Abstract
The International Atomic Energy Agency (IAEA) is an intergovernmental organization composed by 138 Member States within the United Nations. It has a mandate to seek to accelerate and enlarge the contribution of atomic energy to peace, health and prosperity throughout the world. Within the IAEA structure, the Division of Human Health contributes to the enhancement of the capabilities in Member States to address needs related to prevention, diagnosis and treatment of health problems through the development and application of nuclear and radiation techniques within a framework of quality assurance. In view of the increasing cancer incidence rates in developing countries the activities in improving management of cancer have become increasingly important. This review will outline the IAEA's role in cancer management focusing on activities related to improving radiotherapy worldwide.
The International Atomic Energy Agency (IAEA) was established in 1957 as an intergovernmental organization within the United Nations. It has currently 138 Member States. The headquarters are located in the Vienna International Centre and additionally there are two technical and research laboratories, one in Seibersdorf, Austria, and another in Monaco.
The IAEA is well known for its role in the verification of international safeguards agreements, and its activities in nuclear safety-security and nuclear energy, but not so well known for its statutory objective to accelerate and enlarge the contribution of atomic energy to peace, health and prosperity. Within this objective, the IAEA provides the application of nuclear technologies in industry, agriculture, environment, and human health. The IAEA activities in the area of human health focus on the common concerns of Member States that can be most effectively addressed by the use of “nuclear technology” Citation[1]. High priority is given to projects supporting Member States in the implementation of nuclear techniques that are mature or are of service type e.g. common clinical activities and laboratory services for quality assurance in radiation medicine. Equally important are projects that deal with establishing policies for hospitals and laboratory activities and implementing emerging or advanced technologies in radiation medicine. The priority is given to projects dedicated to enhancing or improving existing capacities in response to specific requests from Member States, or research and development in areas of importance in a long-term perspective. In cancer management and radiation oncology, the IAEA is increasingly strengthening collaboration with World Health Organisation (WHO), International Agency for Research on Cancer (IARC), other United Nations (UN) bodies and non-governmental organisations and scientific and professional national and international societies.
The Agency's Department of Nuclear Sciences and Applications is charged with increasing and improving the use of radiation for peaceful purposes, including medical applications. The Division of Human Health contains sections of Applied Radiation Biology and Radiotherapy (ARBR), Dosimetry and Medical Radiation Physics (DMRP), Nuclear Medicine (NM) and Nutritional and Environmental Studies (NAHRES). ARBR focuses its activities in improving access to and the standard level of radiotherapy. Quality control and technical aspects of radiotherapy are together with other activities related to radiation dosimetry in the area of DMRP, which devotes a considerable part of its resources to provide laboratory services in collaboration with WHO and Pan American Health Organisation (PAHO) both to standards dosimetry laboratories and to radiotherapy centres in Member States. The NM section deals with the use of radiopharmaceuticals for the diagnosis, treatment and palliative care in certain diseases including cancer, and to radionuclide-based molecular biology techniques that play a role in the fight against communicable diseases like tuberculosis, malaria and HIV/AIDS. NAHRES has moved from primarily collecting data on contaminants to applications of nuclear techniques using stable isotopes in human nutrition and some aspects on nutritional toxicology, as well as detection of Helicobacter pylori infection, a risk factor for stomach cancer.
WHO has identified four pillars in the fight against cancer, namely Prevention, Early detection and diagnosis, Treatment, and Palliative care Citation[2]. This paper will focus on the description of IAEA's major thrust in the field of cancer care, which is addressing the need for radiotherapy in developing Member States.
An outline of the IAEA activities with input of the Division of Human Health in cancer management is presented in . The collaborative and targeted work has in the 10-year period 1994–2003 resulted in over 500 development programmes and implemented projects supporting 90 countries (value close to 100 million US$). The number of projects has increased during recent years, especially in Africa, Latin America, Eastern Europe, and countries of the former Soviet Union.
Table I. IAEA activities in improving cancer management in developing countries
About half of the Division's work is done through Coordinated Research Projects (CRPs), which are networks of 5 to 15 national research institutions coordinated to conduct research within the countries concerned. Through these projects the standard of care is upgraded through applications of evidence based methodology and protocols adapted to the resources and infrastructure in participating countries. Such projects usually generate a number of scientific publications and reports so that new experiences are widely disseminated.
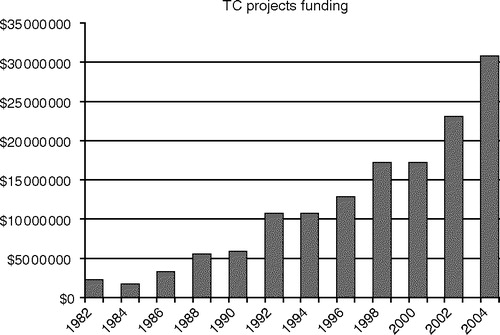
The other half of the work is devoted to provide technical expertise to the IAEA Technical Cooperation (TC) Programme for implementation of projects responding to the increasing needs of Member States. The Agency's budget dedicated to TC projects in the area of Human Health has increased considerably in recent years () being today approximately 25% of the funding of the entire Technical Cooperation Programme. These projects involve for example the transfer of mature nuclear technologies to Member States. Activities include providing recommendations for the purchase of equipment, organization of training courses and workshops (syllabi, teachers and students), selection of technical experts, evaluation of fellowship requests, undertaking technical missions to countries. The IAEA has invested on the average 12 million US$ annually over the last 5 years in radiotherapy TC projects. Currently there are about 100 active TC projects involving radiotherapy, ranging in duration from two to five years. In addition, the Agency activities directed towards improving radiation protection, safety and security infrastructures contribute to establishing the appropriate framework within which radiation therapy can be safely administered.
Need for radiotherapy in the management of cancer
WHO very strongly emphasises cancer prevention relying on three different fronts. These are the widely known anti-tobacco campaigns together with the less known but important healthy diet and prevention of infections, both closely related to cancer incidence Citation[2]. However, there is not much hope that, in a near future, prevention will have a major impact on cancers in developing countries ( with reference Citation[3]). Many will require treatment for cure or relief of pain and other symptoms. A WHO expert consultation group Citation[2] has determined that “together with surgery, radiotherapy currently remains the most cost effective way of curing cancer” and “radiotherapy is an essential component of modern health care”.
Figure 2. Estimate of cancer incidence in developing and developed (industrialized) countries. Note that in 1990 the incidence was practically the same in the two groups. In a time frame of 20 years, there will be approximately 260 million new cancer cases and nearly 150 million will be in developing countries [3].
![Figure 2. Estimate of cancer incidence in developing and developed (industrialized) countries. Note that in 1990 the incidence was practically the same in the two groups. In a time frame of 20 years, there will be approximately 260 million new cancer cases and nearly 150 million will be in developing countries [3].](/cms/asset/8d822fd5-480d-494d-9e59-282abf279335/ionc_a_134118_f0002_b.jpg)
In the developed world 60% of cancer patients have needs for radiotherapy treatment, either with curative or palliative intent Citation[4]. This goal is not quite met even in countries with well-organized public health care and stable infrastructure, such as Sweden Citation[5], where the percentage of cancer patients treated with radiotherapy increased from 32% in 1992 to 47% in 2001. Early and improved diagnostics have increased and will increase the need for curative radiotherapy. Also the use of brachytherapy has significantly increased and includes other than gynaecological indications. A Swedish expert group has estimated that with the overall cancer cure rate slightly above 50%, radiation therapy alone or in combination with other methods is significant for about 40% of patients who are cured Citation[6]. Radiation therapy can also effectively alleviate many tumour related symptoms, but in many countries palliative radiotherapy is not available as much as needed.
Thus, the need to upgrade radiotherapy services is felt worldwide, both due to the growing numbers of cancer patients especially in developing countries and also the overall demand and shortage for professional training of staff working in radiotherapy. For developing countries, the estimate on global cancer incidence development Citation[3] shows an alarming rise in cancer statistics over the next 20 years. The five common cancers with projected increasing incidence in developing countries are cancer of the lung, breast, cervix, head and neck and colorectal cancer. The role of radiotherapy is important in the treatment of these cancers both in curative and palliative indications. It is estimated, that by the year 2015 there will be 15 million new cancer patients in the world each year of which 9 million will be in the developing countries Citation[3].
In developing countries the need for radiotherapy is much larger as tumours are often diagnosed in advanced stage. Therefore it is estimated that even 60 to 70% of cancer patients in these countries would be appropriately treated with radiotherapy, either with curative or palliative intent. However, in developing countries radiation therapy is available only for 20–25% patients needing it Citation[7]. In serving its Member States the IAEA has an emerging role in the field of cancer care and this will be strengthened in all regions during the coming years.
Availability of radiotherapy resources
The number of teletherapy machines per million populations is an essential marker for the ability to deliver appropriate service, and the increase in the number is closely linked to the gross national income (GNP)/per capita of a country Citation[1]. Radiotherapy equipment in developing countries or countries in transition is often old or of such quality that it would no longer be used in developed countries. Some African countries have no facilities for radiotherapy and many developing countries are poorly equipped. For instance, in Ethiopia there is only one cobalt machine for 60 million people and in Nicaragua, one cobalt machine for radiotherapy for 5.4 million people, whereas in the advanced European countries, there is one teletherapy unit for less than 200 000 people Citation[8]. The European standard is not matched in the majority of developing countries. Given the recent cancer rates, and based on a survey by an working group ESTRO has observed that there is on the average one teletherapy machine per 450 patients, one radiation oncologist per 200–250 patients and one physicist per each teletherapy machine or 450 patients Citation[9]. In developed countries the acquisition of equipment increases continuously with the increase in GNP Citation[1].
Directory of radiotherapy centres –DIRAC
In 1995 the IAEA undertook the task of building a computerised international registry of hospitals and clinical institutions that offered radiation therapy with radionuclide or high-energy teletherapy equipment that was given the name of DIRAC (DIrectory of RAdiotherapy Centres). WHO joined the project in an early stage.
DIRAC includes data collected on teletherapy machines, devices and sources used in brachytherapy, and equipment for dosimetry, patient dose calculation and quality assurance. The number of staff employed at installations (radiation oncologists, medical physicists, technicians, etc.) is included as well. In its present version, DIRAC includes approximately 5800 radiotherapy centres in 159 countries with more than 8200 radiotherapy machines and about 2900 brachytherapy units installed (). The database is being continuously updated according to circulated questionnaires and has recently been posted in the internet Citation[8]. However, it is still an incomplete description of the present status of radiotherapy in the world. It is estimated that over 1000 radiotherapy facilities, mainly in USA and Japan, are not yet registered in DIRAC.
Table II. Worldwide resources in radiotherapy: teletherapy and brachytherapy in developing and developed countries (North America, Western Europe, Australasia and Japan, with uncompleted data especially from North America/Japan); data from the IAEA/WHO Directory of Radiotherapy Centres (June 2005).
Even though developing countries represent about 85% of the world population, they only have approximately 40% of the world's radiotherapy facilities. This is far from being sufficient to serve the current population. If one machine is required for 450 new cancer cases treated, as estimated by ESTRO, the current need is at least 5000 machines. To eliminate the deficit in treatment capacity would require at least 1–2 billion US dollars and much more when the need for trained staff and appropriate arrangements for radiation protection, safety and security are added.
In response to the increasing burden of cancer in developing countries and the need for more funding than dedicated by IAEA budgetary sources, a new activity called “Programme of Action for Cancer Therapy” or PACT Citation[7] has been initiated. It aims to raise public awareness, address donators for funds and focus Member State collaborative projects on the growing global needs in cancer management. The program seeks funds from a wide range of donors to increase the IAEA activities in cancer management to better respond to growing needs in developing countries. The PACT programme also seeks to build stronger partnerships with other international organizations and coordinate activities with WHO, PAHO and IARC, as well as including collaboration with the private sector and appropriate nongovernmental organizations.
The short term objectives of the PACT programme are: 1) to raise awareness of the cancer problem and help decision makers to establish appropriate national policies and programmes in cancer care and 2) to upgrade and develop radiotherapy centres towards comprehensive management and training programmes for radiotherapy.
In September 2004, the IAEA general conference gave a resolution supporting PACT in addition to WHO Executive Board giving a resolution on cancer. The effort of both organizations is to build on existing roles and responsibilities with strengthening collaboration to address the cancer problem in the world.
IAEA service in improving cancer management
To establish and upgrade a radiotherapy centre the IAEA provides through its technical cooperation (TC) programmes the expertise to estimate the need for resources and staff, training programmes, expert visits and the most appropriate facilities in specific target areas or countries. IAEA experts assist in project collaboration responding to the needs and requests by Member States. Such projects are carried out through multidisciplinary collaboration of several expertise sections in IAEA. Upgrading radiotherapy facilities is currently ongoing in some 80 countries through national and regional projects, and establishing or improving quality assurance programmes in radiation oncology in another 20 national and five regional projects. Cobalt machines are preferred in centres where power supply, staff training, and infrastructure are not as stable and high level as required in order to use more sophisticated equipments. Several guidelines (IAEA TecDocs, refs Citation[10–13]) for improving safety and QA in radiotherapy have been published. Worth special emphasis is the recently updated IAEA TecDoc 1040 with guidelines for the design and implementation of a radiotherapy programme (clinical, medical physics, radiation protection and safety aspects).
Through IAEA supervised programmes the implementation of modern radiation therapy has commenced in countries such as Ethiopia, Ghana, Mongolia, Namibia, Uganda, and Yemen. For instance, Ghana did not have any radiotherapy services available before IAEA experts provided the technical expertise to design and equip the hospital and organize training opportunities for staff including radiation oncologists, medical physicists and radiation therapy technologists. Economical and collaborative commitment from the country's Health Ministry is the prerequisite for sustainable improvement. Today the centre is serving not only the country's own people but also patients from neighbouring countries as well. More importantly a comprehensive national plan is to be developed with future help of the IAEA experts.
The lack and growing need of skilled and well-trained staff to run radiotherapy centres has been recognized. Lack of qualified staff can result in inappropriate use of treatment facilities. In addition to insufficient training capabilities to match the increasing need of cancer care, developing countries suffer from the ongoing brain drain of healthcare staff to the developed world Citation[14]. IAEA has an active role in developing training programmes and providing opportunities for training and continuous professional development for all professionals needed to run a radiotherapy centre. These include individual training programmes delivered through a generous package of fellowships and scientific visits to highly reputable radiotherapy institutions and a series of training courses organized by the IAEA alone or in co-operation with various organizations. Since 1997 the IAEA has supported the participation of over 1000 radiotherapy professionals in regular ESTRO teaching courses. Training on establishing a cancer registry has been organized together with IARC. Distance learning programs e.g. in radiation biology, have been developed in addition to organizing on site training and distribution of teaching material. Workshops and meetings are organized locally, regionally and inter regionally.
IAEA and Quality Assurance activities
Quality Assurance (QA) in all processes of radiotherapy involving multidisciplinary staff groups is necessary to ensure high and continuous quality of the radiation treatment and to optimize the clinical outcome. A comprehensive, systematic and consistently applied QA programme plays a fundamental role in the prevention of systematic errors, decreasing the frequency and size of random errors, and allowing their early identification and providing guidelines for their management. The majority of accidental exposures in radiotherapy have occurred in hospitals without properly implemented QA programmes. Independent external quality audits, forming part of a comprehensive QA programme, are widely recognized as an effective method to verify that the quality of radiotherapy practice is appropriate. Quality audits include a wide range of types and levels of review, either of the entire radiotherapy process or of specific critical parts of it, such as radiotherapy dosimetry.
In clinical radiotherapy beam output variation has been shown to relate to the complication rate Citation[15]. Generally it has been observed that accurate dosimetry is essential for the ability of a clinic to deliver accurate doses to cancer patients Citation[16]. The verification of the dosimetry of radiotherapy beams is a well-established and well-recognized programme of the IAEA to improve management of cancer. The IAEA in collaboration with the WHO was the first organization to initiate dosimetry audits on an international scale in 1969, using mailed thermoluminescent dosimeters (TLD). WHO (or PAHO in Latin America and the Caribbean) takes care of mailing dosimeters to radiotherapy hospitals in different countries and these are returned after irradiation to the IAEA's Dosimetry Laboratory where the dose measured by the TLD is compared with the dose stated by the hospital staff Citation[11], Citation[17]. When necessary, a follow-up programme for quality improvement for hospitals with poor results is organized. This may include site visits and support and training to the staff with described procedure guidelines to resolve possible discrepancies in dosimetry Citation[18]. In 36 years, the IAEA/WHO TLD audit service has already checked the calibration of more than 5600 radiotherapy beams in about 1400 hospitals in 116 countries worldwide. This work has a significant impact on the quality of radiotherapy.
Though vital for the radiotherapy process, accurate beam dosimetry and treatment planning do not guarantee a successful treatment of the patient; QA of the entire radiotherapy process must be taken into account. Especially with increasing trends of multidisciplinary treatment in radiation oncology, a comprehensive approach in Quality Assurance has become necessary to ensure the effective use of technology and ensure the safety of the patient and the personnel.
The need for QA in developing countries is the same as in developed countries although the conditions and requirements are different. Quality measurements and an understanding of their significance are necessary for the development of basic knowledge on how to create a quality system. Starting a quality program in a centre requires time and costs appropriated for other daily activities, but it will always pay back by more time for the actual work and improving the practice. It leads to fewer complications, better quality of service and safety for the benefit of both patients and personnel. In a comprehensive QA system, all aspects of QA in radiation oncology are addressed, ranging from departmental policy, organization, infrastructure, staffing level and skills, equipment, and the tasks related to quality control, through all processes and procedures, to safety of the patient and personnel and the issues of environment and costs.
Following the recommendations of the IAEA Basic Safety Standards Citation[19] and the Council Directive 97/43 Euratom Citation[20], several Member States are in the process of adopting regulations on QA in radiotherapy, thereby making audits mandatory for radiotherapy departments Citation[20–22]. To address QA of the entire radiotherapy process, a new approach in the audit has been developed by the IAEA and named “Quality Assurance Team for Radiation Oncology (QUATRO)”. In response to the numerous requests of Member States a methodology for the comprehensive audit of radiotherapy centres has been prepared by IAEA through consultancy with a group of international experts Citation[23]. The audit methodology has been successfully pilot tested in a series of field missions. The document outlines procedures for the preparation, implementation and conclusion of a comprehensive clinical audit by a multiprofessional audit team. The audit structure is devised to follow the patient from the diagnosis of cancer through the treatment process taking into account the departmental policy, staff performance and qualifications, process structure, management and safety, and available equipment and fluency of multiprofessional tasks. An international workshop was organised in May 2005 to train the trainers in clinical audit from various geographical regions and regional courses will follow shortly.
Research related activities
Radiation therapy plays an increasingly important role in curative and palliative therapy of cancer and presents a considerable challenge to research Citation[24]. Through IAEA, multinational Co-ordinated Research Projects (CRPs) are established on particular topics in response to the needs of Member States. These can be clinically or laboratory based, or a combination of the two. IAEA CRPs are activities of the kind of “adaptive” research projects, operational research, or implementation of new techniques, leading to developments at the national level. They usually last for 3–5 years and involve institutions from developed countries (unfunded research agreements) and developing countries (funded research contracts). Currently translational research and academic collaboration is encouraged and this is combined to a new concept of involving doctoral CRPs. Through these the number and level of target related PhD degrees will be increased in developing countries by matching with a “host institution” in an industrialized country.
In clinical research the focus is on development of evidence-based resource sparing guidelines for target areas, which are acknowledged as important in Member States. The initiative can come from a Member State or it can be a research protocol prepared by the Agency's experts in collaboration with specialist centres in Member States. shows examples of clinical research projects in radiotherapy with reference to their publications Citation[25–29]. These studies have clarified multidisciplinary treatment practices and helped to develop resource sparing clinical protocols in radiotherapy.
Table III. IAEA research activities in cancer field a) recent studies, b) current studies. Publication reference indicated [25–29].
In the area of medical physics CRPs focus on developments related to national QA programmes for radiotherapy dosimetry, acceptance testing and quality control of treatment planning systems and development of methodology for in vivo dosimetry. In many cases the results of the CRPs are distributed to Member States using technical cooperation mechanisms. An example is the Czech national programme in radiotherapy QA based on the methodology developed under a CRP. Starting with simple dosimetry checks the national audit activity has expanded to a larger programme involving thorough QA tests of teletherapy machines. At present the QA programme further develops towards introducing a comprehensive quality audit in radiotherapy using the QUATRO methodology.
Conclusion
This paper provides an overview of the tasks that IAEA has in the field of cancer care. The overall objective in IAEA activities in cancer management is to provide expertise for the development of sustainable national capability to provide evidence based cancer therapy to patients in developing countries and to help the countries build and improve their service. This requires expert collaboration to create national cancer control strategies, training of staff to provide appropriate treatment and having adequate treatment facilities, effective management, and safety and quality control programs. The IAEA serves Member States as a global centre of expertise in all relevant aspects of radiotherapy technology, such as planning a centre, training staff, economic analysis, implementation, radiation protection, safety and security and developing evidence based guidelines. The role of IAEA activities in cancer control programmes has grown and it is becoming increasingly important in developing countries due to growing cancer rates and the need for expertise to build competent centres with staff training capacities, enhancing the transfer from quantity driven to evidence based quality radiotherapy.
We wish to thank Krys Kiel, M.D., for collecting data from research publications.
References
- Levin V, Tatsuzaki H. Radiotherapy services in countries in transition: Gross national income per capita as a significant factor. Radiother Oncol 2002; 63: 147–50
- World Health Organization. www.who.int/mediacentre/news/releases/2003/pr27/en.
- Globocan. www.dep-depdb.iarc.fr.
- Principles and practice in radiation oncology. In: Perez CA, Brady L, Halperin EC, Smidt-Ullrich RK, editors. 4th ed. Lippincott: Williams and Wilkins; 2004.
- Mattsson S, Brahme A, Carlsson J, Denekamp J, Forssell-Aronsson E, Hellstrom M, et al. Swedish Cancer Society radiation therapy research investigation. Acta Oncol 2002; 41: 596–603
- Ringborg U, Bergqvist D, Brorsson B, Cavallin-Ståhl E, Cedeberg J, Einhorn N, et al. The Swedish Council on technology assessment in health care (SBU) systematic overview of radiotherapy for cancer including a prospective survey of radiotherapy practice in Sweden 2001- Summary and conclusions. Acta Oncol 2003; 42: 357–65
- Kovan D. PACT: The IAEA's plan to stem the ‘cancer crisis’ in developing countries. Nuclear news 2004;Dec:47–51.
- DIRAC. http://www-naweb.iaea.org/nahu/dirac/directory.asp.
- Slotman BJ, Cottier B, Bentzen SM, Heeren G, Lievens Y, van den Bogaert W. Overview of national guidelines for infrastructure and staffing of radiotherapy. ESTRO-QUARTS: Work package 1. Radiother Oncol 2004;Dec 23: e-pub.
- Design and implementation of a radiotherapy programme: clinical, medical physics, radiation protection and safety aspects. IAEA-TECDOC-1040. Vienna: IAEA; 1998 (revised 2005).
- Izewska J, Svensson H, Ibbott G. Worldwide Quality Assurance networks for radiotherapy dosimetry. Proceedings of the international symposium on standards and codes of practice in medical radiation dosimetry, 25–28 November 2002. IAEA-CN-96/76. Vienna: IAEA; 2004. p 139–55.
- International basic safety standards for protection against ionizing radiation and for the safety of radiation sources. Safety Series No. 115. Vienna: IAEA; 1996.
- International Atomic Energy Agency (IAEA). Radiological protection for medical exposure to ionizing radiation, Safety Guide. IAEA Safety Standards Series No. RS-G-1.5 Vienna: IAEA; 2002.
- Coombes R. Developed world is robbing African countries of health staff. BMJ 2005; 330: 923
- Bentzen SM, Bernier J, Davis JB, Horiot JC, Garavaglia G., Chavaudra J, et al. Clinical impact of dosimetry quality assurance programmes assessed by radiobiological modelling of data from the thermoluminescent dosimetry study of the European Organisation for Research and Treatment of Cancer. Eur J Cancer 2000; 36: 615–20
- Thwaites DI, Scalliet P, Leer JW, Overgaard J. Quality assurance in radiotherapy. Radiother Oncol 1995; 35: 61–73
- Izewska J, Andreo P. The IAEA/WHO TLD postal programme for radiotherapy hospitals. Radiother Oncol 2000; 54: 65–72
- Izewska J. Standardized quality audit procedures for on-site dosimetry visits to radiotherapy hospitals. SSDL Newsletter. Vienna 2002; 46: 17–23
- International basic safety standards for protection against ionizing radiation and for the safety of radiation sources. Jointly sponsored by FAO, IAEA, ILO, PAHO, WHO. IAEA Safety Series No. 115. Vienna: IAEA; 1996.
- European Union Council directive 97/43/Euratom, 1997.
- Schweiger B (ed). Quality policy in the health care systems of the EU accession countries. Vienna: Federal Ministry of Social Security and Generations; 2001. www.gesundheit.bmsg.gv.at.
- Shaw C. Clinical audit in the general context of quality management. Proceedings of the symposium for clinical auditing. TampereFinland, 2003.
- Development of procedures for on-site visits to radiotherapy hospitals by IAEA experts concerned with reviewing the treatment planning process Internal report IAEA-DMRP-2003-01. Vienna: IAEA; 2003.
- Zackrisson B, Mattsson S, Kjellen E, Glimelius B. Swedish Cancer Society Investigation Group. Research and development of radiation therapy in clinical routines. Acta Oncol 2003; 42: 115–22
- Sur R, Levin V, Donde B, Sharma V, Miszyck L, Nag S. Prospective randomized trial of HDR brachytherapy as a sole modality in palliation of advanced oesophageal carcinoma-an IAEA study. Int J Rad Oncol Biol Phys 2002; 53: 127–33
- Grau C, Prakash Agarwal J, Jabeen K, Rab Khan A, Abeyakoon S, Hadijieva T, et al. Radiotherapy with or without Mitomycin C in the treatment of locally advanced head and neck cancer: Results of the IAEA multicenter randomized trial. Radiother Oncol 2003; 67: 17–26
- Vasanthan A, Mitsumori M, Park JH, Zhi-Fan Z, Yu-Bin Z, Oliynychenko P, et al. Regional hyperthermia combined with radiotherapy for uterine cervical cancers: a multi-institutional prospective randomized trial of the international atomic energy agency. Int J Radiat Oncol Biol Phys 2005; 61: 145–53
- Sur R, Donde B, Falkson C, Ahmed SN, Levin V, Nag S, et al. Randomized prospective study comparing HDR intraluminal brachytherapy (HDLILBT) alone with HDRILBT and external beam radiotherapy in the palliation of oesophageal cancer. Brachytherapy 2004; 3: 191–5
- Salazar O, Sandhu T, da Motta N, Escutia MA, Lanzos-Conzales E, Mouelle-Sone A, et al. Fractionated half body irradiation (HBI) for the rapid palliation of widespread symptomatic metastatic bone disease: A randomized phase III trial of the IAEA. Int J Rad Oncol Biol Phys 2001; 50: 765–75