Abstract
T-cell large granular lymphocyte leukemia (T-LGL) also known as T-cell chronic lymphocytic leukemia is rare and comprises a small minority of all small lymphocytic leukemias. The concomitant presentation of T-LGL with acute myeloid leukemia (AML) has not been previously reported. We present an elderly gentleman with concomitant T-LGL and AML (non-M3) diagnosed by a combination of morphologic evaluation, immunophenotyping by flow cytometry, and T-cell gene rearrangement studies. The patient was managed with combination AML chemotherapy. He remains alive and well seven months after initial diagnosis. A brief review of literature is also presented.
T-cell large granular lymphocyte leukemia (T-LGL) or chronic lymphocytic leukemia (T-cell SLL/CLL) represents only 2–3% of all CLL patients, the remainder of which are of B-cell lineage Citation[1]. Second malignancies are frequently observed in the later group (B-cell SLL/CLL), the most common and frequent event is transformation to a large B-cell non-Hodgkin's lymphoma, the so-called Richter's syndrome Citation[2]. Progression to a more aggressive course is occasionally seen in patients with T-LGL. Concomitant presentation of acute myeloid leukemia (AML) and SLL/CLL is extremely rare and all reported cases have been of the B-cell type Citation[3–13]. We describe a case of concomitant presentation of AML with T-cell LGL.
Case Description
An 80-year-old white male presented with complaints of fatigue. His past medical history was significant for hypertension and B-12 deficiency. According to the patient, he had been diagnosed with colon cancer in the remote past, which had been treated with segmental colectomy. Physical examination was unremarkable for any lymphadenopathy or hepatosplenomegaly. A complete blood count revealed the following: Hemoglobin, 10.5 g/dl; total leukocyte count, 2.9×103/µl; absolute neutrophil count, 1.5×103/µl; and platelet count, 54×103/µl. Review of a peripheral blood smear revealed an absolute lymphocytosis with mature appearing lymphocytes. The β2 microglobulin levels were elevated at 4.83 mg/l (normal, <1.85 mg/l) and creatinine levels were 1.6 mg/dl; the rest of the laboratory examination was within normal range, included hepatic enzymes, lactate dehydrogenase levels, electrolytes, and vitamin B-12 levels (the patient was on injectable B-12 therapy). A computed tomography scan (CT scan) of the chest and abdomen ruled out any mediastinal or intraabdominal lymphadenopathy or hepatosplenomegaly.
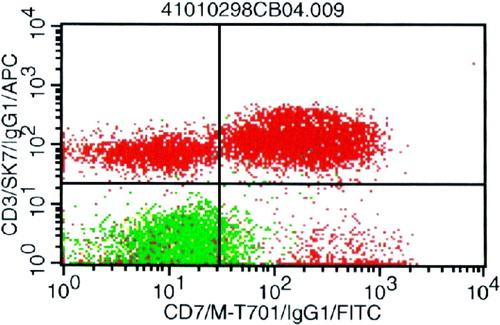
A bone marrow aspirate and biopsy revealed many lymphoid cells with moderate cytoplasm and prominent granules (large granular lymphocytes/ LGL). Immunophenotyping of the bone marrow aspirate by flow cytometric analysis revealed an abnormal monoclonal population of T-cells comprising approximately 22% of cells (). Also identified were an increased number of CD34 positive blasts co-expressing CD117 comprising 26.3% of total cellularity, consistent with acute myelogenous leukemia (AML, WHO classification, ). The CD4/CD8 ratio was decreased, estimated at 0.64. The subset of CD56 positive T-cells with down regulated CD7 and moderate CD3 and CD8 was suggestive of large granular lymphocytic leukemia (). Cytogenetic analysis of the bone marrow revealed a normal male karyotype (46, XY). These results were followed by a polymerase chain reaction (PCR) analysis of the bone marrow, which was positive for clonal T-cell receptor (TCR) gamma gene rearrangement, further evidence in support of a T-cell LGL.
Figure 2. A second population of neoplastic cells in the same sample express the myeloid antigen CD34.
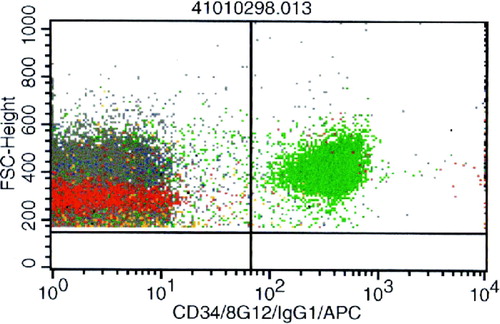
Table I. Immunophenotyping results of bone marrow aspirate (flow cytometry).
The patient was initiated with cytosine arabinoside and daunorubicin based chemotherapy. After the first cycle of chemotherapy, a bone marrow evaluation by flow cytometry showed residual myeloid blasts (7.7% of total) and persistence of abnormal T-cells (28% of cells). He is presently on the drugs listed above and is alive and well seven months after initial diagnosis.
Discussion
A review of literature failed to reveal reports of concomitant AML and T-LGL. The simultaneous or sequential occurrence of CLL/SLL with AML or myelodysplastic syndromes (MDS) may represent either divergent differentiation of the same stem cell clone or two separate processes Citation[14]. It is presumed that the possible mechanism for development of AML in CLL/SLL patients includes immunodeficiency states, since patients with immunodeficiency states have higher incidence of neoplasia when compared to the general population Citation[10]. In most cases however, AML arises after chemotherapy or radiation therapy given to treat CLL/SLL. Treatment with alkylating agents, including chlorambucil and cyclophosphamide, may cause secondary leukemias by directly damaging DNA. Therapy related AML from prolonged exposure to alkylating agents usually develops after interval of 3–6 years, is associated with poor prognostic karyotypes, and is often preceded by a preleukemic phase Citation[15], Citation[16].
Chemotherapy of secondary AML or MDS is associated with poor results Citation[10], Citation[17], although, Mateu et al. report a case of simultaneous B-cell CLL and AML successfully treated with AML-specific induction chemotherapy Citation[6]. There is a general consensus that in secondary AML, chemotherapy specific for this leukemia should be proposed only for patients with favorable karyotypes, younger age, and good performance status Citation[10], Citation[17]. Our patient responded well to combination AML chemotherapy.
References
- Hoyer JD, Ross CW, Li CY, Witzig TE, Gascoyne RD, Dewald GW, et al. True T-cell chronic lymphocytic leukemia: A morphologic and immunophenotypic study of 25 cases. Blood 1995; 86: 1163–9
- Wiernik PH. Second neoplasms in patients with chronic lymphocytic leukemia. Curr Treat Options Oncol 2004; 5: 215–23
- Caballero MD, Gonzalez M, Canizo MC, Orfao A, Nieto MJ, San-Miguel JF. Concomitant chronic lymphocytic leukemia (CLL) and acute myeloid leukemia. Complete remission of CLL achieved with high dose cytosine arabinoside. Leukemia 1992; 6: 856–8
- Conlan MG, Mosher DF. Concomitant chronic lymphocytic leukemia, acute myeloid leukemia, and thrombosis with protein C deficiency. Case report and review of literature. Cancer 1989; 63: 1398–401
- Lima M, Porto B, Rodriguez M, Teixeira MA, Coutinho J, Ribeiro AC. Cytogenetic findings in a patient presenting simultaneously with chronic lymphocytic leukemia and acute myeloid leukemia. Cancer Genet Cytogenet 1996; 87: 38–40
- Mateu R, Bellido M, Suredo A, Gonzalez Y, Rubiol E, Aventin A. Comcomitant chronic lymphocytic leukemia and acute myeloid leukemia with an uncommon immunophenotype. Am J Hematol 1997; 56: 281–7
- Tamul KR, Meyers DC, Bentley SA, Folds JD. Two color flow cytometric analysis of concomitant acute myeloid leukemia and chronic lymphocytic leukemia. Cytometry 1994; 18: 30–4
- Gomez-Arbones J, Gallart MA, Mellado A, Marco V, Panades MJ, Macia JM. Concomitant diagnosis of acute myeloid leukemia(AML) and chronic lymphocytic leukemia (CLL). Importance of flow cytometry in the diagnosis of CLL without lymphocytosis accompanying AML. Eur J Haematol 1997; 59: 335–7
- Yenerel MN, Hatemi I, Keskin H. Concomitant chronic lymphocytic leukemia and acute myeloid leukemia diagnosed by two color flow cytometric analysis. Haematologica 1999; 84: 766–7
- Robak T. Second malignancies and Richter's syndrome in patients with chronic lymphocytic leukemia. Hematology 2004; 9: 387–400
- Stern N, Shemesh J, Ramot B. Chronic lymphatic leukemia terminating in acute myeloid leukemia: Review of literature. Cancer 1981; 47: 1849–51
- Wallis JP, Joyner MV. Acute myeloid leukemia developing in a patient with longstanding untreated chronic lymphocytic leukemia. Acta Haematol 1986; 75: 229–31
- Bracey AW, Maddox AM, Immken L, Hsu SM, Marks ME. Coexistence of myelodysplastic syndrome and untreated chronic lymphocytic leukemia with development of acute myeloid leukemia immediately after treatment of chronic lymphocytic leukemia. Am J Hematol 1989; 30: 174–80
- Lai R, Arber DA, Brynes RK, Chan O, Chang KL. Untreated chronic lymphocytic leukemia concurrent with or followed by acute myelogenous leukemia or myelodysplastic syndrome. A report of five cases and review of the literature. Am J Clin Pathol 1999; 111: 373–8
- Barresi GM, Albitar M, O'Brien S. Acute myeloid leukemia, inversion 16, occurring in a patient with chronic lymphocytic leukemia. Leuk Lymphoma 2000; 38: 621–5
- Morrison VA, Rai KR, Peterson BL, Kolitz JE, Elias L, Appelbaum FR. Therapy-related myeloid leukemias are observed in patients with chronic lymphocytic leukemias after treatment with fludarabine and chlorambucil: Results of an intergroup study, cancer and leukemia group B 9011. J Clin Oncol 2002; 20: 3878–84
- Visani G, Pagano L, Pulsoni A, Tosi P, Piccaluga PP, Pastano R. Chemotherapy of secondary leukemias. Leuk Lymphoma 2000; 37: 543–9