous experiences and specific wishes prior to placement, i.e. specific areas of desired improvement, were identified.
4. Reflection on professional and pedagogical competence
Respondents expressed that since the pedagogical role in the tutorial assignment was clarified at the SRC, the supervisors’ focus on their own pedagogical role was increased. Many expressed an increased need for continuous professional development and training in clinical supervision, in order to develop their own role as a tutor. There was also a need to reshape the structure of supervision since the form of clinical placements at the SRC was altered.
Supervisors said they became more conscious of students’ different needs in learning. This identified the need for pedagogical knowledge and skills, and the competence to alter tutorial methods:
We have had to develop our own supervisor role, but we lack pedagogical instruments. (Physician)
I think it is important that if you will be a supervisor at the SRC you should have training. (Physiotherapist)
Discussion
Principal findings
A majority of 199 out of 229 students reported satisfaction with the learning environment, in particular regarding the pedagogical atmosphere and the supervisory relationship. The feedback obtained from students indicated that the SRC concept was valued by students from all five disciplines included in the study.There were only small differences between student categories.
Most of the 938 patient respondents, reported satisfaction with the care provided. Patients expressed that they were well received, perceived that the quality of care was high, and that the SRC was well organized. From a patient safety perspective, it is important to note that students were supervised by licensed clinicians, responsible for the care given.
Being a clinical supervisor in the SRC context, which is separated from the routine clinical setting, clarified the supervisors’ teaching role. Supervisors perceived that the organization of the SRC provided time and support to focus on the pedagogical assignment. The structure of the SRC facilitated supervision targeting the student’s individual needs. Finding a balance between the student’s level of autonomy and perceived need of own control over care was described as a challenge. Supervising in this context highlighted the need for continuous pedagogical education for clinical supervisors.
Strengths and weaknesses of the study
A central strength of the study was that the SRC was explored from the perspective of students and supervisors, from five health care disciplines, and their patients.
Adequate measures have been taken to assure validity of our results. We used established instruments for data collection in combination with a mixed methods approach including both quantitative and qualitative data, which offered opportunities for data triangulation. Interviews were conducted and analyzed by an inter-professional group of researchers, which reduced the risk of bias since several perspectives were represented. Moreover, member check with respondents was conducted.
One important question is whether a SRC is of value for students from different health care educations; our results show overall high ratings and only small differences between student groups. As shown by the results from the qualitative analyses of the supervisors’ view, each main theme in terms of strengths of the SRC was grounded in statements from supervisors of different disciplines and there were generally small between-profession variations in the perception of the SRC.
Limitations included that the results were not specifically compared with clinical placements within the ordinary clinic at Gustavsberg PHC, and the study should be considered as exploratory and descriptive.
Interviewing supervisors rather than students and patients were prioritized, since the knowledge about supervisors’ experiences of the SRC model is scarce. Supervisors in occupational therapy and psychology could not be interviewed for this study due to logistical reasons. An important venue for future research is to investigate their perceptions of strengths and weaknesses of the SRC.
The Swedish translation of the CSQ-8 is an established tool in research and development; however, a limitation is the lack of validation studies of the questionnaire in a Swedish context. Moreover, the patients’ evaluation response rate was low (), and could not be calculated for patients of all caregiver categories because of different routines between professions, see Methods section. These results should, therefore, be interpreted with caution.
Findings in relation to other studies
The double role of supervisors, as the responsible caregivers, ensuring the quality of provided care, and as clinical supervisors was illustrated by the interview results. The importance of a supportive context, including having enough time, has been described previously [Citation12,Citation20,Citation21]. In this study, a closer supervisory relationship with a more targeted communication was described as a condition to allow the student to practice on various levels of independence, under supervision. This made it possible for students to carry out parts of or the entire consultation, with supervision targeting the student’s own need for guidance [Citation1,Citation13,Citation20].
High student satisfaction and an improved understanding of their own roles and other health care professionals’ roles have been reported from SRCs [Citation2,Citation3,Citation5,Citation6,Citation8,Citation10,Citation22,Citation23]. However, it is difficult to make direct comparisons with other studies since there has been a diversity of contexts in which SRCs have been evaluated and the methods used for evaluation vary. This study explores an SRC in everyday PHC, and not specific target groups, such as populations with limited access to medical care, as is the case with most previous research in the field.
Students in Sweden generally rate their clinical placements positively [Citation14,Citation24]. However, one previous study suggested that nursing students experienced that there were fewer meaningful learning situations in PHC compared to hospital-based settings [Citation24]. In light of this, we find our results, which indicated high student satisfaction on all items of the CLES + T () across all health care professions, as encouraging.
Patient satisfaction and perceived quality of care comparable to that of regular care have previously been reported in studies from SRCs [Citation2,Citation7,Citation11]. The overall mean CSQ-8 score in our study was 30.20 out of 32, indicating a high level of satisfaction with care ().
Implications for health care and research
As shown by previous research, active learning in clinical contexts can improve student outcomes [Citation25–27].
The structure and routines of the SRC made it possible for students to carry out parts of or the entire consultation, with supervision targeting the student’s own need for guidance [Citation1,Citation13,Citation20]. A student-centered approach in clinical supervision has been identified as an important aspect regarding the student’s professional development [Citation12,Citation20,Citation21]. Further studies are needed to clarify the student’s learning process at SRCs, in order to identify models for student-regulated learning, including methods for self- and teacher-assessment.
This study highlights that clinical supervisors’ professional framework is of importance for the experience of clinical teaching and supervision. Our experience is that in order for an SRC to be successful, the management of the SRC needs to fully support the implementation and a project group with representation from the all concerned professions needs sufficient time to develop the procedures of the SRC. The experience at the SRC in Gustavsberg showed that an extended level of student-centered tuition calls for an increased need for pedagogical education for supervisors.
Although the SRC model in this study was designed to improve students’ clinical learning environment, it was intended to be neutral in terms of productivity in comparison to standard clinical placements. In spite of the well-organized workflow and administrative and practical support, the productivity was somewhat lower (in terms of number of clinic visits) at the SRC than at the regular clinic. Having enough time for patient care and student supervision was deemed necessary to maintain educational quality and patient safety. Moreover, the structure of the SRC requires additional resources in terms of room facilities and administrative staff.
The SRC model for clinical PHC placements is a promising model in which students, on the basis of their own theoretical and clinical knowledge, under supervision, can be integrated into ordinary clinical practice. The academic assignment of supervision and clinical teaching needs to be anchored in continuous pedagogical training and education in order to promote a more student-centered tutorial approach in PHC education.
Conclusion
High student and patient satisfaction reported from five disciplines indicate that a SRC in primary care can be adapted for heterogeneous student groups. Supervisors expressed that the structure of the SRC clarified the teacher role, supported them in their pedagogical assignment and facilitated student-centered tuition. Simultaneously, they felt that the altered learning environment highlighted the need for further pedagogical education. Student-run clinics in primary health care have great potential for enhanced student-centered tuition.
Ethical considerations
This work was considered to be a local service evaluation and development project, and this judgment was confirmed by an independent ethical review board in Stockholm, reference number 2014/1684-31/5.
Notes on contributors
Maria Fröberg MD, PhD and resident in Family Medicine at Gustavsberg PHC and Department of Neurobiology, Care Sciences and Society, Karolinska Institutet Stockholm, Sweden.
Charlotte Leanderson MD, PhD, specialist in Family Medicine at Segeltorp PHC, Stockholm, Sweden. Clinical lecturer and affiliated researcher at the Department of Neurobiology, Care Sciences and Society, and the Department of Learning, Informatics, Management and Ethics, both Karolinska Institutet.
Birgitta Fläckman Registered Nurse, PhD and senior lecturer at Department of Care Sciences, Ersta Sköndal Bräcke University College, Stockholm, Sweden.
Erik Hedman-Lagerlöf Licensed psychologist and psychotherapist, Associate Professor, Gustavsberg PHC and Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden.
Karin Björklund Licensed occupational therapist, PhD student and academic clinical instructor at the Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden.
Gunnar H. Nilsson MD, Professor, specialist in Family Medicine at the Department of Neurobiology, Care Sciences and Society, Stockholm, Sweden.
Terese Stenfors Associate Professor of Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Stockholm, Sweden.
Acknowledgments
The authors wish to acknowledge Kersti Ejeby, Gustavsberg PHC Center, who made this project possible through her foresight and vision. We would also like to thank current and previous academic clinical instructors Åsa Spångberg, Helena Almer, Helene Kruse, Nanna Gautier, Ulrica Wedholm, Annika Pettersson, Tommy Engström and Karoline Kolaas and SRC coordinator and assistant nurse Annika Eriksson for valuable discussions and collaboration. Moreover, we thank Axel C. Carlsson, Karolinska Institutet, for advice and discussions on statistical analysis and presentation. We also wish to express our gratitude to Maria Blomqvist, previous controller at Gustavsberg PHC Center, for assistance with retrieving clinic visit data.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Meah YS, Smith EL, Thomas DC. Student-run health clinic: novel arena to educate medical students on systems-based practice. Mt Sinai J Med. 2009;76:344–356.
- Schutte T, Tichelaar J, Dekker RS, et al. Learning in student-run clinics: a systematic review. Med Educ. 2015;49:249–263.
- Sheu L, O’Brien B, O’Sullivan PS, et al. Systems-based practice learning opportunities in student-run clinics: a qualitative analysis of student experiences. Acad Med. 2013;88:831–836.
- Teherani A. On autonomy in student-run clinics. Med Educ. 2015;49:238–239.
- Ericson A, Masiello I, Bolinder G. Interprofessional clinical training for undergraduate students in an emergency department setting. J Interprof Care. 2012;26:319–325.
- Hallin K, Kiessling A, Waldner A, et al. Active interprofessional education in a patient based setting increases perceived collaborative and professional competence. Med Teach. 2009;31:151–157.
- Hallin K, Henriksson P, Dalén N, et al. Effects of interprofessional education on patient perceived quality of care. Med Teach. 2011;33:e22–e26.
- Hylin U, Lonka K, Ponzer S. Students’ approaches to learning in clinical interprofessional context. Med Teach. 2011;33:E204–EE10.
- Buckley E, Vu T, Remedios L. The REACH project: implementing interprofessional practice at Australia’s first student-led clinic. Educ Health. 2014;27:93–98.
- Riddle MC, Lin J, Steinman JB, et al. Incorporating the principles of the patient-centered medical home into a student-run free clinic. Adv Med Educ Pract. 2014;11:289–297.
- Kent F, Keating J. Patient outcomes from a student-led interprofessional clinic in primary care. J Interprof Care. 2013;27:336–338.
- Hallin K, Danielson E. Being a personal preceptor for nursing students: registered Nurses’ experiences before and after introduction of a preceptor model. J Adv Nurs. 2009;65:161–174.
- Von Below B, Haffling AC, Brorsson A, et al. Student-centred GP ambassadors: perceptions of experienced clinical tutors in general practice undergraduate training. Scand J Prim Health Care. 2015;33:142–149.
- Johansson UB, Kaila P, Ahlner-Elmqvist M, et al. Clinical learning environment, supervision and nurse teacher evaluation scale: psychometric evaluation of the Swedish version. J Adv Nurs. 2010;66:2085–2093.
- Saarikoski M, Isoaho H, Warne T, et al. The nurse teacher in clinical practice: developing the new sub-dimension to the clinical learning environment and supervision (CLES) scale. Int J Nurs Stud. 2008;45:1233–1237.
- Ohman EA, Alinaghizadeh H, Kaila P, et al. Adaptation and validation of the instrument clinical learning environment and supervision for medical students in primary health care. BMC Med Educ. 2016;16:308.
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5:233–237.
- Brey D. A cross-national validation of the client satisfaction questionnaire: the Dutch experience. Eval Program Plann.1983;6:395–400.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112.
- Hauer KE, Oza SK, Kogan JR, et al. How clinical supervisors develop trust in their trainees: a qualitative study. Med Educ. 2015;49:783–795.
- Kaufman DM. ABC of learning and teaching in medicine-applying educational theory in practice. BMJ. 2003;326:213–216.
- Clark DL, Melillo A, Wallace D, et al. A multidisciplinary, learner-centered, student-run clinic for the homeless. Fam Med. 2003;35:394–397.
- Smith SD, Johnson ML, Rodriguez N, et al. Medical student perceptions of the educational value of a student-run free clinic. Fam Med. 2012;44:646–649.
- Bisholt B, Ohlsson U, Engstrom AK, et al. Nursing students’ assessment of the learning environment in different clinical settings. Nurse Educ Pract. 2014;14:304–310.
- Rich SK, Keim R, Shuler CF. Problem-based learning versus a traditional educational methodology: a comparison of preclinical and clinical periodontics performance. J Dent Educ. 2005;69:649–662.
- Dornan T, Boshuizen H, King N, et al. Experience-based learning: a model linking the processes and outcomes of medical students’ workplace learning. Med Educ. 2007;41:84–91.
- Graffam B. Active learning in medical education: strategies for beginning implementation. Med Teach. 2007;29:38–42.