To the Editor
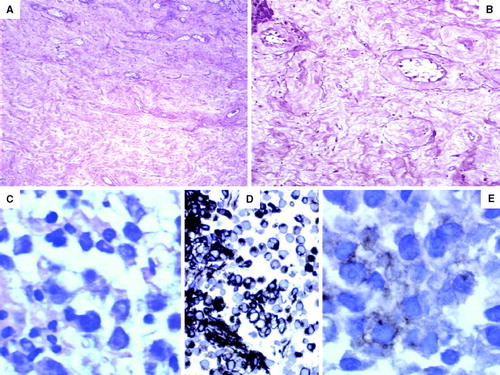
A 42-year-old male patient presented to his local doctor with profuse night sweating and back pain. Multiple retroperitoneal lymph node metastases (from 2.1 to 3.5 cm masses) were found to the right of the aorta on the computed tomography (CT) scan. The masses displace the aorta, renal right arteria and cava vein with CT evidence of infiltration. A testicular ultrasound confirmed a 3.0 cm hypoechoic nodule within the left testicle; the right testicle was normal in size. Tumour marker β-human chorionic gonadotropin (β-HCG) was out of range (11 mUI/m) and α-fetoprotein (α-FP) was normal. Lactic dehydrogenase (LDH) was found out of normal range (LDH = 5515 UI/l). The patient was found to have low testosterone level (2.56 ng/ml; normal range 2.0–11.0 ng/ml) and high follicle-stimulating hormone (FSH = 20.6 mU/ml; normal range: 1.5–12.4 mU/l) and luteinizing hormone (LH = 8.3 mU/ml; normal range 1.7–8.0 mU/ml). The patient underwent an inguinal left orchiectomy. Histology showed absence of germ cells, Leydig cell hyperplasia with mixomatoid intratubular transformation and severe tubular atrophy (A, B). The patient subsequently underwent a CT guided retroperitoneal lymph node biopsy, which was histologically confirmed with widespread replacement by seminoma (immunohistochemistry positive for PLAP; negative for LCA, CD3, CD20, CD30, CD138 e S – 100) (C, D, E). Treatment was completed with four cycles of cisplatin, bleomycin and etoposide due to presence of bulky retroperitoneal disease.
Figure 1. (A) The testis showed severe tubular atrophy, Leydig cell hyperplasia and absence of germ cells (hematoxylin and eosin×200 magnification). (B) Eosinophilic and mixoid transformation with rare hyalinized tubules (elastic tissue stain×200 magnification). (C) Lymph node core biopsy showed uniform cells with clear cytoplasm and clumped chromatin pattern of nucleus. (D) The neoplastic cells showed strong expression of vimentin. (E) Weak expression of placental alckaline phosphatase.
“Burned out” phenomenon in germ cell tumours is not a rare event Citation[1–5]. For retroperitoneal germ cell tumours it is a routine to look for small primary tumours in the testicles and we usually find various histological lesions of the testis including hyalinosis, hemosiderin deposition and fibrosis, indicative of the earlier and completely regressed malignancy. Such scars usually are, however, generally less than 1 cm. Our patient presented with hypogonadism, and endocrinological abnormalities have been reported in other cases Citation[3], Citation[6]. We cannot exclude the possibility that tumour regression may be due to an underlying endocrinopathy with an immunostimulating effect. It is conceivable that the immune-privileged site of the testes disfavors the recruitment of innate immune cells that have been associated with tumour growth and with the induction of tolerance. When the tumour becomes metastatic, it probably reaches the draining lymph node before the establishment of full immune-escape mechanisms. Once in the lymph node, tumour cells could become visible to professional antigen presenting cells for induction of adaptive immunity, which can participate to the regression of the primary tumour. In the presence of retroperitoneal lymph nodal bulky, a testicular ultrasound can detect tiny intratesticular lesions, minimizing the possibility of a primary extragonadal germ cell tumour. It is important to distinguish “burned out” tumours of the testis from true extragonadal germ cell tumours because the primary removal of the testicular tumour is necessary for the overall outcome Citation[5]. These malignancies are treated surgically with or without chemotherapy or radiotherapy. The therapeutic outcome for patients with extragonadal germ cell tumours is similar to that of patients with very advanced testicular cancer when considered in relation to the presence of prognostic factors and, among them, seminomas have a better prognosis Citation[7].
References
- Perimenis P, Athanasopoulos A, Geraghty J, Macdonagh R. Retroperitoneal seminoma with “burned out” phenomenon I the testis. Int J Urol 2005; 12: 115–6
- Ojea Calvo A, Rodriguez Alonso A, Perez Garcia D, Dominguez Freire F, Alonso Rodrigo A, Rodriguez Iglesias B, et al. Extragonadal germ cell tumor with “burned out” phenomenon in the testis. Actas Urol Esp 1999; 23: 880–4
- Goss PE, Schwertfeger L, Blackstein ME, Iscoe NA, Ginsberg RJ, Simpson WJ, et al. Extragonadal germ cell tumors. A 14-year Toronto experience. Cancer 1994; 73: 1971–9
- Weber O, Hubert J, Grignon Y, Mangin P. Spontaneously involuting metastatic seminoma of the testis (“burned out” seminoma). Report of a case presenting with supraclavicular adenopathy. Prog Urol 1996; 6: 278–81
- Borrego Hernando J, Guinda Sevillano C, Laguna Pes MP, Zazo A, Gimeno A, Cuesta R, et al. Retroperitoneal germinal tumor: extragonadal or burned out phenomenon of testicular primari? Presentation of a clinical case. Actas Urol Esp 1998; 22: 170–4
- Casella R, Rochlitz C, Sauter G, Gasser T. Burned out testicular tumor: A rare from of germ cell neoplasias. Scheiz Med Wochenschr 1999; 129: 235–40
- Daugaard G, Rorth M, von der Maase H, Skakkebaek NE. Management of extragonadal germ cell tumors and the significance of bilateral testicular biopsies. Ann Oncol 1992; 3: 283–9
