To the Editor
Granular cell tumors (GCT) are uncommon benign tumors. They may occur in various sites. The tongue and breast comprise the two most common locations, while a lesion in the digestive and respiratory tracts is not unusual. Laryngeal involvement is fairly uncommon and is present in approximately 10% of all cases Citation[1]. Malignant GCTs represent less than 2% of all granular cell tumors Citation[2]. As with their benign counterparts, malignant GCT have a wide anatomic distribution. However, they carry a poor prognosis, with recurrence and metastasis typically within one year of diagnosis Citation[3].
We present a case of malignant granular cell tumor arising from larynx, which has metastasized to lungs and bones. We also conducted a search on the MEDLINE database (National Library of Medicine, Bethesda, MD) and identified 52 previously reported cases of metastatic GCT whose survival data were reported. Basic characteristics of these cases together with ours are described in the following sections. We also review the metastatic GCT in literature.
Case Report
A 43-year-old woman was admitted to the hospital for long-standing cough and recent hemoptysis. In her past history, she had undergone right vertical laryngectomy in another institution two years ago. The diagnosis was laryngeal GCT. Physical examination was unremarkable except for decreased breath sounds in the apex of the right lung. Chest x-ray revealed infiltration of right upper lung region. Computed tomography (CT) of the thorax showed mediastinal lymphadenopathies as well as a lesion that partially obstructed the upper lobe bronchus and invaded the inferior vena cava. Bronchoscopy revealed a bright, smooth and vascularized mass, obstructing the right upper lobe entrance. Punch biopsy was performed. Histopathological examination showed a GCT. The lesion appeared inoperable due to the invasion of large vessels. Ultrasound and CT of the abdomen showed a giant hemangioma in the right lobe of the liver. This finding was confirmed by biopsy. Sixty Gy of external radiotherapy was administered to the pulmonary lesion. This intervention resulted in the palliation of hemoptysis, but the size of the lesion remained stable. As no other effective treatment modality was available, a decision to administer chemotherapy was made. She received three cycles of cisplatin and fluorouracil. Toxicity was acceptable, however, the pulmonary lesion remained unchanged while multiple osteoblastic lesions appeared on direct x-rays and radionuclide bone scan. Chemotherapy was discontinued, and she was given radiotherapy to the right distal femur for pain palliation. Oral etoposide 50 mg/day was prescribed, but patient could not tolerate and refused to use it after only ten days of treatment.
On her last visit 24 months after the detection of metastatic disease, she is in good health and symptom-free except for mild pain of the right femur that responds well to paracetamol. She has not been given any specific treatment since 12 months.
Discussion
GCT is almost always benign. However, a malignant course is encountered in 2% of cases. Differentiation between benign and malignant GCTs is often difficult, and only the development of metastases may ultimately establish malignancy Citation[3]. Because malignant GCTs are extremely rare, an effort has been made to identify specific features that would predict malignant behavior. Based on the cumulative experience of previous case reports of malignant GCTs, six histologic criteria are considered to be important Citation[4]. These include spindling of the tumor cells, the presence of vesicular nuclei with large nucleoli, increased mitotic rate (>2 mitoses/10 high-power fields at 200x magnification), a high nuclear to cytoplasm ratio, pleomorphism, and necrosis Citation[5]. Histologically, malignant GCT is diagnosed when three or more of the six criteria are fulfilled. In addition to these morphological features, upregulation of p53 as well as Ki-67, a nuclear proliferative marker, has been recently found to correlate with an aggressive clinical course and malignant behavior. In a recent study, p53 immunostaining was negative in all benign cases, while p53 expression was seen in greater than 10% of the cell population in 21 of 25 (79%) malignant GCTs. Similarly, benign GCTs showed immunoreactivity of Ki-67 in 1% or less of the tumor cell population, while fourteen of 25 (56%) malignant tumors had Ki-67 immunoreactivity in up to 30% of the cell population Citation[3]. Clinical characteristics like size larger than 5 cm, multicentricity, rapid growth, and recurrent disease may also increase the likelihood of malignant behavior.
We searched PubMed for metastatic GCT and summarized some clinical characteristics of 53 cases in . Metastatic GCT is more commonly seen in women with a female to male ratio being 2.5:1 (n = 38/15). Patient age at presentation ranges from 17 to 72 with the median age at diagnosis being 43 years.
Table I. Clinical features of metastatic granular cell tumor cases.
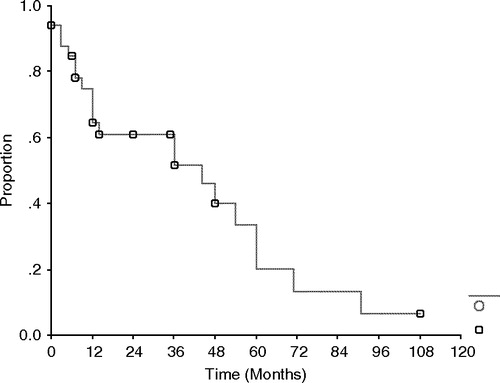
Almost all patients have been treated surgically at diagnosis. Most metastases develop within two years following diagnosis. Median disease free survival was 17 months (95% confidence interval [CI]: 13–21). Most frequently affected sites are the lungs, liver and bones. Other frequently involved site was local lymph nodes. The majority of these metastases were associated with local recurrences (n = 21/53; 40%). Median overall survival from diagnosis was 84 months (95% CI: 46–122). Median overall survival after the detection of metastases was 44 months (95% CI: 11–76, ).
It may be concluded that patients who have undergone surgical resection for GCT should be followed up closely at least during the first 2 years, especially if unfavorable histological features are present. In case metastases develop, surgical resection should be attempted whenever feasible, because neither radiotherapy nor chemotherapy appear particularly effective. Chemotherapy has been given to several cases, but no effective agent has emerged, and currently chemotherapy should be reserved only for very selected patients.
References
- Chiang MJ, Fang TJ, Li HY, Chen IH, Lee KF. Malignant granular cell tumor in larynx mimicking laryngeal carcinoma. Am J Otolaryngol 2004; 25(4)270–3
- Budino-Carbonero S, Navarro-Vergara P, Rodriguez-Ruiz JA, Modelo-Sanchez A, Torres-Garzon L, Rendon-Infante JI, et al. Granular cell tumors: Review of the parameters determining possible malignancy. Med Oral 2003; 8(4)294–8
- Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol 1998; 22(7)779–94
- Polivka M, Wassef M, Lot G, Herman P, Marsot Dupuch K, Prudhomme De Saint Maur P, et al. [A palate tumor revealed by pain]. Ann Pathol 2002; 22(4)324–7
- Khansur T, Balducci L, Tavassoli M. Granular cell tumor. Clinical spectrum of the benign and malignant entity. Cancer 1987; 60(2)220–2
- Yang SW, Hong SW, Cho MY, Kang SJ. Malignant granular cell tumor at the retrotracheal space. Yonsei Med J 1999; 40(1)76–9
- Callejo SA, Kronish JW, Decker SJ, Cohen GR, Rosa RH, Jr. Malignant granular cell tumor metastatic to the orbit. Ophthalmology 2000; 107(3)550–4
- Di Tommaso L, Magrini E, Consales A, Poppi M, Pasquinelli G, Dorji T, et al. Malignant granular cell tumor of the lateral femoral cutaneous nerve: report of a case with cytogenetic analysis. Hum Pathol 2002; 33(12)1237–40
- Berg JC, Tewari KS, Del Rosario R, Berman ML. Unusual presentation of a malignant granular cell tumor of the pelvis: case report and literature review. Gynecol Oncol 2003; 90(1)224–30
- Schmidt O, Fleckenstein GH, Gunawan B, Fuzesi L, Emons G. Recurrence and rapid metastasis formation of a granular cell tumor of the vulva. Eur J Obstet Gynecol Reprod Biol 2003; 106(2)219–21
- Stiegler-Giec R, Wittekind C, Schutz A, Haupt R, Wiechmann V, Gillissen A. [Pulmonary and pleural metastasis of a malignant granular cell tumor]. Dtsch Med Wochenschr 2002; 127(17)923–6
- Gartmann H. [Malignant granular cell tumor]. Hautarzt 1977; 28(1)40–4
- Simsir A, Osborne BM, Greenebaum E. Malignant granular cell tumor: a case report and review of the recent literature. Hum Pathol 1996; 27(8)853–8
- Parayno PP, August CZ. Malignant granular cell tumor. Report of a case with DNA ploidy analysis. Arch Pathol Lab Med 1996; 120(3)296–300
- Shimamura K, Osamura RY, Ueyama Y, Hata J, Tamaoki N, Machida N, et al. Malignant granular cell tumor of the right sciatic nerve. Report of an autopsy case with electron microscopic, immunohistochemical, and enzyme histochemical studies. Cancer 1984; 53(3)524–9
- Klima M, Peters J. Malignant granular cell tumor. Arch Pathol Lab Med 1987; 111(11)1070–3
- Uzoaru I, Firfer B, Ray V, Hubbard-Shepard M, Rhee H. Malignant granular cell tumor. Arch Pathol Lab Med 1992; 116(2)206–8
- Chetty R, Kalan MR. Malignant granular cell tumor of the breast. J Surg Oncol 1992; 49(2)135–7
- Chia J, Poh WT, Tan SK. Malignant granular cell tumour of the lower limb–a case report and review of the literature. Ann Acad Med Singapore 1993; 22(3)384–6
- Gokaslan ST, Terzakis JA, Santagada EA. Malignant granular cell tumor. J Cutan Pathol 1994; 21(3)263–70
- Robertson AJ, McIntosh W, Lamont P, Guthrie W. Malignant granular cell tumour (myoblastoma) of the vulva: report of a case and review of the literature. Histopathology 1981; 5(1)69–79
- Ross RC, Miller TR, Foote FW, Jr. Malignant granular-cell myoblastoma. Cancer 1952; 5(1)112–21
- Jardines L, Cheung L, LiVolsi V, Hendrickson S, Brooks JJ. Malignant granular cell tumors: report of a case and review of the literature. Surgery 1994; 116(1)49–54
- Rosenthal SA, Livolsi VA, Turrisi AT, 3rd. Adjuvant radiotherapy for recurrent granular cell tumor. Cancer 1990; 65(4)897–900
- Carretero, C, Rudner, E. A Case of Multiple Recurrent Granular Cell Tumors with Malignant Behavior. J AM ACAD DERMATOL 2005;52(3, Supplement 1):P42.
- Rochaix P, Durroux R. [Malignant granular cell tumor. Report of a clinico-pathologic case]. Ann Pathol 1996; 16(4)292–5
- Urabe A, Imayama S, Yasumoto S, Nakayama J, Hori Y. Malignant granular cell tumor. J Dermatol 1991; 18(3)161–6
- Cruz-Mojarrieta J, Navarro S, Gomez-Cabrera E, Perez-Pena L, Soriano P, Peydro-Oyala A, et al. Malignant granular cell tumor of soft tissues: a study of two new cases. Int J Surg Pathol 2001; 9(3)255–9
- Bouraoui S, Letaief H, Mestiri H, Chadly-Debbiche A, Ben Zineb S, Haouet S, et al. [Malignant granular cell tumors. Report of a case of anal localization]. Ann Pathol 1999; 19(2)151–2
- Yoshida T, Hirai S, Horii Y, Yamauchi T. Granular cell tumor of the urinary bladder. Int J Urol 2001; 8(1)29–31
- Adeniran A, Al-Ahmadie H, Mahoney MC, Robinson-Smith TM. Granular cell tumor of the breast: a series of 17 cases and review of the literature. Breast J 2004; 10(6)528–31
- Miracco C, Andreassi A, Laurini L, De Santi MM, Taddeucci P, Tosi P. Granular cell tumour with histological signs of malignancy: report of a case and comparison with 10 benign and 4 atypical cases. Br J Dermatol 1999; 141(3)573–5
- Horowitz, IR, Copas, P, Majmudar, B. Granular cell tumors of the vulva. Am J Obstet Gynecol 1995;173(6):1710–3; discussion 1713–4.
- Ramos PC, Kapp DS, Longacre TA, Teng NN. Malignant granular cell tumor of the vulva in a 17-year-old: Case report and literature review. Int J Gynecol Cancer 2000; 10(5)429–434