To the Editor
As presented in the review-article by us, elsewhere in this issue Citation[1], combination chemotherapy in the treatment of advanced pancreatic carcinoma (APC) has proven disappointing. Illustrated by these case-reports we show, however, that individual patients can benefit well from existing combination chemotherapies and even be reassessed for radical surgery.
Little is, however, known concerning the long-term prognosis for patients with tumors, which respond well to chemotherapy and can be resected. A few reports have been published on good responders to chemoradiation who subsequently have undergone radical surgery Citation[2–5]. The results of the latter phase II trials suggest that the long-term survival may be better than for primarily resectable cases that have undergone direct surgery.
Case report 1
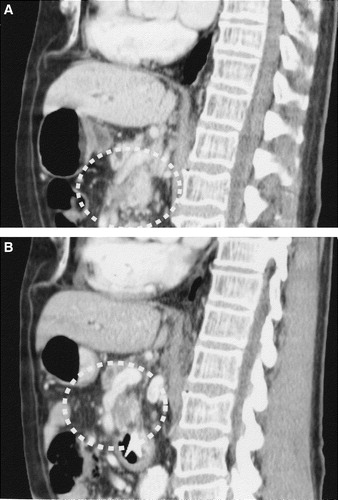
A 50-year-old woman presented with epigastrial pain following intake of fatty meals. The symptoms had been present for more than one year. An ultrasonography showed a dilated common bile duct but no signs of gallstones. The patient complained of increasing symptoms. Liver function tests showed a slightly increased level of plasma amylases but were otherwise normal. An abdominal CT scan was performed (A) which showed a 28×24 mm expansion in the head of pancreas and a greatly dilated pancreatic duct. The expansion also involved the portal vein at the level of the confluence of the splenic vein and the superior mesenteric vein. There were no signs of distant metastases within the abdomen. The expansion was biopsied percutaneosly using ultrasound. Histological examination showed PC.
Figure 1. (A) An abdominal CT scan performed before chemotherapy demonstrating a 28×24 mm tumour in the head of pancreas. (B) Abdominal CT scan after 3 months of chemotherapy showing a markedly decreased tumour.

Due to the vascular involvement the tumour was judged as inoperable. The patient was referred to our Oncological Department for palliative chemotherapy. The tumour marker CA 19-9 before chemotherapy was 53 kE/L (ref <35 kE/L). The patient received 3 months of chemotherapy in the form of FLG (bolus 5-Fu at a dose of 500 mg/m2, leucovorin 60 mg/m2 and gemcitabine 1000 mg/m2, at d1, 8 and 15 of a 28-day cycle).
A follow up CT scan after 3 months of treatment (B) showed that the expansion in the head of pancreas had decreased significantly, and most importantly; there were no longer any signs of involvement of the portal vein. As before there were no signs of distant metastases. The absence of vascular involvement following chemotherapy treatment was verified using magnetic resonance angiography. The patient was referred to the Surgical Department and reconsidered for radical surgery. The tumour was removed ad modum Whipple Citation[6]. Histological analysis revealed small remains of adenocarcinoma within the head of pancreas. All margins were free of tumour. The postoperative level of CA 19-9 was 27 kE/L. The patient was treated with another 3 months of FLG postoperatively and is currently disease free (10 months post surgery).
Case report 2
A 74-year-old man presented with obstructive jaundice. An abdominal CT scan was performed (A) which showed a 45×40 mm expansion in the head of pancreas. The expansion involved the superior mesenteric vein. There were no signs of distant metastases within the abdomen. The expansion was biopsied percutaneosly using ultrasound. Histological examination showed PC. Because of the vascular involvement the tumour was judged as inoperable.
Figure 2. (A) An abdominal CT scan performed before chemotherapy showing a tumour in the head of pancreas involving the superior mesenteric vein. (B) An abdominal CT after 3 months of chemotherapy demonstrating a decreased tumour. The superior mesenteric vein is no longer occluded.
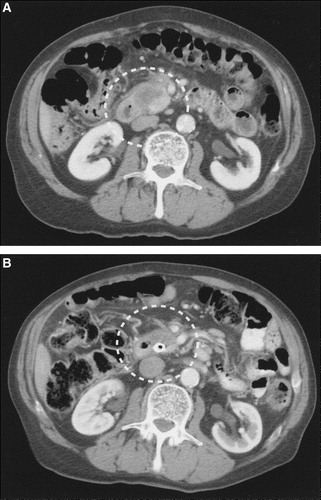
As in the previous case, the patient was referred to our Oncological Department for palliative chemotherapy. Before chemotherapy, the tumour marker CA 19-9 was 14 669 kE/L. The patient received 3 months of chemotherapy in the form of FLG. A follow-up CT scan after 3 months of treatment showed that the tumour had markedly decreased with a largest diameter of about 30 mm and no longer involved the superior mesenteric vein (B). CA 19-9 now measured 400 kE/L. A and B shows sagital CT slice depicting the occluded superior mesenteric vein before chemotherapy and improvement in patency after 3 months of treatment. The patient was referred to the Surgical Department and was further reassessed for radical surgery. An abdominal MRI was performed and the decrease of the size of the primary tumour and the vessel involvement was corroborated. However, according to this modality, liver metastases were suspected and the patient was, thus, not suitable for resection of the primary tumour despite the good local response to FLG-therapy.
Discussion
Involvement of crucial blood vessels is the major obstacle for radical surgery in locally advanced PC and deems many patients for palliative chemotherapy only. Several treatments for locally advanced PC, including chemoradiation, which aims to make patients candidates for radical surgery, are under evaluation Citation[7–9].
Although no combination chemotherapy has proven superior to single agent gemcitabine in terms of overall survival in the treatment of advanced PC, several trials suggest better outcome in other endpoints such as PFS, in favor of the combination regimens. This may point to an initial superior activity in favor of combination chemotherapy that could be made use of in a preoperative setting.
Until recently, metastatic and locally advanced PC was treated in the same way for palliation. This is, however, no longer the case. Some trials of palliative systemic treatment exclude locally advanced PC because of the lack of measurable disease and difficulties in assessing tumor response to therapy (e.g. the AVITA-study). This raises the question whether patients with locally advanced PC should be treated as potentially resectable i.e. with chemoradiation or as palliative i.e. with chemotherapy only. In our department patients with locally advanced PC that are judged to be candidates for radical resection after downstaging are treated with radiochemotherapy prior to surgery. Patients who are not candidates for radical surgery, e.g. tumor involvement of the coeliac axis, complete occlusion of the superior mesenteric vein/vena portae, or major arteries, are treated with chemotherapy only or in some cases with initial palliative stereotactic radiotherapy.
As described in the review article Citation[1], the use of target therapies in the treatment of pancreatic carcinoma may prove to be the best hope in the future, and will then no doubt find its way in to the neoadjuvant setting as well.
As more patients with APC are treated with palliative chemotherapy the question of reassessment for radical surgery will be increasingly relevant. This stresses the importance of frequent high quality radiographic evaluation and a close communication with the surgeons and radiologists of the multidisciplinary team.
References
- Lideståhl, A, Permert, J, Linder, S, Bylund, H, Edsborg, N, Lind, P. Efficacy of systemic therapy in advanced pancreatic carcinoma. Acta Oncol 2005; in press.
- White RR, Hurwitz HI, Morse MA. Neoadjuvant chemoradiation for localized adenocarcinoma of the pancreas. Ann Surg Oncol 2001; 8(10)758–65
- White RR, Tyler DS. Neoadjuvant therapy for pancreatic cancer: The Duke experience. Surg Oncol Clin N Am 2004; 13(4)675–84, ix–x
- Wanebo HJ, Glicksman AS, Vezeridis MP, Clark J, Tibbetts L, Koness RJ, et al. Preoperative chemotherapy, radiotherapy, and surgical resection of locally advanced pancreatic cancer. Arch Surg 2000; 135(1)81–7; discussion 88
- Snady H, Bruckner H, Cooperman A, Paradiso J, Kiefer L. Survival advantage of combined chemoradiotherapy compared with resection as the initial treatment of patients with regional pancreatic carcinoma. An outcomes trial. Cancer 2000; 89(2)314–27
- Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P, Pasquali C, et al. Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: A multicenter, prospective, randomized study. Lymphadenectomy Study Group. Ann Surg 1998; 228(4)508–17
- Oya N. Chemoradiotherapy for pancreatic cancer: Current status and perspectives. Int J Clin Oncol 2004; 9(6)451–7
- Pasetto LM, Jirillo A, Stefani M, Monfardini S. Is there a role for chemoradiotherapy in the treatment of pancreatic carcinoma?. Anticancer Res 2003; 23(3C)2805–13
- Fung MC, Ishiguro H, Takayama S, Moriazane T, Adachi S, Sakata T. Survival benefit of chemotherapy treatment in advanced pancreatic cancer: A metaanalysis. Proc Am Soc Clin Oncol 2003; 22: 288 (abstract 1155)