Abstract
The aim of the present study was to analyze whether leukocyte subsets in peripheral blood and tumour biopsies obtained before treatment were able to predict response or survival in patients with metastatic melanoma following Interleukin-2 (IL-2) based immunotherapy. Flow cytometry was performed on peripheral blood for CD4+ T cells, CD8+ T cells and CD56+ natural killer (NK) cells. Immunohistochemical analyses were used to identify CD4+ T cells, CD8+ T cells, CD57+ NK cells and CD64+ (macrophages) cells in tumour biopsies. High numbers of tumour-associated CD64+ macrophages in tumour biopsies were statistically significantly associated with poor response to treatment. Our data suggest that tumour-associated macrophages may correlate negatively with response, which may be of biological importance for IL-2 based immunotherapy of malignant melanoma.
Interleukin-2 (IL-2) has been used in the treatment of metastatic melanoma either alone or combined with interferon-α (IFN) or selected chemotherapeutics, and long-term survival has been shown in a minor fraction of patients Citation[1]. Thus, it is of obvious importance to select those patients who most likely may benefit from treatment or those patients, who are unlikely to benefit. As IL-2 has no direct effect on cancer cells, it is believed that tumour regression is mediated by a modulation of immune effector cells and secondary cytokines released by these immune cells Citation[2]. Various immunomodulatory effects of IL-2 in patients with metastatic melanoma have been demonstrated Citation[3–5], among which are increased numbers of lymphocyte subsets in peripheral blood, including T cells, NK cells and monocytes. However, the present knowledge about immunological parameters that can predict objective response and survival is scarce.
The aim of the present study was to study leukocyte subsets in peripheral blood and tumour biopsies before IL-2 based immunotherapy in patients with metastatic melanoma and to correlate these findings to response and survival.
Materials and methods
Patients and samples
The patients included in the current study were treated in the period from February 1997 to March 2001 at the Department of Oncology, Aarhus University Hospital. The patients participated in two multi-center phase 2 protocols for metastatic melanoma. The inclusion criteria were identical in the two protocols and included biopsy verified stage IV disease, a WHO performance status of 2 or better and absence of brain metastases. Only patients treated in Aarhus and patients with superficial metastases were eligible for inclusion in this tumour biopsy and blood sample study. Tumour biopsies from superficial metastases and blood samples were obtained within a few days prior to treatment. The ethics committee accepted the present project, and written informed consent was obtained from each patient (project # 1997/3900). The treatment schedules have been described in detail elsewhere Citation[6], Citation[7]. Briefly 15 patients were treated with subcutaneous IL-2, IFN and cisplatinum Citation[6], and 12 patients were treated with subcutaneous IL-2, IFN±histamine Citation[7]. Clinical response in both protocols was evaluated according to WHO criteria.
Flow cytometry
Leukocyte phenotypes were determined by flow cytometry on peripheral blood mononuclear cells (PBMCs) from 13 patients treated with IL-2, IFN and cisplatinum and on whole blood samples from 10 patients treated with IL-2, IFN±histamine. PBMCs from heparinized whole blood were prepared by density gradient centrifugation on Ficoll/Hypaque. Interphases were harvested, washed twice at low speed to remove platelets and cryopreserved in 20% DMSO and stored at −135°C until use. Cell surface phenotypes were determined by flow cytometry using either a Coulter XL-2 flow cytometer (Coulter Electronics, Miami FL) or a FACS-Calibur flow cytometer (Becton Dickinson). Data were analysed using the Flow-Jo software for Macintosch from Treestar (San Carlos, CA, USA). Direct fluorochrome-conjugated antibodies were purchased from Becton Dickinson, San Jose, Ca, USA, Leucogate CD45/CD14 FITC/PE catalogue number (cat) 340040, CD4 FITC, cat 340133, CD8 FITC, cat 347313 and CD56 PE cat 347747. A total of 2 x 105 PBMC were incubated with antibody for 15 min at room temperature in the dark, washed twice with PBS containing 0.1% sodium azide and fixed in 1% formaldehyde and prepared for FCM analysis. Whole peripheral blood samples (100 µl) were incubated with antibody for 15 min at room temperature in the dark. Erythrocytes were lysed after staining by addition of FACS lysing Solution (Becton Dickinson) for 10 min at room temperature in the dark. Cells were washed twice with PBS containing 0.1% sodium azide and fixed in 1% formaldehyde before analysed by FCM. The gating was conventionally based on CD45FITC and CD14PE labelled mononuclear cells to separate the monocyte population from the lymphocyte population. A total of 10 000 cells in the lymphocyte gate were analysed for each surface marker. Absolute numbers of lymphocyte subpopulations were calculated from the complete lymphocyte blood count. Monocyte counts were drawn from routine leukocyte differential counts.
Preparation of tumour biopsies and immunohistochemistry
After excision, tumour biopsies were immediately stored in Tissue Tek® (Sakura Finetek Europe B.V, The Netherlands) and snap frozen in n-Hexane. Vials were stored at −70°C until analysis. Cryosections (6 µm) were prepared on a Micron HM 500M cryotome. After drying at room temperature for one hour, the sections were frozen two by two in 50 ml Nunc tubes at −20°C. Before staining, tubes were thawed for 30 min at room temperature before fixed in 100% acetone for 10 min. The staining procedure was performed using a 3-layer technique (primary antibody, biotin conjugated secondary antibody, HRP-sABC) developed with DAB and counterstained with Mayer′s hematoxylin. Tissue sections were incubated with the primary antibody for one hour, washed and incubated for 45 min with biotin conjugated secondary antibody (Biotin-rabbit-anti-mouse IgG, Jackson 315-066-045). After washing, HRP-sABC (DAKO, K0377) was added for 30 min. Thereafter, the tissue sections were washed and incubated with DAB for 5–15 min. Finally, the samples were counterstained with Mayer′s hematoxylin for 5 min and mounted using Aquamount (BDH, Kebo Lab). Isotype controls were performed for all antibodies as well as negative controls for all layers included. Anti-Melan-A (IgG1, M7196, DAKO) antibody staining was applied to identify the tumour areas. For identification of leukocyte subsets, the following MoAbs were used: anti-CD4 (IgG1, M0716, DAKO), anti-CD8 (IgG1, DAKO, M0707), anti-CD57 (IgM, Pharmingen, 555618) and anti-CD64 (IgG1, Pharmingen 555525). In tumour biopsies, CD57 was used instead of CD56 as a marker of NK cells because melanoma cells can express CD56 Citation[8]. As negative controls, the following antibodies were used: IgG1 (Pharmingen, 33811A/555746), IgM (DAKO, X 0942). Titration of the antibodies was performed on normal lymph node and spleen tissue and optimal concentrations used throughout the study.
Measurement of intra-tumoral immune cells
A stereological examination was performed using a morphometric system consisting of an Olympus BH-2 microscope with a motorized stage, controlled by a computer for manual interactive counting on the computer screen Citation[9]. The software used was CAST-GRID v 2.0, developed by Olympus, Denmark. Each microscopic field of vision was projected onto the computer screen with a video camera, and the computer generated an unbiased counting frame, in which the measurements were performed. On the projected image of the section, the tumour area was encircled on basis of the Melan-A staining when possible. In the present study, no analyses were performed with special emphasis on infiltration in and around necrotic areas. The field of vision was chosen at random and the computer then systematically sampled fields of vision within the entire encircled area. A minimum number of 85 fields (85–104) were counted for each sample. Only cells with staining restricted to the plasma membrane, a visible nucleus and located within the counting frame were counted as positive. The diameter of the cells in question was used to determine the number of positive cells per volume tumour (mm−3) for each patient.
Statistics
Absolute cell counts in blood and biopsies were compared using the Mann-Whitney test with the clinical outcome dichotomised as response (complete response and partial response) vs no response (no change and progression). The Mann-Whitney U statistic divided by the product of the number of patients in the two groups is presented i.e. estimating the probability that the first value is less than the second in randomly selected pairs. All p-values are two sided. Univariate and multivariate Cox analyses were performed to investigate the prognostic value of the variables in relation to survival. Hazards ratios were calculated to estimate the magnitude and the direction of the effect. Survival was defined as the interval from the day of treatment start to the end point (death or censoring). The simultaneous relationship of multiple prognostic factors for survival was assessed with Cox's proportional hazards model using the enter method. Variables with a p-value less than 0.10 were included in the Cox analyses to identify variables of independent significance. Included were cell counts in biopsies and blood dichotomised using the median as well as established prognostic factors such as WHO performance status, number of metastatic sites and serum lactate dehydrogenase (LDH). Because of multiple testing, the p-values for the univariate analyses have to be considered descriptive. All data on duration of survival were updated as of April 1st 2005. Calculations were performed using SPSS statistical software, v 11.5.
Results
Clinical outcome and sampling
A total of 27 patients were evaluable for response and survival. Patient characteristics are given in . Three patients achieved complete remission (CR), 6 patients achieved partial remission (PR), 5 patients achieved stable disease (SD), and 13 patients had progressive disease (PD). The median survival was 8.9 months (range 1–35 months). A total of 23 blood samples and 27 biopsies from the included 27 patients were analysed for the present study. There were only CD64 results from 25 patients; the remaining biopsy material after staining for the other markers was too poor (necrosis) to perform any further staining.
Table I. Patient characteristics.
Leukocyte subsets in peripheral blood and tumour in relation to overall response
Baseline leukocyte subsets in peripheral blood were quantified by flow cytometry. When comparing counts of CD4+ (helper T cells), CD8+ (cytotoxic T cells), CD56+ (NK) cells and monocytes no significant differences were seen between responding and non-responding patients ().
Table II. Leukocyte subpopulations in blood in relation to overall response.
The number of leukocyte subsets infiltrating the tumour CD4+, CD8+, CD57+ (NK) cells and CD64+ macrophages were quantified by immunohistochemistry. In responding patients, CD4+ were most numerous followed by CD8+, CD64+, and CD57+ (). In contrast, biopsies from non-responding patients were predominately infiltrated by CD64 + cells followed by CD8+, CD4+ and CD57+ cells (). A high number of infiltrating CD64 cells () was shown to be associated with poor response (p = 0.007) with an estimated probability of 84% that a random count in the responder group was less than a random count in the non-responder group ().
Figure 1. Immunohistochemical staining of CD64 + tumor-associated macrophages in a non-responding patient. Tumor-associated macrophages (black arrow) and tumor cells (white arrow).
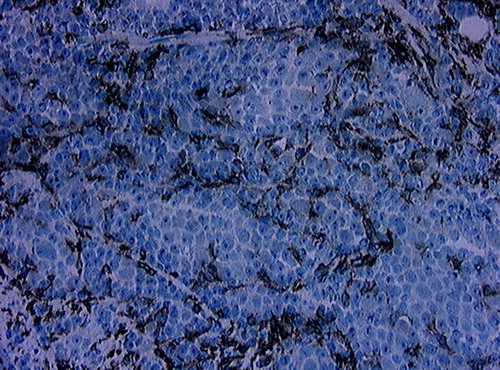
Table III. Leukocyte subpopulations in tumour biopsies in relation to overall response.
Leukocyte subsets in peripheral blood and tumour in relation to overall survival
Univariate analyses for overall survival identified a performance status of 2, a high number of metastatic sites, and an elevated serum LDH level as prognostic factors for poor survival. In the multivariate analysis, a performance status of 2 (p = 0.02) and a high number of metastatic sites (p = 0.004) were independent prognostic factors for poor survival ().
Table IV. Univariate and multivariate analyses of potential prognostic factors for overall survival.
Discussion
Various important functions of the immune system are modulated by IL-2, which plays a pivotal role in the regulation of lymphocyte activation and proliferation Citation[10], Citation[11]. Interleukin-2 also increases the lytic activity of NK cells and cytotoxic T lymphocytes Citation[12]. It is, thus, reasonable to assume that the therapeutic efficacy at least in part depends on the presence of certain immune cells in peripheral blood and metastases before treatment is initiated. As T lymphocytes, NK cells and macrophages have been associated with the efficacy of IL-2 Citation[13], Citation[14], the presence of these subsets of cells have been analysed in the present study.
In the present study, we have employed the anti-CD64 antibody as a marker of tumour-associated macrophages (TAMs), identifying the high affinity FcγRI constitutively expressed on the surface of monocytes/macrophages. This is in contrast to most other studies in which detection of the intracellular glycoprotein CD68 has been applied Citation[15]. The CD68 glycoprotein is a member of a family of acidic, highly glycosylated, lysosomal proteins implicated in antigen processing and expressed in macrophages, monocytes, neutrophils, basophils and dendritic cells Citation[16], Citation[17]. As CD64 seems more restricted, primarily expressed by monocytes/macrophages and some dendritic cells, and staining for CD64 was possible on cryosections, this antibody was chosen for the present study. In order to evaluate the possible staining of neutrophils by the CD64 antibody, comparisons to staining by CD66b, an antibody detecting a glycosylphosphatidylinositol (GPI) linked protein expressed on granulocytes, were performed. We observed no CD64 positive cells that also were CD66b positive, thus, CD64 did not stain granulocytes.
Our study showed that the metastases were predominately infiltrated by macrophages, followed by T cells and NK cells. These results are in agreement with findings by other groups Citation[5], Citation[18]. Interestingly, our results demonstrate that a high number of TAMs were negatively associated with clinical response to IL-2 based immunotherapy. An association between high numbers of TAMs and poor prognosis have been reported in a variety of human cancer types except melanoma Citation[15].
Tumour-associated macrophages have various and mutually opposite functions, depending on their activation state and the intrinsic properties of the tumour cells Citation[15], Citation[19]. They have been shown to play a key role in tumour angiogenesis, which ultimately modulates the tumour growth and invasion Citation[19–22]. Moreover, TAMs have been reported to produce angiogenic factors, such as vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), tumour necrosis factor (TNF) and IL-8 Citation[23], Citation[24]. In contrast to these pro-tumour properties, TAMs may also be directly tumoricidal and stimulate the anti-tumour properties of T cells Citation[15], Citation[19].
Our findings that the level of macrophage infiltration was significantly associated with progression may indicate that the macrophage population has tumour promoting and/or immune suppressing functions in metastatic melanoma. These results are in accordance with findings where macrophage infiltration has been correlated with tumour stage and angiogenesis in malignant melanoma Citation[22]. Furthermore, increased serum concentrations of angiogenic factors have been found to correlate with tumour progression and poor survival in malignant melanoma Citation[25]. Thus, our results may reflect a production of angiogenic factors from TAMs. Further studies will have to be performed in order to investigate this possibility. In our study there was no significant impact on survival of TAMs. The prognostic role of CD64 infiltration in tumour biopsies with regard to overall survival was analysed with univariate Cox analysis yielding a hazard ratio (HR) of 0.7. However, the 95% confidence interval was not statistically significant. As CD64 was dichotomised as counts below the median vs. counts above the median, the HR of 0.7 implies a better survival for a count below the median. This question has to be addressed in a larger study.
In conclusion, the present study suggests that tumour-associated macrophages may correlate negatively with the clinical outcome in patients with metastatic melanoma undergoing IL-2 based immunotherapy. However, these data should be validated in an independent study.
The Danish Cancer Society, “Max and Inger Woerzners mindelegat”, “Lægeforeningens forskningsfond”, “Sigvald og Edith Rasmussen født Poulsen” supported this study. The authors wish to thank Anni Skovbo and Eva Lykke Petersen for excellent technical assistance, Dr. Jens Randell Nyengaard for helpful guidance with the Cast-Grid system, Ib Jarle Christensen for help with the statistics, and the members of the department of Oncology for their careful management of the patients.
References
- Atkins MB, Kunkel L, Sznol M, Rosenberg SA. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J Sci Am 2000; 6(Suppl 1)S11–S14
- Rosenberg SA. Progress in human tumour immunology and immunotherapy. Nature 2001; 411: 380–4
- Engelhardt M, Wirth K, Mertelsmann R, Lindemann A, Brennscheidt U. Clinical and immunomodulatory effects of repetitive 2-day cycles of high-dose continuous infusion IL-2. Eur J Cancer 1997; 33: 1050–4
- Konjevic G, Jovic V, Jurisic V, Radulovic S, Jelic S, Spuzic I. IL-2-mediated augmentation of NK-cell activity and activation antigen expression on NK- and T-cell subsets in patients with metastatic melanoma treated with interferon-alpha and DTIC. Clin Exp Metastasis 2003; 20: 647–55
- Rubin JT, Elwood LJ, Rosenberg SA, Lotze MT. Immunohistochemical correlates of response to recombinant interleukin-2- based immunotherapy in humans. Cancer Res 1989; 49: 7086–92
- Schmidt H, Geertsen PF, Fode K, Rytter C, Bastholt L, von der Maase H. Subcutaneous interleukin-2 and interferon-alpha plus cisplatin with and without prophylactic cimetidine in patients with metastatic malignant melanoma: a phase II study. Melanoma Res 2000; 10: 66–77
- Schmidt H, Larsen S, Bastholt L, Fode K, Rytter C, von der Maase H. A phase II study of outpatient subcutaneous histamine dihydrochloride, interleukin-2 and interferon-alpha in patients with metastatic melanoma. Ann Oncol 2002; 13: 1919–24
- Anastassiou G, Schilling H, Stang A, Djakovic S, Heiligenhaus A, Bornfeld N. Expression of the cell adhesion molecules ICAM-1, VCAM-1 and NCAM in uveal melanoma: A clinicopathological study. Oncology 2000; 58: 83–8
- Gundersen HJ, Bendtsen TF, Korbo L, Marcussen N, Moller A, Nielsen K, et al. Some new, simple and efficient stereological methods and their use in pathological research and diagnosis. APMIS 1988; 96: 379–94
- Strausser JL, Rosenberg SA. In vitro growth of cytotoxic human lymphocytes. I. Growth of cells sensitized in vitro to alloantigens. J Immunol 1978; 121: 1491–5
- Trinchieri G, Matsumoto-Kobayashi M, Clark SC, Seehra J, London L, Perussia B. Response of resting human peripheral blood natural killer cells to interleukin 2. J Exp Med 1984; 160: 1147–69
- Lotze MT, Grimm EA, Mazumder A, Strausser JL, Rosenberg SA. Lysis of fresh and cultured autologous tumor by human lymphocytes cultured in T–cell growth factor. Cancer Res 1981; 41: 4420–5
- Panelli MC, Wang E, Phan G, Puhlmann M, Miller L, Ohnmacht GA, et al. Gene-expression profiling of the response of peripheral blood mononuclear cells and melanoma metastases to systemic IL-2 administration. Genome Biol 2002; 3: RESEARCH0035
- Donskov F, Bennedsgaard KM, von der MH, Marcussen N, Fisker R, Jensen JJ, et al. Intratumoural and peripheral blood lymphocyte subsets in patients with metastatic renal cell carcinoma undergoing interleukin-2 based immunotherapy: association to objective response and survival. Br J Cancer 2002; 87: 194–201
- Bingle L, Brown NJ, Lewis CE. The role of tumour-associated macrophages in tumour progression: Implications for new anticancer therapies. J Pathol 2002; 196: 254–65
- Baldus SE, Zirbes TK, Weidner IC, Flucke U, Dittmar E, Thiele J, et al. Comparative quantitative analysis of macrophage populations defined by CD68 and carbohydrate antigens in normal and pathologically altered human liver tissue. Anal Cell Pathol 1998; 16: 141–50
- Fukuda M. Lysosomal membrane glycoproteins. Structure, biosynthesis, and intracellular trafficking. J Biol Chem 1991; 266: 21327–30
- Hernberg M, Turunen JP, Muhonen T, Pyrhonen S. Tumor-infiltrating lymphocytes in patients with metastatic melanoma receiving chemoimmunotherapy. J Immunother 1997; 20: 488–95
- Pollard JW. Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer 2004; 4: 71–8
- Leek RD, Lewis CE, Whitehouse R, Greenall M, Clarke J, Harris AL. Association of macrophage infiltration with angiogenesis and prognosis in invasive breast carcinoma. Cancer Res 1996; 56: 4625–9
- Takanami I, Takeuchi K, Kodaira S. Tumor-associated macrophage infiltration in pulmonary adenocarcinoma: association with angiogenesis and poor prognosis. Oncology 1999; 57: 138–42
- Torisu H, Ono M, Kiryu H, Furue M, Ohmoto Y, Nakayama J, et al. Macrophage infiltration correlates with tumor stage and angiogenesis in human malignant melanoma: Possible involvement of TNFalpha and IL-1alpha. Int J Cancer 2000; 85: 182–8
- Boudreau N, Myers C. Breast cancer-induced angiogenesis: Multiple mechanisms and the role of the microenvironment. Breast Cancer Res 2003; 5: 140–6
- Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature 2000; 407: 249–57
- Ugurel S, Rappl G, Tilgen W, Reinhold U. Increased serum concentration of angiogenic factors in malignant melanoma patients correlates with tumor progression and survival. J Clin Oncol 2001; 19: 577–83
