Abstract
In Denmark, a general impression of prolonged pretreatment delay for patients with head and neck cancer led to a nationwide study of time spans from symptom debut over first health care contact to start of treatment. Charts of consecutive new patients with squamous cell carcinoma of the pharynx and larynx, seen at the five Danish oncology centers in January–April 1992 and 2002, respectively, were reviewed. Of the 288 patients identified, definitive treatment was radiotherapy in 264 cases, surgery in one case. Twenty-three patients had neither surgery nor radiotherapy. Total time from first health care contact to start of definitive treatment was significantly longer in 2002 than in 1992 (median 70 versus 50 days, p < 0.001). There was no significantly difference in time used for diagnosis. Time for treatment preparation and planning was 46 days in 2002 versus 31 days in 1992 (p < 0.001). Significantly more diagnostic procedures (CT, MR, US, PET) were done in 2002. In conclusion, this nationwide study showed that waiting time before start of radiotherapy was significantly longer in 2002 compared to 1992. An increasing number of imaging procedures including CT-based dose planning was observed. The prolongation was mainly related to shortage of radiotherapy capacity. The three weeks extra pretreatment delay could theoretically lead to a 10% lower tumor control probability in 2002 compared to 1992.
The clinical workup for patients with head and neck cancer is often complex. Since the options for primary treatment include surgery, radiation therapy, chemotherapy or a combination of these, multidisciplinary care over long periods of time is often required. The expression ‘continuum of care’ has been introduced to describe this ‘coordinated activities in health care linked together to achieve the best possible result for the patient’ Citation[1].
A prolonged delay prior to treatment start may cause decrease in the local control rate as well as survival due to tumor growth Citation[2–5]. Radiobiological studies indicate that a 4-week delay of start of radiotherapy may result in a decrease in local tumor control especially in stage 4 patients and in patients with tumors in the oral cavity Citation[6], a suggestion which was also dealt with in a report from Mackillop et al. Citation[3]. These reports, together with a general impression of prolonged work-up time, led to a nationwide study of time spans from first health care contact to treatment of patients with squamous cell carcinoma of the larynx or pharynx in Denmark. The aim of the study was to analyze changes in time consummation from 1992 to 2002 in a large non-selected population and to obtain ideas for reducing unnecessary waiting time.
Materials and methods
Patients
The population base was Denmark with its 5.4 million inhabitants. Patients were identified from The Danish Head and Neck Cancer Study Group (DAHANCA) database. Since 1992 all patients with hypo pharynx and larynx squamous cell carcinoma have been registered in the DAHANCA database. The study group was unselected patients with primary squamous cell carcinoma of the pharynx and larynx seen for initial work-up in two 4 months periods, January–April 1992 and January–April 2002. We included all patients treated in Denmark in each period. Patients were treated on the 5 head and neck oncology centers: Rigshospitalet, Herlev/Gentofte, Odense, Aarhus, and Aalborg.
The following data were collected: age, sex, location of cancer, stage, treatment center, treatment and dates of first symptom and appointments. Tumor and patient characteristics are shown in . Tumor stage is preterapeutic including information from US, CT, MR and PET scans when these were performed. Two hundred sixty four patients were treated with radiotherapy and only one was treated with surgery as definitive treatment, 23 had neither. This does not allow any conclusions about waiting time for surgery.
Table I. Patient and tumor characteristics
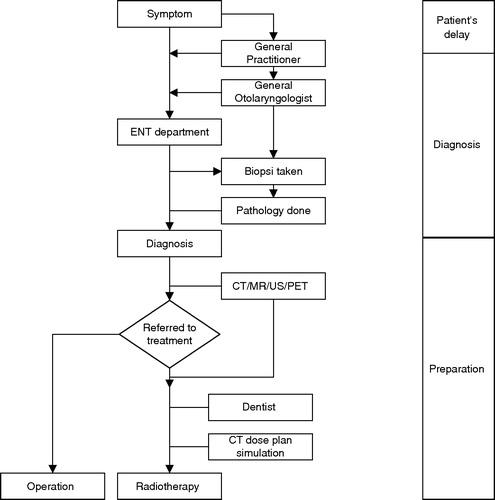
The duration of the pretreatment delay was defined as the time from first contact with the health care system to the start of definitive treatment of the cancer, either the start of radiotherapy or the date of definitive surgery. The pretreatment delay consisted of different steps and time intervals for the individual patient. shows the typical flow pattern for the single patient from first symptom to start of treatment. First contact to the health care system was a general practitioner, general otolaryngologist, dentist or department of head and neck surgery. After biopsy, different imaging as well as dental procedures was performed if indicated and treatment was planned. For this study the pretreatment delay was divided into different calculated time intervals. The three main time intervals were defined: (A) Patient delay; (B) Diagnostics; (C) Treatment Planning.
Figure 1. A graphical presentation of a typical patient flow through the health care system in Denmark. First contact is to a general practitioner (GP), otolaryngologist (ENT) or dentist for referral to a head and neck cancer center (ENT center). The ENT center makes the definitive diagnosis and refers the patient for definitive treatment, which will be decided at a multidisciplinary conference.
Statistics
SPSS 11.5 statistical software for PC was used. All analyzes were non-parametric. Mann-Whitney test was used for comparing time spans between groups. Chi-square was used for testing significant differences in distribution of factors in n-by-n tables. Kruskall-Wallis test was used to compare time spans between institutions. All statistical tests were two-sided and significance was defined as p values less than 0.05.
Results
Patient characteristics were comparable in the two time periods. There was no significant difference in distribution of gender and age above versus below 60 years in the patients. (). There was a trend towards proportionally more pharyngeal tumors in 2002 compared to 1992 (55% versus 36%) and consequential less laryngeal cancers (45% versus 64%). These differences were, however, not statistically significant. More tumors were stage 4 (40% versus 27%) and less were stage 1 (17% versus 28%) in 2002 (p = 0.01, Mann-Whitney). This is explained by the change in distribution of site. If we compare stage distribution for each site there is no significant difference ().
The main results are shown in . There was a trend for longer patient delay in 2002 than in 1992, 75 days versus 63 days, (non significant). Total time from first health care system contact to start of definitive treatment was significantly longer in 2002 than in 1992 (70 versus 50 days, p < 0.001). Time used for diagnosis (B) was unchanged (18 versus 19 days). Prepare time for treatment (C) was 46 days in 2002 versus 31 days in 1992 (p < 0.001).
Table II. Main time intervals in the pretreatment delay 1992 and 2002. All numbers are in days.
The time from the patient had the initial diagnosis to referral for radiotherapy includes assessment at multidisciplinary conferences as well as unnecessary delay. This interval was median 5.5 days (10;90% percentiles 0–30 days) in 1992 and 7 days (10;90% percentiles 0–23 days) in 2002. This difference was not significant. Time from patient was referred for radiotherapy to start of treatment was median 21 days (10;90% percentiles 13–33 days) in 1992 and 40 days (10;90% percentiles 25–50 days) in 2002 (p < 0.001), respectively.
Patients had more imaging procedures in 2002 than in 1992 (). This was significant for all procedures including US, CT, MR and PET. PET was not available in 1992. In 2002 the centres at Rigshopitalet and Aarhus had PET scanners, which were also open for referral from the other centres. For treatment planning there was a change towards more advanced techniques including CT based dose planning ().
Table III. The extent of diagnostic tests used in the two periods. Information was available in 121–124 patients in 1992, 156–157 patients in 2002.
To get an idea of the impact of more imaging procedures on time spans we separately looked at patients in clinical Stage 1. The work up for these patients was similar in the two time periods; patients in clinical Stage I had very few imaging procedures in both time periods: In 1992, none of 47 patients had CT, MR or US scans; in 2002 five of 36 patients had CT (1), MR (1), or US (3), respectively. A substantial part had CT based dose plans in 2002, twelve of 36 (33%) versus none of 28 (0%) in 1992. Although not significant, the results of the subgroup analysis for stage I show a trend for longer time in health care system in 2002 than in 1992 (median 70 versus 48 days, p = 0.18).
Discussion
The current data confirmed the impression that the time span from first symptom to start of treatment for patients with head and neck cancer is very long, and also increased over the last ten years. It seems that both the patient delay and the radiotherapy planning time are involved, whereas the time required from first visit until diagnosis remains fairly short and unaltered over the ten years.
The patient's delay was not significantly longer in 2002 compared to 1992. The few other studies have shown that the reliability of this parameter is questionable. It may be highly variable Citation[7] as well as imprecise and difficult to explain Citation[8]. The lack of reliable data does not mean that patient's delay is not of importance. The present study, however, demonstrated that the prolonged delay of treatment is due to increased time consummation in the health care system.
The current study was inspired by a Swedish report from the Stockholm area Citation[1]. The authors compared two time periods, before and after a major reorganization of the local ENT service in 1998. The results showed an increase in median time from first contact with health care provider to start of treatment from 67 days to 89 days. In contrast to our findings, their preparation time and waiting time for radiotherapy remained unchanged at around one month, whereas the time used for initial diagnosis increased with two weeks. All in all, the Swedish and Danish waiting times seem to be comparably long Citation[1].
Waiting time for treatment is frustrating both for the patient and the involved health care staff. Apart from the psychological stress, it has been shown that tumors grow during waiting time, which will potentially lead to impaired chance of cure. Waaijer et al. Citation[2] found a mean increase in tumor volume of 70% during a mean waiting time of 56 days for oropharyngeal cancer. The estimated loss of tumor control probability from such a volume increase was 16–19%. A recent Danish study suggested that in glottic larynx cancer one month delay led to a 4% decrease in survival Citation[9]. Other studies support that delay may lead to tumor growth and stage migration in head and neck cancer patients Citation[3–5]. These waiting times are comparable to the observation from the present study, so also in our material there is a risk of impaired tumor control and survival during the prolonged work-up for Danish patients in 2002 compared to 1992.
The negative consequences of delay for the outcome of treatment of head and neck cancer has been described by Mackillop et al. Citation[3]. If tumor volume doubling time in squamous cell carcinomas is set to 58 days, as suggested by Tubiana Citation[10], the effect of the additional 20 days delay in 2002 compared to 1992 will correspond to a loss of tumor control probability of approximately 10%. A change in local tumor control of this magnitude equals the gain from shorter treatment time, which was achieved by introducing accelerated fractionation in the DAHANCA 6 and 7 trials Citation[11].
New diagnostic tests and technology has been suggested to play a role in prolonging the pre-treatment delay. In our series, more imaging procedures (CT, MR, PET, US) were performed in 2002, and also CT based treatment planning was routinely used in the latter period. These modalities were more easily available in 2002 than in 1992, where we had few MR scanners and no PET scanners in Denmark. Although there is an apparent association between the use of imaging procedures and pre-treatment delay, it is important to emphasize that the current data do not prove such causality. For most centres, the main bottleneck in 2002 was the time slots on the treatment machines. Because surgery, radiotherapy fractionation, field techniques, total treatment time and the use of chemotherapy have changed in the same period, the impact of new technology on outcome in the current series is impossible to evaluate.
It has been suggested that the shortage of radiotherapy units should encourage us to use more surgery as primary treatment for head and neck cancer, i.e. more laser surgery for selected glottic tumors. We believe, however, that the choice of treatment in national treatment recommendations should be based on documented treatment outcome, and for laser surgery, it has never been convincingly documented that it leads to the same functional results as radiotherapy. The radiotherapy centres have instead temporarily increased the throughput by using extended working hours on the machines, and by referring patients to treatment abroad.
The shortage of radiotherapy treatment units in Denmark has been documented in a expert report from the Danish Society for Oncology 1999, and later acknowledged by the Cancer Control Plan by the National Board of Health in 2000 Citation[12]. In the late 1990's the accelerator capacity became a limiting factor due to new indications for radiotherapy in a number of other cancer types. In 2002 a total of 34 linear accelerators served the Danish population of 5.4 million inhabitants. Only 20 of these units were equipped with multileaf collimators. The expert group estimated that the lack of capacity in 2002 equaled an additional 16 units Citation[12]. This definitely influenced the waiting time in 2002 in all five centers. The National Cancer Plan from 2000 caused a significant increase in the investments in capacity for cancer treatment, including radiotherapy Citation[12]. As a result all centers are currently expanding their capacity. The apparent differences between centers in 2002 may be explained by differences between the expansion rates of the centers in that specific year. A planned new survey in 2007 will hopefully show that the investments in facilities have lead to the desired drop in waiting time at all centers.
Conclusions
From the present study it is clear that the pretreatment delay for new head and neck cancer patients was three weeks longer in 2002 compared to 1992. An increasing number of imaging procedures including CT-based dose planning was observed. The prolongation was mainly related to shortage of radiotherapy capacity. The three weeks extra pretreatment delay could theoretically lead to a 10% lower tumor control probability in 2002 compared to 1992. The long waiting time in health care system is hopefully solved by the investments in The National Cancer Plan for more staff, scanners and linear accelerators.
We thank the Danish Cancer Society and the Hede Nielsen Foundation for financial support.
References
- Sharp L, Lewin F, Hellborg H, Lundgren J, Hemmingsson E, Rutqvist LE. When does my treatment start?–The continuum of care for patients with head and neck cancer. Radiother Oncol 2002; 63: 293–7
- Waaijer A, Terhaard CH, Dehnad H, Hordijk GJ, van Leeuwen MS, Raaymakers CP, et al. Waiting times for radiotherapy: consequences of volume increase for the TCP in oropharyngeal carcinoma. Radiother Oncol 2003; 66: 271–6
- Mackillop WJ, Bates JH, O'Sullivan B, Withers HR. The effect of delay in treatment on local control by radiotherapy. Int J Radiat Oncol Biol Phys 1996; 34: 243–50
- Coles CE, Burgess L, Tan LT. An audit of delays before and during radical radiotherapy for cervical cancer–effect on tumour cure probability. Clin Oncol (R Coll Radiol) 2003; 15: 47–54
- Wyatt RM, Beddoe AH, Dale RG. The effects of delays in radiotherapy treatment on tumour control. Phys Med Biol 2003; 48: 139–55
- Kowalski LP, Carvalho AL. Influence of time delay and clinical upstaging in the prognosis of head and neck cancer. Oral Oncol 2001; 37: 94–8
- Amir Z, Kwan SY, Landes D, Feber T, Williams SA. Diagnostic delays in head and neck cancers. Eur J Cancer Care (Engl) 1999; 8: 198–203
- Wildt J, Bundgaard T, Bentzen SM. Delay in the diagnosis of oral squamous cell carcinoma. Clin Otolaryngol 1995; 20: 21–5
- Hansen, O, Larsen, S., Bastholt, L, Godballe, C, Jorgensen, KE. Duration of Symptoms Impact on outcome in glottic cancer patients. Int J Radiat Oncol Biol Phys 2005; In Press.
- Tubiana M. Tumor cell proliferation kinetics and tumor growth rate. Acta Oncologica 1989; 28: 113–21
- Overgaard J, Hansen HS, Specht L, Overgaard M, Grau C, Andersen E, et al. Five compared with six fractions per week of conventional radiotherapy of squamous-cell carcinoma of head and neck: DAHANCA 6 and 7 randomised controlled trial. Lancet 2003; 362: 933–40
- National Board of Health [Sundhedsstyrelsen]. The National Cancer Control Plan 2000. http://www.sst.dk/faglige_omr/planlaeg/kraeft/national_kraeftplan.htm.
- National Board of Health [Sundhedsstyrelsen]. The National Cancer Control Plan II 2005. http://www.sst.dk/publ/publ2005/plan/kraeftplan2/kraeftplan2.pdf.
