To the Editor
Gliomatosis Peritonei (GP) is the implantation of mature neuroglial tissues on the surfaces of visceral or parietal peritoneum. This condition is usually seen in patients with immature ovarian teratomas and rarely reported with mature teratoma. We report a unique case of an adolescent female with a Pouch of Douglas mass one year after the primary resection of the mature ovarian teratoma.
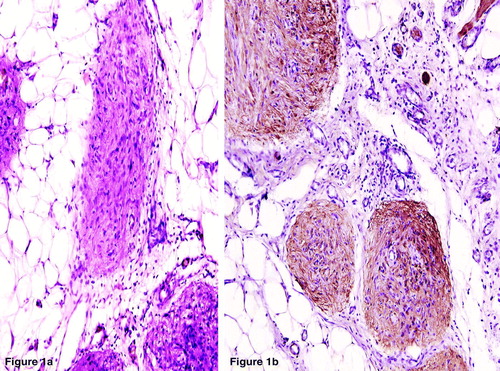
A 15-year-old female with abdominal pain and lump lower abdomen was operated for radiologically suspected right ovarian teratoma. Right salphingoophorectomy revealed features of a mature ovarian teratoma comprising of skin, adnexae, gut, respiratory epithelium and mature glial tissue and cartilage. Multiple sections showed no immature elements or primitive neuroectodermal tissues. The adnexal mass recurred in 4 months. Contrast enhanced CT scan revealed complex solid cystic mass in left lower abdomen and pelvis. Resections of this densely adherent mass revealed features as were seen in the previous tumor. One year following this, the patient presented with difficulty in defecation. At laprotomy, a firm irregular nodular, gray-white, growth measuring 3.2×2×1.5 cm in the rectovaginal septum and multiple small nodules measuring 0.3 to 1 cm on the uterine serosa, and omentum were seen. Biopsy of these nodules and partial omentectomy was done, microscopically; all revealed diffusely scattered Grade 0 mature astroglial tissue. (a) The glial fibrillary acidic protein (GFAP) immunostaining confirmed the nature of these elements. (b). The postoperative period was uneventful. No additional therapy was given. The patient is asymptomatic on follow-up.
Figure 1. a. The peritoneal implants and the omental deposits showing diffusely scattered Grade 0 mature astroglial tissues. (H&E×100). b. Positive Glial Fibrillary Acidic Protein (GFAP) immunostaining in the nodules confirming the glial nature. (LSAB×400).
Gliomatosis Peritonei (GP), a rare condition with benign glial implants on the peritoneal surface may be per operatively mistaken for peritoneal carcinomatosis or peritoneal tuberculosis Citation[1]. The mechanism of origin includes rupture and implantation from primary tumor or glial metaplasia of the pluripotent stem cells in the peritoneum Citation[2]. All grades of ovarian teratomas have been described, with immature teratomas being most commonly associated with GP. Stringent criteria for diagnosis of GP must be adhered to before labeling a case as Gliomatosis Peritonei (a) peritoneal surface, omentum, and diaphragmatic surfaces should be extensively sampled histologically and (b) each of the sampled implants should be composed exclusively, or almost exclusively, of Grade 0 glial tissue Citation[3]. This is extremely important because on extensive staging, if peritoneal sampling shows completely mature implants, a benign clinical course can be expected. In case no other teratomatous components or malignant glial tissue is identified, these should be ignored and therapy judged by the stage and grade of the primary ovarian teratoma only. However, if either of these is present, the treatment should be that of metastatic ovarian teratoma. GP is reported to impart an improved prognosis even in high-grade ovarian teratomas despite wide spread involvement of peritoneal surfaces Citation[4].
To conclude, GP is a rare condition that by and large imparts a favorable prognosis to patients with ovarian teratomas, especially mature teratoma. However, extensive sampling and microscopic search should always follow to exclude any immature or malignant component and the patient must remain on regular long-term follow-up.
References
- C.-Y. Chou, Y.-L. Chang, W.-F. Cheng, C.-A. Chen. Mature cystic teratoma with Gliomatosis Peritonei. Taiwan J Obstet Gynecol 2005 44:183–6.
- Thurlbeck WM, Scully RE. Solid teratoma of the ovary. A clinicopathological analysis of 9 cases. Cancer 1960; 13: 104–811
- Das CJ, Sharma R, Thulkar S, Mukhopadhyay S, Deka D, Mannan R. Mature ovarian teratoma with gliomatosis peritonei - A case report. Indian J Cancer 2005; 42: 165–7
- Muller AM, Sondgen D, Strunz R, Muller KM. Gliomatosis peritonei: A report of two cases and review of the literature. Eur J Obstet Gynecol Reprod Biol 2002; 100: 213–22
